Abstract
Background
Internet-delivered treatments for depressive symptoms have proved to be successful in high-income Western countries. There may be potential for implementing such treatments in low- and middle-income countries such as Colombia, where access to mental health services is limited.
Objective
The objective of this study was to assess the efficacy of a culturally adapted cognitive behavioral internet-delivered treatment for college students with depressive symptoms in Colombia.
Methods
This was a randomized controlled trial with a 3-month follow-up. The program comprised seven modules. A total of 214 Colombian college students were recruited. They were assessed and randomly assigned to either the treatment group (n=107) or a waiting list (WL) control group (n=107). Participants received weekly support from a trained supporter. The primary outcome was symptoms of depression, as measured by the Patient Health Questionnaire - 9, and the secondary outcomes were anxiety symptoms assessed by the Generalized Anxiety Disorder questionnaire - 7. Other measures, including satisfaction with treatment, were evaluated after 7 weeks.
Results
Research attrition and treatment dropouts were high in this study. On average, 7.6 sessions were completed per user. The mean time spent on the program was 3 hours and 18 min. The linear mixed model (LMM) showed significant effects after treatment (t 197.54=−5.189; P<.001) for the treatment group, and these effects were maintained at the 3-month follow-up (t 39.62=4.668; P<.001). Within-group results for the treatment group yielded a large effect size post treatment (d=1.44; P<.001), and this was maintained at the 3-month follow-up (d=1.81; P<.001). In addition, the LMM showed significant differences between the groups (t 197.54=−5.189; P<.001). The results showed a large effect size between the groups (d=0.91; P<.001). In the treatment group, 76.0% (16/107) achieved a reliable change, compared with 32.0% (17/107) in the WL control group. The difference between groups was statistically significant (X22=10.5; P=.001).
Conclusions
This study was the first contribution to investigating the potential impact of a culturally adapted internet-delivered treatment on depressive symptoms for college students as compared with a WL control group in South America. Future research should focus on identifying variables associated both with premature dropout and treatment withdrawal at follow-up.
Trial Registration
ClinicalTrials.gov NCT03062215; https://clinicaltrials.gov/ct2/show/NCT03062215
Keywords: culture, internet, cognitive behavioral therapy, depressive symptoms, students, South America
Introduction
High rates of prevalence of depression have been found worldwide and in various cultural groups [1-5], with an upward trend in prevalence in low- and middle-income countries (LMICs) [6]. In South American countries such as Colombia, high prevalence rates are reported, which are similar to the prevalence rates found in high-income countries (HICs) [3,4]. In Colombia, the 12-month prevalence rate has been estimated to be between 6.6% and 10% [7].
Studies have shown that Colombia reports the second highest prevalence of major depression in Latin America after Brazil [3,8]. An epidemiological report on the prevalence of mood disorders in LMICs shows that Colombia ranks first (6.9%), compared with India (5.5%), Iraq (4.1%), Nigeria (1.2%), Beijing (2.2%), and Shenzhen (4.8%) [9]. Recently, the Pan American Health Organization and World Health Organization [10] reported that most of the South American countries have higher depression disability (7.7%), specifically Paraguay (9.4%), Brazil (9.3%), Peru (8.6%), and Colombia (8.2%). The Colombian National Mental Health Survey [11] estimated a point prevalence of mild to moderate depressive symptoms in 15.6% and severe depressive symptoms in 4.2% of adults. In addition, a report [12] shows that moderate depression among women is 70.4% compared with that among men (29.6%). Depressive symptoms can go undiagnosed and untreated, and the absence of treatment may be associated with the development of a depressive disorder [13].
Depressive symptoms are commonly reported in general populations and among college students [14-16]. Cross-cultural studies show high rates of depressive symptoms among students [17,18]. Depressive disorders are more frequent among college students in comparison with the general population [19]. For instance, a systematic review showed a 30.6% weighted mean prevalence of depression symptoms in college students from Europe, the United States, Canada, Egypt, Turkey, Korea, Lebanon, and China [20]. These rates are comparable with those from Latin American countries [21-24]. In Colombia, a study reported high prevalence of depressive symptoms (30%) in students [25]. Another recent study showed 36.2% prevalence of depression symptoms in a college sample [26]. A recent report from Colombia showed that people with university studies presented with higher levels of depression (61.6%) compared to those without a higher education (45.2 %) [12]. Several variables have been associated with the vulnerability of college students to depression: changes in lifestyle related to poor sleep habits, eating disorders, economic stressors, and family problems [20,27].
