Fig. 2. Incremental costs, QALYs and incremental cost-effectiveness ratios (ICER) resulting from previously-documented expanded access to HIV prevention programs and HIV testing and care interventions implemented at previously- documented scale of delivery in six U.S. cities.
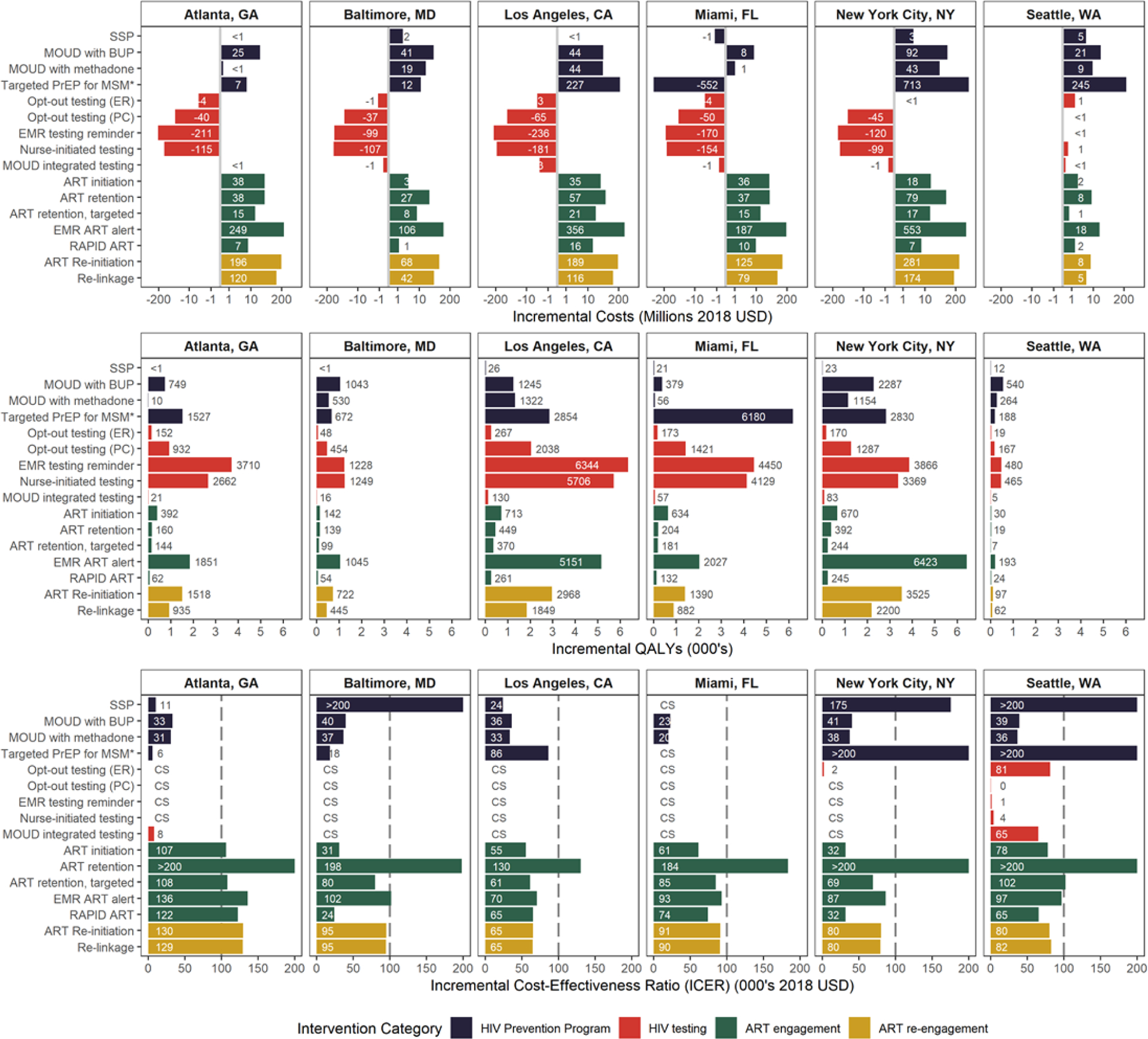
Results presented are for the 2020–2040 study period with expanded access to HIV prevention programs and implementation of HIV testing and care interventions sustained over a 10-year period (mean of the 2,000 run conducted in the probabilistic sensitivity analysis; 95% credible intervals are presented in Supplemental Table 8 http://links.lww.com/QAD/B592). The vertical gridline in the 3rd row indicates the $100,000/QALY threshold for interventions to be considered cost-effective. CS: Cost-saving; QALYs: quality-adjusted life-years; ART: Antiretroviral therapy; SSP: Syringe service program; PrEP: pre-exposure prophylaxis; MOUD: Medication for opioid use disorder; BUP: Buprenorphine; ER: Emergency Department; PC: Primary care; EMR: Electronic medical records; ART initiation: Case management intervention to increase ART initiation; ART retention: Care coordination to increase ART retention; EMR alert: EMR alert of suboptimal ART engagement.
* Targeted PrEP for high-risk men who have sex with men (MSM) and high-risk MSM who inject drugs (MWID).
