Abstract
Background
Lung transplantation has long been the accepted therapy for end-stage pulmonary fibrotic disease. Presently, there is an ongoing debate over whether single or bilateral transplantation is the most appropriate treatment for end-stage disease, with a paucity of high-quality evidence comparing the two approaches head-to-head.
Methods
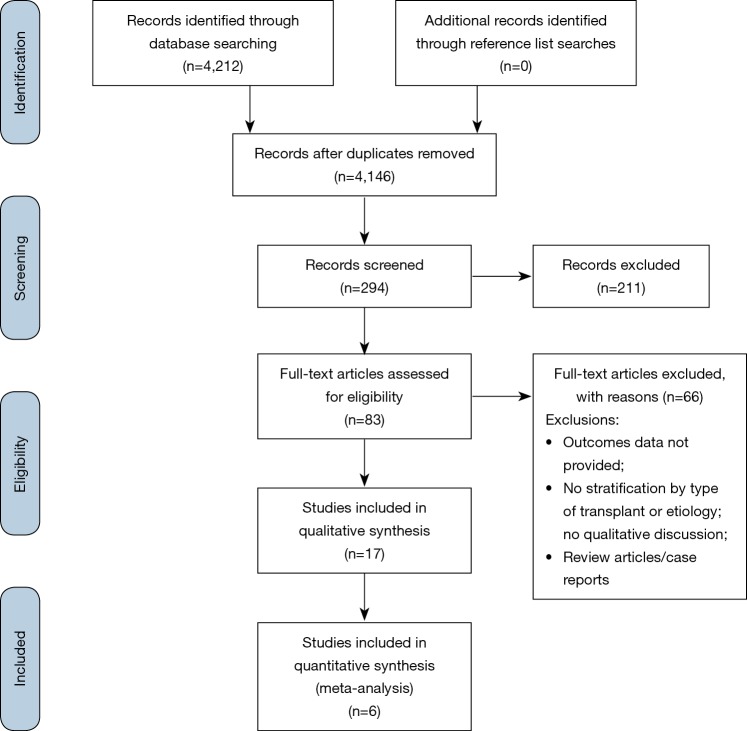
This review was performed in accordance with PRISMA recommendations and guidance. Searches were performed on PubMed Central, Scopus and Medline from dates of database inception to September 2019. For the assessed papers, data was extracted from the reviewed text, tables and figures, by two independent authors. Estimated survival was analyzed using the Kaplan-Meier method for studies where time-to-event data was provided.
Results
Overall, 4,212 unique records were identified from the literature search. Following initial screening and the addition of reference list findings, 83 full-text articles were assessed for eligibility, of which 17 were included in the final analysis, with a total of 5,601 patients. Kaplan-Meier survival analysis illustrated improved survival in patients receiving bilateral lung transplantation (BLTx) than in those receiving unilateral transplantation for idiopathic pulmonary fibrosis at all time intervals, with aggregated survival for BLTx at 57%, 35.3% and 24% at 5-, 10- and 15-year follow-up, respectively. Survival rates for SLTx were 50%, 27.8% and 13.9%, respectively.
Conclusions
Whilst a number of studies present conflicting results with respect to short-term transplantation outcomes, BLTx confers improved long-term survival over SLTx, with large-scale registries supporting findings from single- and multi-center studies. Through an aggregation of published survival data, this meta-analysis identified improved survival in patients receiving BLTx versus SLTx at all time intervals.
Keywords: Lung transplantation, fibrotic disease, outcomes
Introduction
Lung transplantation has long been an accepted therapy for end-stage pulmonary fibrotic disease given the poor long-term prognosis of patients managed with medical and conservative treatment (1). Presently, there is an ongoing debate over whether single (SLTx) or bilateral (BLTx) lung transplantation is the most appropriate treatment, with a paucity of high-quality evidence comparing the two approaches head-to-head (2). As such, practice is still largely specific to the institution or to the surgeon’s preference. Historically, SLTx has been used under the rationale that it is a more limited operation and hence is more appropriate for high-risk candidates; however, as surgical techniques have improved, bilateral transplantation—particularly with its increasingly acceptable long-term morbidity and mortality—has become predominant. Given the heterogeneity of interstitial lung diseases, particularly in terms of their etiology and pathophysiology, substantive subgroup analysis to date has been hindered outside of registry findings, with patient outcomes highly variable within the literature (3). The present systematic review will detail the mid- and late-term outcomes after SLTx vs. BLTx for pulmonary fibrotic disease and will provide an aggregation of the present data on survival outcomes.