Such a high prevalence warrants implementation of interventions for depression in Colombia. However, as in many other LMICs, there are barriers for accessing mental health treatments, such as cost and coverage, that prevent people from accessing the treatments they need [11,26]. In 2016, the World Mental Health survey reported that only 6.7% of college students received treatment for their mental health disorder in LMICs [28]. Furthermore, the population with mental health problems does not have an adequate insurance coverage [11,29]. The Colombian National Mental Health Survey in 2015 showed that about 50% of the population reported that personal stigma is one of the principal reasons for not accessing mental health services, followed by geographical location and limited service availability [11].
Despite the necessity to implement psychological interventions for depression in Latin America, there are only a few studies in this field [30], more so because treatments are mostly pharmacological, and evidence-based psychological treatments are rarely used. Furthermore, most of the treatments in LMICs are implemented without considering the cultural context of the clients; very little research has investigated culturally adapted treatments [31,32], whereas there is even less research on internet-delivered treatments [33,34] that may be a suitable alternative to make evidence-based treatments available, especially when nearly 56% of the population in Colombia has access to the internet [35].
Depressive symptoms can be effectively treated with psychotherapy and pharmacotherapy [36-39]. Psychological treatments for depression have shown better outcomes than a waiting list (WL) or placebo, and combined treatment is more effective than pharmacotherapy alone [38,40]. Research has found that psychological treatments can enhance the positive effect and decrease the negative effect in depression, contributing to better outcomes [41]. A systematic review and a meta-analysis have shown that cognitive behavioral therapy (CBT) had been extensively researched and was demonstrated to be effective for depression [42,43].
Low-intensity internet-delivered treatment is usually based on cognitive behavioral principles. It involves complete or partial guidance and uses CBT techniques that are typically used in face-to-face therapy, for instance, reading passages, listening to audio files, seeing pictures, and watching animations and videos [44,45]. This type of intervention is highly structured, and it involves psychoeducation, activities, and supplementary resources such as a supporter contact via asynchronous message [46].
Internet-delivered interventions have an established empirical base for major [47] and subthreshold [48,49] depression. They are also used as maintenance treatments [50-52]. For instance, a systematic review of computer-based interventions for depression, with a supporter, found a medium-to-large (0.58-0.76) and a small-to-medium (0.25-0.36) effect size when the intervention was delivered as a stand-alone self-help treatment for the reduction of depressive symptoms, both compared with usual care [51].
Internet-delivered interventions for depression are available in many languages. Research with Spanish language versions [53] reported positive results of the effectiveness of a CBT-based internet-delivered program for depression. A recent 4-year descriptive, naturalistic study monitoring a Web-based CBT treatment developed and researched in Mexico indicated that the intervention was useful for depressive symptoms [54]. In addition, a feasibility study in Chile found a Web-based treatment to be beneficial, acceptable, and feasible [55].
For the most part, there is availability of psychological treatments and mental health services in HICs. In addition, research evidence of internet-delivered interventions and their implementation have been mainly developed in HICs [56], whereas in LMICs, most people who need mental health services do not receive any—this is known as the mental health gap. For instance, the World Health Organization [57] has estimated that between 76% and 85% of the people with severe mental health problems receive no treatment in LMICs. Therefore, internet-delivered interventions may be a valuable resource to reduce the treatment gap in LMICs, such as Colombia, thus ameliorating social health inequalities in these regions [58]. In addition, there is little knowledge on internet-based interventions for depression emerging in such countries [34]. A recent systematic review found that only three articles reported the results of randomized controlled trials (RCTs) in internet-delivered interventions for mental health conditions in LMICs [33].
This study aimed at evaluating the efficacy of a culturally adapted internet-delivered CBT (iCBT), Yo puedo sentirme bien/I can feel better program, for college students with depressive symptoms. This study is the first contribution to investigating the efficacy of an iCBT intervention in Colombia.
Methods
Study Design
The study used a randomized control design (trial registration: ClinicalTrials.gov NCT03062215) to examine the efficacy of the culturally adapted intervention in which participants were randomly assigned to two groups: (1) a culturally adapted iCBT group and (2) a WL control group.
