Abstract
SUMMARY: Cervical transforaminal blocks are frequently performed as a treatment of cervical radicular pain. These blocks are performed mostly under fluoroscopy, but a CT-guided technique also has been described. We describe a modification that leads to a more extraforaminal than transforaminal and equally selective nerve root block.
Cervical selective nerve root blocks (CSNRB) are commonly performed with fluoroscopic guidance.1 However, CT-guidance is also possible and has been described. CT guidance offers the advantage of enhanced anatomic resolution and a more precise positioning of the needle tip.2 Disadvantages are extended procedure times and increased exposure to radiation. In both the fluoroscopic and the CT-guided CSNRB, the aim is to block the root within the foramen. Therefore, the patient is placed in the supine position, and the foramen is reached laterally in a nearly horizontal plane. We describe a modification of the CT guidance technique in which the patient is in the prone position and the foramen is reached dorsally, with the tip of the needle aiming at the outer confines of the foramen. This technique leads to an extraforaminal, but still selective, nerve root block. It may imply a smaller risk for devastating complications such as spinal cord infarction or cerebellar infarction.
Technique
We obtained informed consent before the intervention. The procedure, its benefits, and its risks were discussed with the patient. Among the risks are the possibilities of infection, bleeding, and allergic reaction as well as a small risk for severe neurologic impairment, such as spinal cord stroke, or even death. The procedure is only performed by or under the supervision of an experienced spine interventionalist.
For dorsal access, the patient is placed in the prone position. The head is rested in a straight position with the forehead on a pillow. After a lateral scout image, the target level is marked, and images are obtained through the desired cervical neural foramen. An appropriate needle entry point is calculated before it is identified and marked on the skin before its sterilization. The entry site should be chosen to avoid carotid and jugular vessels and to gain access to the outer foramen. Usually, the needle is placed in a 45 to 90° lateral angle to the table.
Once the site is disinfected and the skin and subcutaneous tissue are anesthetized, a 22-gauge, 10-cm straight spinal needle (Seibel–needle; William Cook Europe, Bjaeverskov, Denmark) is partially inserted, and an initial image is obtained. The needle bears markings to control the depth of introduction.
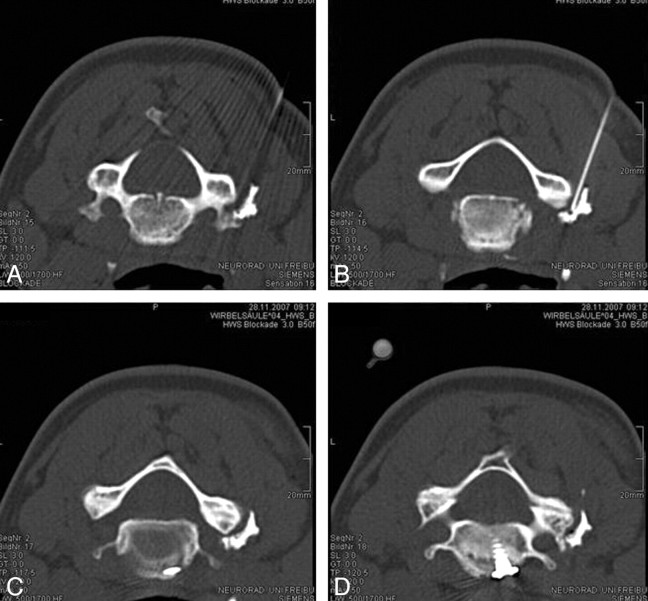
After the initial image is obtained, the needle is adjusted and advanced toward the posterior aspect of the neural foramen according to a preassigned trajectory in CT-guided technique. Usually 1 or 2 views, followed by another view after contrast application, are sufficient. The optimal placement of the needle tip is at the outer edge of the posterior foramen, which is reached in a 45–90° angle dorsally (Fig 1). The facet joint capsule can serve as a confine for the needle. Patients sometimes describe reproduction of their typical pain when the needle is in the right position.
Fig 1.
CT scan of the contrast distribution after CSNRB of the right C5 nerve root.