Methods
Literature search
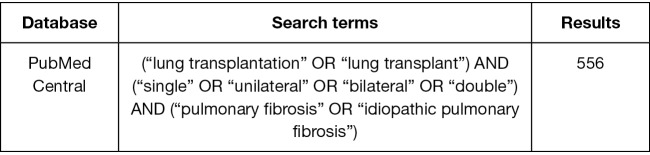
This review was performed in accordance with PRISMA recommendations and guidance (4,5). Electronic searches were performed on PubMed Central, Scopus and Medline from dates of database inception to September 2019, using the terms (“lung transplantation” OR “lung transplant”) AND (“single” OR “unilateral” OR “bilateral” OR “double”) AND (“pulmonary fibrosis” OR “idiopathic pulmonary fibrosis”) as either keywords or MeSH headings. After removal of duplicate records, studies were screened according to their titles and abstracts, then reviewed according to the inclusion and exclusion criteria detailed below by two independent authors (AR Wilson-Smith, YS Kim). Conflicts were resolved by the senior researcher (AR Wilson-Smith). A PRISMA diagram of the search strategy is presented in Figure S1. Additional references for discussion were obtained by reference list searches, or via targeted database searches.
Figure S1.
PRISMA flow chart detailing the literature search process for mid- to late-term outcomes of single vs. bilateral lung transplantation in the setting of pulmonary fibrosis.
Inclusion and exclusion criteria
Studies were eligible for this review if they had at least ten patients in their cohorts and where transplantation (either SLTx or BLTx) was indicated primarily for idiopathic pulmonary fibrosis (IPF). Follow-up of a minimum of one year was also required. Non-English records, review articles, conference and paper abstracts, editorials, letters, case reports, series, and opinions were excluded. Studies were excluded from analysis if they failed to delineate between SLTx and BLTx outcomes, or if no mention was made of the outcome between the two approaches qualitatively.
Studies which aggregated etiologies in their survival analysis (e.g., IPF + cystic fibrosis + chronic obstructive pulmonary disease) were excluded from quantitative analysis, as were emergent surgeries. Duplicate studies were removed prior to the commencement of the literature screen and only the most up-to-date references from ongoing studies or registries were reviewed for statistical aggregation to minimize patient overlap. Studies were also excluded if they did not present baseline patient characteristics, or if the study was centered on pediatric patients (i.e., those <18 years).
Data extraction, statistical analysis and presentation
For the assessed papers, data was extracted from the reviewed text, tables and figures. Data was extracted independently by two independent authors (AR Wilson-Smith, YS Kim) into Microsoft Excel. Discrepancies were reviewed and discussed until a consensus was reached. Findings are presented in Tables 1-3. Estimated survival was analyzed using the Kaplan-Meier method in studies where time-to-event data was provided (6). Censoring was assumed to be constant, unless the particular curve had a long follow-up of only minimal patients—in which case, censoring was manually entered. Death events and censoring data were compiled for the entire patient cohort and overall survival curves were produced using R Studio (7).
Table 1. Study characteristics and clinical outcomes.
| Study | Year | Institution | Country | Period | Type | Total patients | IPF patients | Stratify data by transplant indications | Stratify data by surgical type (SLTx vs. BLTx) | Stratify by transplant indication and surgery type | Study quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Algar | 2010 | Lung Transplantation Unit, Hospital Universitario Reina Sofia, University of Cordoba, Cordoba, Spain | Spain | October 1993–December 2009 | Single and bilateral | 301 | 89 | Yes | No | No | High |