Participants
College students from two cities and universities in Colombia were included in this study. Both undergraduate- and graduate-level students from any school at a university in Bogota City and students of psychology, medicine, nursing, and education from a university in Bucaramanga City in Colombia were eligible to participate, and they were selected according to the criteria described in Textboxes 1 and 2.
Inclusion criteria.
Age ≥18 years
Mild to moderately severe depressive symptoms determined by the Patient Health Questionnaire - 9 scores of 10-19
Exclusion criteria.
Severe depressive symptoms: score of >19 on the Patient Health Questionnaire - 9
Suicidal ideation or intent: score of ≥2 on question 9 of the Patient Health Questionnaire - 9
Psychosis
Currently in psychological treatment for depression
On medication for <1 month
Alcohol or drug misuse
Previous diagnosis of an organic mental health disorder
Depression preceding or coinciding with a diagnosed medical condition
User Recruitment
An email with information about the study and a link to access to the treatment was sent to all college students (undergraduates and postgraduates) in Bogota university and to undergraduate students studying medicine, psychology, and education in Bucaramanga university. Potential participants were able to visit a website to receive information about the study, participation criteria, treatment, and how to get in contact to proceed with the study. Recruitment took place between August 2016 and January 2017.
Procedure
Overview
Once participants read the study information, informed consent was obtained from each user before screening and randomization. Through the SilverCloud platform, participants were instructed to type their name on the informed consent page to indicate that they had read and understood the study information and agreed to participate in the study. Thereafter, participants completed measures for screening purposes, including the Patient Health Questionnaire - 9 (PHQ-9), Sociodemographic and Clinical History Questionnaire, and Generalized Anxiety Disorder - 7 (GAD-7) questionnaire. Thereafter, participants who were eligible for the study (Textbox 1) were randomized through computer algorithms and assigned to one of two groups: the iCBT treatment and WL control groups.
Participants assigned to the active treatment group started the internet-delivered treatment immediately for 7 weeks, whereas treatment for the WL participants started after 7 weeks. Individuals not meeting the inclusion criteria at baseline assessment were referred to other appropriate sources of face-to-face support at the student counseling service in their respective universities. Once the students completed the questionnaires, they received immediate feedback on their results. If exclusion from the study was necessary, information and advice to seek counseling services at their college was provided to the student. In addition, the counseling service manager received an automatic email with information of the excluded students, their questionnaires (ie, Sociodemographic and Clinical History Questionnaire, PHQ-9, and GAD-7), and their scores. Participants received emails and calls from the research team at the posttreatment and 3-month follow-up time points to encourage them to complete their assigned measures.
Randomization
After baseline screening, eligible participants were randomized and informed immediately about their group assignment. Randomization was handled by a computer algorithm administered by a person independent of the researchers. Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) participant flow through the trial.
Figure 1.
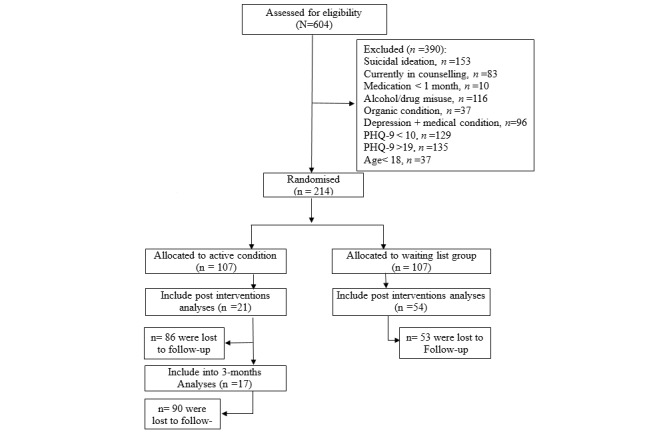
Study participants flowchart—Consolidated Standards of Reporting Trials diagram. PHQ-9: Patient Health Questionnaire - 9.
Intervention
The Colombian iCBT program for depression assigned as treatment in this study (Yo puedo sentirme bien/I can feel better) is a modified version of the clinically efficacious Space from Depression program [59] used in Ireland and the United Kingdom. The name Yo puedo sentirme bien (I can feel better in English) was selected as a culturally appropriate descriptor for improving mood to avoid the negative connotations related to depression in Colombian culture.