In the last 4 years, the authors have performed more than 200 procedures in a dorsal approach, most of them with a diagnostic indication. When performed with therapeutic indication, we used 4 or 8 mg of dexamethasone. We have never encountered any major complications such as medullary infarction, cerebellar infarction, or permanent neurologic deficit.
Discussion
CSNRB is a technique frequently used in cases of cervical radicular pain, with estimates ranging in the magnitude of more 30,000 per year in the United States.3 It can be used as a diagnostic tool, but more often it is performed therapeutically with local application of corticosteroids as an alternative to medical treatment or operative decompression of the nerve root.
Recently, there has been a growing awareness of possible devastating complications of the procedure including spinal cord, brain stem, and cerebellar infarction.4 Eight major complications have been published, but in all more than 30 cases are known.5 However, many of them have not been published because they are still sub judice. Among the published cases, there is also 1 case in which CSNRB was performed under CT guidance.6 In this case, a transforaminal access was chosen.
For most of the complications, an embolic mechanism from inadvertent injection of highly particulate material in the nerve root artery has been assumed.7
In 2007, complications were analyzed after an anonymous survey, and proposals were made to reduce the probability of their occurrence: the use of real-time fluoroscopy to detect vascular uptake, nonparticulate corticosteroids such as dexamethasone, and microbore extension tubing (“pigtail”) to minimize needle manipulation while changing syringes.5
CT guidance for dorsal access offers the possibility of still performing a selective block, as the contrast distribution pattern demonstrates. For the therapeutic efficiency of corticoids, it may not be important if the target point is located slightly more distal because of diffusional spread and strong axonal transport of corticoids.8 However, if an intraspinal epidural (less selective) distribution of the corticoid is intended, the conventional, or even a translaminar, approach is more suitable.
The prone position can mostly be made comfortable for the patient, with the use of pillows except for rare cases of patients with obstructive pulmonary disease or hyperkyphosis from ankylosing spondylitis. A comfortable positioning together with ample local anesthesia reduces problems of patient motion.
In our opinion, the above-described technique leads to minimization of the danger of inadvertent puncture of the nerve root artery compared with the conventional technique for 2 reasons: 1) the target point lies anteriorly to the plane in which the nerve root and the radicular artery can be expected and 2) the angle between the needle and the presumed course of the radicular artery is much more obtuse. Also, the vertebral artery is less at risk for puncture with the dorsal approach. The risk for puncture of the carotid and jugular vessels as well as the pharynx is negligible because they lie anteriorly. Apart from the advantages in security, the technique is simple, not very time consuming, and the required radiation dose is in an acceptable range.
References
- 1.Cluff R, Mehio AK, Cohen SP, et al. The technical aspects of epidural steroid injections: a national survey. Anesth Analg 2002;95:403–08 [DOI] [PubMed] [Google Scholar]
- 2.Wagner AL. CT fluoroscopic-guided cervical nerve root blocks. AJNR Am J Neuroradiol 2005;26:43–44 [PMC free article] [PubMed] [Google Scholar]
- 3.Manchikanti L. The growth of interventional pain management in the new millennium: a critical analysis of utilization in the Medicare population. Pain Physician 2004;7:465–82 [PubMed] [Google Scholar]
- 4.Rozin L, Rozin R, Koehler SA, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol 2003;24:351–55 [DOI] [PubMed] [Google Scholar]
- 5.Scanlon GC, Moeller-Bertram T, Romanowsky SM, et al. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine 2007;32:1249–56 [DOI] [PubMed] [Google Scholar]
- 6.Suresh S, Berman J, Connell DA. Cerebellar and brainstem infarction as a complication of CT-guided transforaminal cervical nerve root block. Skeletal Radiol 2007;36:449–52 [DOI] [PubMed] [Google Scholar]
- 7.Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med 2004;5:202–05 [DOI] [PubMed] [Google Scholar]
- 8.Frolkis VV, Tanin SA. Peculiarities of axonal transport of steroid hormones (hydrocortisone, testosterone) in spinal root fibres of adult and old rats. Neuroscience 1999;92:1399–404 [DOI] [PubMed] [Google Scholar]