| Burdett | 2012 | Freeman Hospital, Newcastle-upon-Tyne, United Kingdom | United Kingdom | 1987–2010 | Single | 259 | 108 | Yes | No | No | Moderate |
| Burton | 2005 | Hjertecentret, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark | Denmark | January 1992–December 2003 | Single and bilateral | 362 | N/A | No | Yes | No | High |
| De Oliveira | 2012 | Division of Cardiothoracic Surgery, Department of Surgery, University of Wisconsin Hospital and Clinics, Madison, WI, USA | USA | January 1993–March 2009 | Single and bilateral | 111 | 79 | Yes | Yes | Yes | High |
| De Perrot | 2004 | Toronto Lung Transplant Program, Toronto General Hospital, University of Toronto, Toronto, Ontario, Canada | Canada | 1983–2003 | Single and bilateral | 501 | 97 | Yes | Yes | No | High |
| Harringer | 1999 | Division of Thoracic and Cardiovascular Surgery, Hannover Medial School, 20623 Hannover, Germany | Germany | December 1987–September 1998 | Single and bilateral | 258 | 73 | Yes | Yes | No | High |
| Mason | 2007 | Departments of Thoracic and Cardiovascular Surgery, Quantitative Health Sciences, and Pulmonary, Allergy, and Critical Care Medicine, Cleveland Clinic, Cleveland, Ohio, USA | USA | February 1990–November 2005 | Single and bilateral | 469 | 82 | Yes | Yes | Yes | High |
| Meyers | 2000 | Divisions of Cardiothoracic Surgery and Pulmonary and Critical Care Medicine, Washington University School Medicine, St Louis, Mo, USA | USA | July 1988–July 1998 | Single and bilateral | 433 | 45 | Yes | Yes | Yes | High |
| Rubin | 2015 | Pavilhão Pereira Filho, Santa Casa de Porto Alegre; and at the Universidade Federal de Ciências da Saúde de Porto Alegre, Porto Alegre, Brasil | Brazil | January 2006–December 2012 | Single | 218 | 79 | Yes | N/A | N/A | Moderate |
| Smith | 2006 | Departments of Surgery, Public Health Sciences, and Internal Medicine, University of Virginia, Charlottesville, Virginia, USA | USA | 1995–2005 | Single and bilateral | 182 | 37 | Yes | No | No | High |
| Thabut | 2003 | Service de Pneumologie et Re´animation Respiratoire, a Service de Chirurgie Thoracique et Vasculaire, b and Service d’Anatomopathologie, Hoˆpital Beaujon, c Clichy, France | France | N/A | Single | 28 | 28 | Yes | N/A | N/A | High |
| Wei | 2019 | Transplant Center, The Affiliated Wuxi People’s Hospital of Nanjing Medical University, Jiangsu, China | China | January 2015–December 2017 | Single and bilateral | 109 | 109 | Yes | Yes | Yes | High |
| Kreisel | 2011 | Division of Cardiothoracic Surgery, a Department of Surgery, and The Division of Pulmonary and Critical Care Medicine Department of Medicine, Washington University in St Louis, Mo, USA | USA | July 1988–January 2009 | Single and bilateral | 1,000 | 161 | Yes | Yes | Yes | High |
| Schachna | 2006 | Johns Hopkins Hospital and the University of Pittsburgh Medical Center | USA | December 1989–June 2002 | Single and bilateral | 689 | 70 | Yes | No | No | High |
| Neurohr | 2010 | Ludwig-Maximilians University, Munich, Germany | Germany | 1997–2008 | Single and bilateral | 76 | 76 | Yes | Yes | Yes | High |
| Keating | 2009 | Lung Transplant Service, Allergy, Immunology and Respiratory Medicine, Alfred Hospital, Melbourne, Australia | Australia | 1990–2008 | Single and bilateral | 585 | 90 | Yes | Yes | Yes | High |
| Grossman | 1989 | Mount Sinai Hospital and the University of Toronto | Canada | November 1983–August 1989 | Single | 20 | 20 | Yes | N/A | N/A | High |
SLTx, single lung transplantation; BLTx, bilateral lung transplantation; N/A, not available.
Table 2. Single versus bilateral lung transplantation study characteristics.