The cultural adaptation that underwent several steps is described in a separate study [60]. The adaptation involved three distinct phases based on an integrative approach proposed by the author (AS). In the first phase, it involved a top-down cultural sensitivity framework, developed by the principal researcher (AS). The preliminary adaptation included work done by professional translators and an independent video company in Colombia. The first phase in the adaptation comprised a translation of the program from English to Spanish and the incorporation of cultural expressions, examples, and personal stories into the program. The second phase comprised an assessment of the preliminary program through the Cultural Relevance Questionnaire (CRQ) that was designed specifically for this study. The CRQ is based on cultural sensitivity and ecological validity theory [61] and principles from cross-cultural assessment research [60,62]. The CRQ has two sections: (1) a general assessment of the program and (2) an assessment of each module, including feedback from college students and psychology experts. The third phase involved further development of cultural incorporations into the program based on this feedback [60].
Both Yo puedo sentirme bien (the Colombian iCBT program used as treatment in this study) and Space from Depression (the original program from which it was culturally and linguistically adapted) comprise seven modules of CBT (Table 1) [63]. The treatment includes self-monitoring, behavioral activation, cognitive restructuring, and challenging core beliefs. All modules have the same structure and format, comprising quizzes, videos, educational content, and activities with homework suggestions and a module review page (Multimedia Appendices 1 and 2). Moreover, users have a supporter who provides weekly feedback asynchronously [59].
Table 1.
Yo puedo sentirme bien/Space from Depression program description.
| Module | Brief description | ||
| Getting started | Outlines the basic premise of cognitive behavioral therapy, provides information about depression, and introduces some of the key ideas of Space from Depression; users are encouraged to begin to chart their own current difficulties with depression | ||
| Tune in | |||
|
|
I: Getting to grips with mood | The focus in this module is on mood monitoring and emotional literacy; users can explore different aspects of emotions, physical reactions, action and inaction, and how they are related | |
|
|
II: Spotting thoughts | This module focuses on noting and tracking thoughts; users can explore the connection between their cognitions and mood and record them graphically | |
| Change it | |||
|
|
I: Boosting behavior | This module focuses on behavioral change as a way to improve mood; ideas about behavioral activation are included, and users can plan and record activities and chart their relationship with their mood | |
|
|
II: Challenge your thoughts | This module supports users to challenge distorted or overly negative thinking patterns, with thought records as well as helpful coping thoughts | |
|
|
III: Core beliefs | This module outlines the role that deeply held core beliefs could play in mood and depression; users can use a range of interactive activities to identify, challenge, and balance any unhelpful core beliefs | |
| Bringing it all together | In this final module, users are encouraged to bring together all the skills and ideas they have gathered so far, note their personal warning signs, and make a plan for staying well | ||
The participants accessed the intervention for free during the time of the study. They also had access to the program without a supporter for a year after the study if they wanted to use it.
Wait List Control Group
Participants in the WL control group received treatment only after 7 weeks; therefore, this group received no treatment in the first 7 weeks of the study.
Supporters
Each of the 214 participants were assigned a supporter, who was a postgraduate student in clinical psychology with experience delivering CBT for adults. A total of 10 supporters were trained by the principal researcher (AS) to use the Yo puedo sentirme bien/I can feel better platform and program before starting their role as a supporter, and they were supervised by an experienced clinical psychologist at the university.
Each supporter was assigned users. Supporters provided asynchronous postsession feedback of 10-15 min per participant per week through the platform. The role of the supporter was to motivate and provide feedback to the users. The feedback was focused on improving adherence to the interventions and encouraging the application of CBT activities in the program. They scheduled the feedback at specific times, once each week for a period of 7 weeks. This schedule of support replicated what had already been implemented with the program in the Irish RCT. The messages explain how to work through the program; the supporters also suggested modules and activities to the users. All the messages were personalized, depending on the user’s necessities (the content used or specific questions or comments the user made to the supporter through the platform). Further, 7 weekly automated alert messages were sent by email to all the participants, indicating that they had received a new review from their supporter.
Assessments
Through the SilverCloud platform, the assessments were completed by the participants. For the efficacy trial, participants were assessed at baseline, posttreatment, and 3-month follow-up; details of the measures are described in Table 2.