| Study | De Oliveira et al., 2012 | Mason et al., 2007 | Meyers et al., 2000 | Wei et al., 2018 | Kreisel et al., 2011 | Rubin et al., 2015 | Thabut et al., 2003 | Neurohr et al., 2010 | Keating et al., 2009 | Grossman et al., 1989 |
|---|---|---|---|---|---|---|---|---|---|---|
| Total IPF patients | 79 | 82 | 45 | 109 | 161 | 44 | 28 | 76 | 90 | 20 |
| Males (%) | ||||||||||
| Single | 76.5 | 63.4 | 59 | 91.1 | – | 66 | 71.4 | 54.3 | 70 | 85 |
| Double | 70 | – | 54 | 96.7 | – | – | – | 60 | – | – |
| Age (years) | ||||||||||
| Single | 56.8±7.2 | 52±11 | 48.8±9.1 | 62.6±7.8 | – | 57 | 49.3 | 53.74±1.15 | 52 | 48.4 |
| Double | 43.4±12.3 | – | 52.9±8.7 | 53.7±9.3 | – | – | – | 50.38±1.34 | – | – |
| Transplant approach (n) | ||||||||||
| Single | 65 | 50 | 32 | 79 | – | 44 | 28 | 46 | 53 | 20 |
| Double | 14 | 32 | 13 | 30 | – | – | – | 30 | 37 | – |
| 1-year survival (mean) (%) | ||||||||||
| Single | 81.8 | 67 | 81 | 80.8 | – | 74 | 79.4 | 69.6 | 78 | 55 |
| Double | 73 | 81 | 77 | 66.7 | – | – | – | 79.5 | 68 | – |
| 3-year survival (mean) (%) | ||||||||||
| Single | 65.4 | 34 | 63 | 73.8 | – | – | 55.3 | 49 | – | |
| Double | 60.2 | 55 | 54 | 63.3 | – | – | 74.2 | 50 | – | |
| 5-year survival (mean) (%) | ||||||||||
| Single | 62.7 | – | 50 | – | 44.9 | 45 | 39 | 41.7 | 29 | – |
| Double | 53.5 | – | 38 | – | 58.9 | – | – | 66.8 | 50 | – |
| 10-year survival (mean) (%) | ||||||||||
| Single | 39 | – | – | – | 20.8 | 22 | – | – | – | – |
| Double | 42.8 | – | – | – | 36.7 | – | – | – | – | – |
Table 3. Reported mortality and morbidity.
| Study | Mortality | Additional factors | Comments | |
|---|---|---|---|---|
| SLTx | BLTx | |||
| Algar | – | – | – | BLTx conferred higher observed perioperative and 1-year mortality rates compared to SLTx |
| Burton | n=228. 30-day perioperative mortality (7.9%) and 90-day perioperative mortality (9.7%) | n=112. 30-day perioperative mortality (3.6%) and 90-day perioperative mortality (10.8%) | – | This was not stratified by indication |
| De Oliveira | 9.40% | 7.70% | Length of hospital stay (days): SLTx, 15 (IQR, 10–25); BLTx, 24 (IQR, 16–48) | P values: mortality difference, 0.46; length of hospital stay, <0.01; readmission, 0.94; length of ICU stay <0.01 |
| Readmission <30 days: SLTx, 21 (25.9%); BLTx, 8 (26.7%) | ||||
| Length of ICU stay: SLTx, 4 (IQR, 3–9); BLTx, 8 (IQR, 6–24) | ||||
| Mason | 30-day perioperative mortality (6%) | 30-day perioperative mortality (6%) | – | – |
| Meyers | In-hospital mortality 9.4% of 32 SLTx patients | In hospital mortality of 7.7% of 13 BLTx patients | Length of hospital stay (days): SLTx, 21 [13–32]; BLTx, 23 [15–39] | P values: difference in hospital mortality is not significant; length of hospital stay was 0.4; length of ICU stay 0.7; mechanical ventilation 0.5 |
| Intensive care unit stay (days): SLTx, 5 [3–10]; BLTx, 6 [4–12] | ||||
| Mechanical ventilation (days): SLTx, 3 [2–9]; BLTx, 4 [3–18] | ||||
| Wei | – | – | Post-operative ICU days (mean ± SD): SLTx, 5.8±6.3; BLTx, 4.6±2.8 P value for: post-op length of stay was 0.014; post-op ICU stay 0.551 |
30-day mortality was higher in BLTx but not statistically significant based on the Mantel Haenzel log rank test (P=0.131) |
| Post-operative length of stay in days (mean ± SD): 49.8±33.0; 33.1±25.2 | The difference in the number of complications including primary graft dysfunction, pulmonary bacterial infection, anastomotic complications, heart failure, arrhythmia, acute kidney injury and malignant tumour was not significant between SLTx vs. BLTx | |||
| Neurohr | – | – | – | Increased 90-day mortality in SLTx without difference reaching statistical significance (P=0.06) |
SLTx, single lung transplantation; BLTx, bilateral lung transplantation; IQR, interquartile range; ICU, intensive care unit; SD, standard deviation.
Quality assessment of included studies
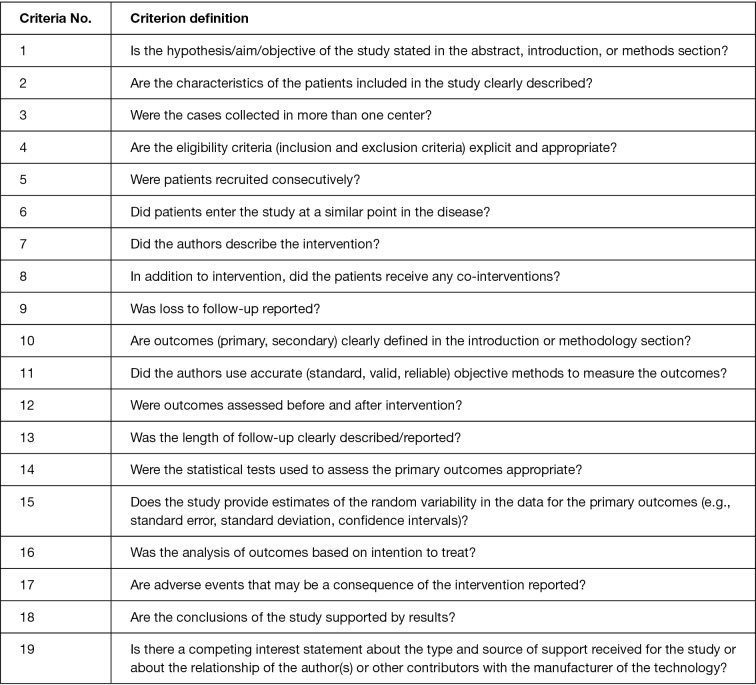
An appraisal schema based on the Canadian National Institute of Health Economics’ (CNIHE) Quality Assessment Tool (i.e., the modified Delphi technique) for case series studies was employed to evaluate all included studies (Figure S2). Studies were categorized based on the following domains: clarity of study objective, adequate description of the study population, description of the intervention, adequate reporting of outcome measures, appropriate reporting of results/conclusions (quality findings are listed in Table 1, criteria are provided in Figure S2). Studies were considered to be of high quality if they addressed at least 15 of the 19 criteria outlined in the CNIHE tool. Moderate quality was defined as 13–15 of 19 and low quality below 13 of 19.
Figure S2.
Quality appraisal criteria.
Results
Overall, 4,212 unique records were identified from the literature search (Figures S1,S3). Following initial screening and the addition of reference list findings, 83 full-text articles were assessed for their eligibility, of which 17 were included in the final analysis. Six studies were included in the quantitative synthesis (8-13). The search of 4,212 records yielded 17 studies which met inclusion criteria, with a total of 5,601 patients. The majority of studies (90%) were found to be of high quality according to the CNIHE tool, with the remainder as moderate quality. The majority of studies included in the final analysis were from European or United States centers, with the remainder being drawn from Asian, Canadian or Central American centers.
Figure S3.
Search strategy supplementary.
Survival—SLTx vs. BLTx
All curves digitized and aggregated in this study were unadjusted. Aggregated survival for SLTx at 5-, 10- and 15-year time intervals was 50%, 27.8% and 13.9%, respectively. Survival for BLTx was 57%, 35.3% and 24%, respectively (Figure 1).
Figure 1.
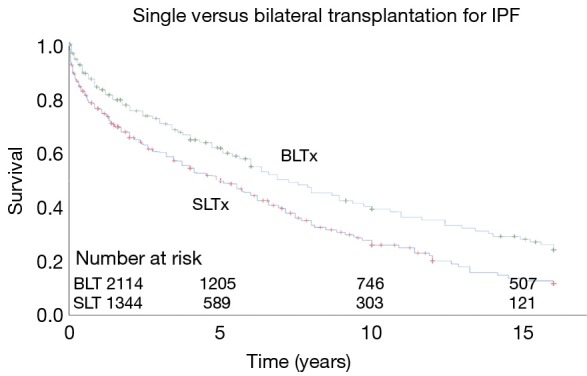
Kaplan-Meier survival analysis for single versus bilateral lung transplantation in IPF. IPF, idiopathic pulmonary fibrosis; BLTx, bilateral lung transplantation; SLTx, single lung transplantation.
Morbidity—SLTx vs. BLTx
Reported morbidity findings are detailed in Table 3. Three studies outlined morbidity data quantitatively (8,10,11). Length of hospital stay was statistically significant in two studies in favor of SLTx. Length of ICU stay was only significant in one study in favor of SLTx. All other reported complication rates were not statistically significant between the two surgical modalities.