Table 2.
Measures used (study: efficacy trial—screening and primary and secondary outcomes).
| Measure | Assessed variable | Time of assessment |
| Patient Health Questionnaire - 9 | Depression symptoms | Baseline, posttreatment, and follow-up |
| Generalized Anxiety Disorder - 7 | Anxiety symptoms | Baseline, posttreatment, and follow-up |
| Sociodemographic and Clinical History Questionnaire | Gender, age, marital status, education, occupation, socioeconomic status, and clinical history | Baseline |
| Helpful and Hindering Aspects of Treatment> | Helpful and hindering aspects of treatment | After each session |
| Satisfaction | Satisfaction with the therapy | Posttreatment |
Participants were assessed at baseline using the PHQ-9, Sociodemographic and Clinical History Questionnaire, and GAD-7. At the beginning of each session, participants were asked to reflect on their previous session and complete the Helpful Aspects of Treatment Form, a qualitative measure, the results of which are not presented in this paper. PHQ-9 and GAD-7 were completed at week 7 and follow-up was completed at week 20 (3 months). A Satisfaction With Treatment (SAT) questionnaire was completed after week 7.
Screening Measure
Sociodemographic Information and Clinical History Questionnaire
This instrument was developed on the basis of a previous version [64]. It collects data on the participants, such as the length of time one is experiencing depression symptoms; the participant’s experience of counseling/therapy and medication for depression; and whether one has had a previous diagnosis of an organic mental health disorder or serious mental health disorders such as schizophrenia, psychosis, and bipolar disorder. In addition, it contains items related to comorbidity of depression, such as alcohol and drug misuse, or any recent medical diagnosis.
Outcome Measures
Primary Outcome: Patient Health Questionnaire - 9
The PHQ-9 [65] is a 9-item self-report measure that assesses the nine depression symptoms from the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), depression criteria. Each item is scored on a 4-point scale (0-3), and scores range from 0 to 27. The score can be used to describe a patient’s symptoms in one of the five categories: none (0-4), mild (5-9), moderate (10-14), moderately severe (15-19), and severe (20-27). The PHQ-9 has been shown to have good internal reliability (Cronbach alpha=0.86-0.89) [66]. The PHQ-9 has been translated into Spanish, and a Colombian version will be used in this study. The Spanish version of PHQ-9 has also demonstrated good reliability among Latinos in the United States (alpha=.85) [67,68]. In this study, the internal consistency of the PHQ-9 in the sample was .87.
Secondary Outcome: General Anxiety Disorder - 7
The GAD-7 [69] comprises seven items measuring symptoms and severity of anxiety based on the DSM-IV diagnostic criteria. It has shown good internal reliability (alpha=.92) [70]. It has been culturally adapted into Spanish [71] and is available in a Colombian Spanish version. In this study, the internal consistency of the GAD-7 in the sample was .88.
Other Measures
Posttreatment: Satisfaction With Treatment
At posttreatment, participants were asked to complete the SAT questionnaire [72]. It asks users about positive and negative experiences with the internet-delivered treatment. It contains two questions asking participants to describe what they most and least liked about the Web-based treatment.
Data Analysis
All participants’ data were included, irrespective of treatment compliance. Descriptive statistics (Chi-square and t tests) were used to analyze sociodemographic and clinical variables at the baseline among the groups (eg, gender and age) [73].
The effect of treatment on PHQ-9 and GAD-7 severity scores was evaluated separately for each measure by using the repeated-measures linear mixed-effects models fit with restricted maximum likelihood in the R package lme4 [74]. The core computational algorithms are implemented using the “Eigen” C++ library for numerical linear algebra and “RcppEigen glue” in the R (general public license ≥ version 2.0) [75]. Linear mixed-effects models are appropriate for analysis of longitudinal data where repeated measurements are taken from the same subjects over time and are particularly robust to missing data. All participants who provided posttreatment measures or 3-month follow-up measures, irrespective of treatment compliance, were included. Linear mixed model (LMM) fit by the restricted maximum likelihood (REML) t test using Satterthwaite method was employed to estimate covariance matrix, including fixed effects for time [74,76]. The REML approach is a particular form of maximum likelihood estimation that does not base estimates on a maximum likelihood fit of all the information, but instead uses a likelihood function calculated from a transformed set of data. For each measure, total scores were modeled using fixed effects of time, treatment group and the interaction between time and treatment group, and a random effect of individual/identification. The significance of each fixed effect was evaluated with t tests using the Satterthwaite degrees of freedom method [77]. Post hoc pairwise comparison of means estimated from the models were performed using the R package. All reported P values are two-tailed, with significant levels at P<.01, P<.01, and P<.05. The magnitude of the treatment effect within and between the two groups was assessed using the Cohen d statistic [73]. Cohen describes an effect size of 0.2 as small, 0.5 as medium, and 0.8 as large [78].