Discussion
SLTx vs. BLTx: head-to-head studies
Out of the seven studies that present survival rates of BLTx vs. SLTx specifically for IPF patients, three of these studies establish improved survival in patients receiving SLTx. De Oliveira et al. demonstrate in 79 patients that survival is better in SLTx up to 5 years. The 1-, 3-, 5-year survival rates of SLTx vs. BLTx were 81.8% vs. 73%, 65.4% vs. 60.2%, 62.7% vs. 53.5% (P=0.68), respectively (8). The 10-year survival rate was 39% vs. 42.8%, respectively. Meyers et al. demonstrate survival rates of SLTx vs. BLTx being 81% vs. 77%, 63% vs. 54% and 50% vs. 38% for the 1-, 3- and 5-year endpoints (P=0.42) (10). These rates were established in 32 SLTx and 13 sequential BLTx; no difference in in-hospital mortality between SLTx (9.40%) and BLTx (7.70%) was noted.
The most recent single center study by Wei et al. (11) demonstrated survival rates in a cohort of 109 patients of 80.8% vs. 66.7% and 73.8% vs. 63.3% for SLTx vs. BLTx, at 1- and 2-year survival, respectively (P=0.13). When the survival rates of SLTx vs. BLTx in IPF patients are further stratified by age <60 and age >60, SLTx had significantly greater survival in the over-60 age-group (P=0.008).
The other studies align with the findings of the UNOS Registry and ISHLT registry, which outline that BLTx has improved survival for IPF patients over SLTx (14-22). In their cohort of 469 patients, 82 of which had IPF, Mason et al. found that patients receiving BLTx had better risk-unadjusted survival than those receiving SLTx, with 1-year survival at 81% and 67%, and 5-year survival at 55% and 34%, respectively. BLTx survival rates were similar to those for non-IPF indications (9). Following matched analysis, the benefit of BLTx over SLTx was not maintained, with perioperative mortality and short-term postoperative mortality both at 6% (10).
Neurohr et al. found a significant survival benefit of BLTx over SLTx in their cohort of 76 patients at 1-year and in overall survival (P=0.026) (13). Although SLTx had a higher percentage of acute rejection (35.6%) compared to BLTx (29.6%), this was not statistically significant; however, there was a significantly higher number of deaths in SLTx compared to BLTx as a result of the development of bronchiolitis obliterans. Kreisel et al. demonstrate a higher survival rate in BLTx for the 5- and 10-year mark (23). Interestingly, Kreisel extracted data from 1988 to 2009, including the data used in the Meyers et al. (10) study from the same institution (1988–1998); however, it appears that the data from the extended 10-year follow-up reversed the survival benefit that SLTx had over BLTx found by Meyers et al. (10) One reason for this finding may be improved surgical technique of BLTx within the last ten years, or alternatively, BLTx may in fact have improved long-term survival benefits after the initial convalescence period. Keating et al. (12) demonstrated a survival rate pattern similar to that of De Oliveira et al. (8) up to the 3-year mark, the survival rate was higher for SLTx compared to BLTx; however, at the 5-year mark, BLTx conferred a higher survival rate of 50% compared to SLTx at 29%.
Six studies outlined findings for IPF patients undergoing transplantation but did not stratify for surgical approach with quantitative analysis. For instance, Algar et al. found that survival did not differ between SLTx and BLTx at long-term follow-up, noting that whilst BLTx conferred increased mortality in the short-term, the long-term survival benefit offset the initial mortality (24). A number of studies compared SLTx and BLTx, but did not differentiate for etiology. de Perrot et al. (15) found in their cohort of 501 patients, long-term survival was higher in patients receiving BLTx vs. patients receiving SLTx (P=0.07); when separately analyzing for etiology (i.e., cystic fibrosis, chronic obstructive pulmonary disease, IPF, etc.) this effect disappeared; however, no data were presented in-text.
Database analysis of IPF patient outcomes
Villavicencio et al. (25) presents the most recent data comparing survival outcomes of SLTx vs. BLTx in IPF recipients. This study includes 9,191 lung transplant recipients with IPF from 1987 to 2015. They have demonstrated that BLTx has improved survival outcomes in IPF patients compared to SLTx across all lung allocation scores and additionally when adjusted for age, excepting those exceeding 70 years (P<0.001). The International Society for Heart and Lung Transplantation Registry (ISHLT) have collated the survival outcomes of SLTx vs. BLTx in IPF patients and presented their data on transplant recipients with IPF from January 1990 to June 2016. Kaplan-Meier curves were produced from 1,043 SLTx patients with IPF and 1,936 BLTx patients with IPF. BLTx was shown to have improved survival outcomes compared to SLTx at each year from the 1st year to the 16th year (P<0.0001).