Analyses were conducted to assess how many participants achieved clinically significant changes at the end of the intervention and at follow-up. The assessments were made through a comparison of pretreatment scores with posttreatment and follow-up scores on the outcome measures PHQ-9 and GAD-7. Reliable change was assessed using the Jacobson and Truax reliable change criteria. Internal consistency, measured with Cronbach alpha, was used as the reliability estimate, and it was high for both the PHQ-9 (alpha=.89) and GAD-7 (alpha=.88). Change on either measure was considered reliable if it exceeded the resulting reliable change index, which was calculated to be 3.98 for the PHQ-9 and 3.61 for the GAD-7. Reliable recovery criteria were calculated as the combination of the reliable change index (RCI) and cutoff score and the percentage of participants who achieved a posttreatment score of ≤10 on the PHQ-9 and ≤8 on the GAD-7.
Descriptive statistics were used to analyze the quantitative data from the SAT questions, and the qualitative responses from this questionnaire were analyzed using thematic analysis. The categorization of data followed that identified in the previous research [79].
Ethics
The research project and all related materials were submitted and approved by the appropriate university ethics committees in Colombia. Participants were provided with the study information including the aims and objectives and provided informed consent. Participants meeting exclusion criteria were referred to other appropriate sources of support at the universities. The study protocol, information on the study, informed consent, and related materials were submitted and approved by the ethics committee of the two universities.
Results
Baseline Characteristics
Descriptive statistics revealed that at postrandomization, there were no significant differences in the sample between the iCBT and WL control groups on any variables. Table 3 shows details of the characteristics of the sample. The mean age was 22.15 (SD 4.74) years. All the participants were full-time students. The majority of the college student sample was from health sciences (86/214, 40.2%), followed by social sciences (62/214, 29.0%), and engineering (37/214, 17.3%).
Table 3.
Demographic and clinical variables.
| Variable | Total (N=214), n (%) | Treatment (N=107), n (%) | Control group (N=107), n (%) | P value | ||||||
| Gender | .56 | |||||||||
|
|
Female | 153 (71) | 74 (69.2) | 79 (73.8) |
|
|||||
| Male | 61 (28.5) | 33 (30.8) | 28 (26.2) |
|
||||||
| Age (years) |
|
|||||||||
|
|
Mean (SD) | 22.15 (4.7) | 22.24 (5.4) | 22.06 (3.9) | .98 | |||||
| Range | N/Aa | 18-52 | 18-37 | — | ||||||
| Education subject | .81 | |||||||||
|
|
Health sciences | 86 (40.2) | 46 (43.0) | 40 (37.4) |
|
|||||
| Social sciences | 62 (29.0) | 31 (29.0) | 31 (29.0) |
|
||||||
| Engineering | 37 (17.3) | 17 (15.9) | 20 (18.7) |
|
||||||
| Postgraduate subjects | 29 (13.6) | 13 (12.1) | 16 (15.0) |
|
||||||
| Time with symptoms | .31 |
|
||||||||
|
|
<6 months | 56 (26.1) | 28 (26.2) | 28 (26.2) |
|
|||||
| 1-2 years | 75 (35.0) | 42 (39.3) | 33 (30.8) |
|
||||||
| 2-5 years | 43 (20.0) | 22 (20.6) | 21 (19.6) |
|
||||||
| >5 years | 40 (18.6) | 15 (14.0) | 25 (23.4) |
|
||||||
| Previous therapy for depression | .32 | |||||||||
|
|
Yes | 47 (21.9) | 20 (18.7) | 27 (25.2) |
|
|||||
| No | 167 (78.0) | 87 (81.3) | 80 (74.8) |
|
||||||
| Previous medication for depression | .72 | |||||||||
|
|
Yes | 37 (17.2) | 20 (18.7) | 17 (15.9) |
|
|||||
| No | 177 (82.7) | 87 (81.3) | 90 (84.1) |
|
||||||
| Current medication for depression | >.99 | |||||||||
|
|
Yes | 7 (3.2) | 3 (18.7) | 4 (15.9) |
|
|||||
| No | 207 (96.7) | 104 (81.3) | 103 (84.1) |
|
||||||
| Information technology–related confidence | .02 | |||||||||
|
|
Very confident | 6 (2.8) | 2 (1.9) | 4 (3.7) |
|
|||||
| Confident | 72 (33.6) | 35 (32.7) | 37 (34.6) |
|
||||||
| Average | 4 (1.8) | 2 (1.9) | 2 (1.9) |
|
||||||
| Mildly confident | 72 (33.6) | 52 (23.4) | 20 (18.7) |
|
||||||
| Not confident | 87 (40.6) | 43 (40.2) | 44 (41.1) |
|
||||||
aNot applicable.