Limitations
To the authors’ knowledge, this is the most recent and thorough systematic review of the literature comparing SLTx to BLTx in the context of IPF and the only review to incorporate an aggregation of survival data across single- and multi-center studies and registries.
However, are several limitations with respect to the present review. The number of single- and multi-center studies analyzing the survival outcomes of IPF patients with clear stratification of which patients received SLTx and BLTx was low, with only 17 studies meeting the final inclusion criteria. The majority of these studies provided survival outcomes of IPF recipients compared to other transplant recipients of varying indications, and/or survival outcomes comparing SLTx vs. BLTx in all transplant recipients. Only six studies—with one potentially replicated dataset—were able to stratify survival outcomes by SLTx vs. BLTx specifically for IPF patients.
The limited number of studies with survival outcomes and stratification between surgical approaches prevented meaningful quantitative analysis of the single- and multi-center studies, requiring an aggregation of the findings from large registries. It is likely that there is a degree of patient overlap, as patients within the registries would have been drawn from these single- and multi-center studies; however, using the methods of Sampson et al. who present techniques for identifying cohort overlap, this was mitigated as far as possible (26). Although registry studies are extremely useful (i.e., they benefit from large numbers that allow for sound statistical analysis), it is of note that they include and collate data from a wide array of centers, with surgeons of variable expertise, using different surgical protocols and incomplete patient data. Hence, in centers which have always preferred one technique over another become highly proficient in that technique; it would not be surprising to note outcomes that go against the findings from registry data.
The primary constraint of this review is that the single- and multi-center studies identified have often yielded conflicting results, with largely uninterpretable or sparsely reported data (from a meta-analytical perspective) supporting their recommendations; often, no differentiation is made between the indications for transplantation (e.g., cystic fibrosis, IPF, etc.) or which patients are receiving what type of intervention (i.e., SLTx or BLTx). Further, very limited morbidity data were reported, with only three studies comparing SLTx and BLTx for IPF providing quantitative results (Table 3). Often, authors would make comments in their discussions noting that one technique was more favorable in terms of survival or complications, but with no analysis to substantiate the claims.
In order to carry out definitive analysis, it is critical that patients with different pathologies are not grouped and vice versa for transplantation technique, as the level of heterogeneity strongly calls into question the validity of the findings. It is imperative that for future analysis of survival outcomes, clinicians and researchers provide datasets which have been stratified appropriately for etiology as well as for surgical approach.
Conclusions
Whilst a number of studies present conflicting results with respect to short-term transplantation outcomes, the consensus is that BLTx confers improved long-term survival over that of SLTx, with large-scale registries supporting the findings from single- and multi-center studies. Through an aggregation of the present survival data, this meta-analysis identified improved survival in patients receiving BLTx versus those receiving SLTx at all time intervals.
Acknowledgments
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Schaffer JM, Singh SK, Reitz BA, et al. Single- vs double-lung transplantation in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis since the implementation of lung allocation based on medical need. JAMA 2015;313:936-48. 10.1001/jama.2015.1175 [DOI] [PubMed] [Google Scholar]
- 2.Puri V, Patterson GA, Meyers BF. Single versus bilateral lung transplantation: do guidelines exist? Thorac Surg Clin 2015;25:47-54. 10.1016/j.thorsurg.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kistler KD, Nalysnyk L, Rotella P, et al. Lung transplantation in idiopathic pulmonary fibrosis: a systematic review of the literature. BMC Pulm Med 2014;14:139. 10.1186/1471-2466-14-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phan K, Tian DH, Cao C, et al. Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg 2015;4:112-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guyot P, Ades AE, Ouwens MJ, et al. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol 2012;12:9. 10.1186/1471-2288-12-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowther MJ, Riley RD, Staessen JA, et al. Individual patient data meta-analysis of survival data using Poisson regression models. BMC Med Res Methodol 2012;12:34. 10.1186/1471-2288-12-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Oliveira NC, Osaki S, Maloney J, et al. Lung transplant for interstitial lung disease: outcomes for single versus bilateral lung transplantation. Interact Cardiovasc Thorac Surg 2012;14:263-7. 10.1093/icvts/ivr085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mason DP, Brizzio ME, Alster JM, et al. Lung transplantation for idiopathic pulmonary fibrosis. Ann Thorac Surg 2007;84:1121-8. 10.1016/j.athoracsur.2007.04.096 [DOI] [PubMed] [Google Scholar]
- 10.Meyers BF, Lynch JP, Trulock EP, et al. Single versus bilateral lung transplantation for idiopathic pulmonary fibrosis: a ten-year institutional experience. J Thorac Cardiovasc Surg 2000;120:99-107. 10.1067/mtc.2000.106322 [DOI] [PubMed] [Google Scholar]
- 11.Wei D, Gao F, Wu B, et al. Single versus bilateral lung transplantation for idiopathic pulmonary fibrosis. Clin Respir J 2019;13:376-83. 10.1111/crj.13020 [DOI] [PubMed] [Google Scholar]
- 12.Keating D, Levvey B, Kotsimbos T, et al. Lung transplantation in pulmonary fibrosis: challenging early outcomes counterbalanced by surprisingly good outcomes beyond 15 years. Transplant Proc 2009;41:289-91. 10.1016/j.transproceed.2008.10.042 [DOI] [PubMed] [Google Scholar]
- 13.Neurohr C, Huppmann P, Thum D, et al. Potential functional and survival benefit of double over single lung transplantation for selected patients with idiopathic pulmonary fibrosis. Transpl Int 2010;23:887-96. [DOI] [PubMed] [Google Scholar]
- 14.Burdett C, Butt T, Lordan J, et al. Comparison of single lung transplant with and without the use of cardiopulmonary bypass. Interact Cardiovasc Thorac Surg 2012;15:432-6; discussion 436. 10.1093/icvts/ivs264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Perrot M, Chaparro C, McRae K, et al. Twenty-year experience of lung transplantation at a single center: Influence of recipient diagnosis on long-term survival. J Thorac Cardiovasc Surg 2004;127:1493-501. 10.1016/j.jtcvs.2003.11.047 [DOI] [PubMed] [Google Scholar]
- 16.Harringer W, Wiebe K, Strüber M, et al. Lung transplantation--10-year experience. Eur J Cardiothorac Surg 1999;16:546-54. 10.1016/S1010-7940(99)00313-9 [DOI] [PubMed] [Google Scholar]
- 17.Rubin AS, Nascimento DZ, Sanchez L, et al. Functional improvement in patients with idiopathic pulmonary fibrosis undergoing single lung transplantation. J Bras Pneumol 2015;41:299-304. 10.1590/S1806-37132015000000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith PW, Wang H, Parini V, et al. Lung transplantation in patients 60 years and older: results, complications, and outcomes. Ann Thorac Surg 2006;82:1835-41; discussion 1841. [DOI] [PubMed]
- 19.Thabut G, Mal H. Outcomes after lung transplantation. J Thorac Dis 2017;9:2684-91. 10.21037/jtd.2017.07.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schachna L, Medsger TA, Jr, Dauber JH, et al. Lung transplantation in scleroderma compared with idiopathic pulmonary fibrosis and idiopathic pulmonary arterial hypertension. Arthritis Rheum 2006;54:3954-61. 10.1002/art.22264 [DOI] [PubMed] [Google Scholar]
- 21.Grossman RF, Cooper JD. Lung transplantation. Immunol Allergy Clin North Am 1989;9:153-63. 19304274 [Google Scholar]
- 22.Burton CM, Milman N, Carlsen J, et al. The Copenhagen National Lung Transplant Group : survival after single lung, double lung, and heart-lung transplantation. J Heart Lung Transplant 2005;24:1834-43. 10.1016/j.healun.2005.03.001 [DOI] [PubMed] [Google Scholar]
- 23.Kreisel D, Krupnick AS, Puri V, et al. Short- and long-term outcomes of 1000 adult lung transplant recipients at a single center. J Thorac Cardiovasc Surg 2011;141:215-22. 10.1016/j.jtcvs.2010.09.009 [DOI] [PubMed] [Google Scholar]
- 24.Algar FJ, Espinosa D, Moreno P, et al. Results of lung transplantation in idiopathic pulmonary fibrosis patients. Transplant Proc 2010;42:3211-3. 10.1016/j.transproceed.2010.05.046 [DOI] [PubMed] [Google Scholar]
- 25.Villavicencio MA, Axtell AL, Osho A, et al. Single- Versus Double-Lung Transplantation in Pulmonary Fibrosis: Impact of Age and Pulmonary Hypertension. Ann Thorac Surg 2018;106:856-63. 10.1016/j.athoracsur.2018.04.060 [DOI] [PubMed] [Google Scholar]
- 26.Sampson M, McGowan J, Cogo E, et al. Managing database overlap in systematic reviews using Batch Citation Matcher: case studies using Scopus. J Med Libr Assoc 2006;94:461-3, e219. [PMC free article] [PubMed]