There was no significant difference between the proportions of participants who reported a previous diagnosis of depression in the control group versus the treatment group. The majority of the participants reported depressive symptoms of between 1 and 2 years (35.0%, 75/214). Of the participants, 21.9% (47/214) reported to have had counseling/psychotherapy for depression in the past. Finally, the sample reported confidence in their use of information technology (IT), with 33.6% (72/214) of participants reporting feeling confident. Of the participants, 40.6% (87/214) reported feeling not so confident using technology.
Treatment Response Rate
Participants were offered 7 modules to complete. Similar to the original efficacy trial, although they were instructed to complete each of the 7 modules, the choice, pace, and control over the direction and dose of their engagement was entirely up to them [59]. Of the 107 participants randomized to the immediate treatment group, 80% (86/107) began module 1, and 9.3% (10/107) completed all modules. Figure 2 represents the treatment response rate over time.
Figure 2.
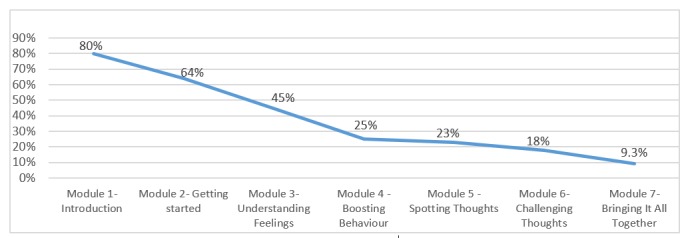
Percentage of users accessing modules over time.
A session in a Web-based intervention is defined as an instance when a client logged into the system [59]. Session time estimation is not exact because users may be interrupted or take breaks within a session and may not formally log out of the system. Regarding the treatment group, the total number of sessions completed was 734, with an average of 7.6 sessions completed per user. The mean time spent on the program was 3 hours and 18 min.
Research Data Attrition
A total of 604 participants were screened, of which 390 were excluded based on the established criteria. A significant number of participants were excluded because of suicidal ideation (153/604, 25.3%) and misuse of drugs or alcohol (116/604, 19.2%). At sign-up, there were a total of 107 participants assigned to the treatment group and 107 assigned to the WL control group. See CONSORT flow in Figure 1.
The Little´s Missing Completely at Random (MCAR) test revealed a nonsignificant result (X24=1.28; P=.86), indicating that the data were missing completely at random [80]. The percentage of participants who completed research measures at postintervention was 19.6% (21/107) and the 3-month follow-up was 16.8% (18/107). In the WL group, the response was higher, with 50.4% (54/107) of participants present at the postintervention assessment. The WL control group was not followed up beyond this point, as they entered treatment.
Intention-To-Treat Analysis
Owing to the very high percentage (86/107, 80.3%) of missing data in the sample, we decided not to follow the protocol data analysis strategy [63]. Instead, we modified our approach to include only those participants who provided posttreatment measures (21/107, 19.6%) or the 3-month follow-up (18/107, 16.8%) measures.
Patient Health Questionnaire - 9
The iCBT and WL control group samples were compared using LMMs, adjusting for depression and anxiety scores in the model. LMM including fixed effects for time showed significant effects after treatment (t 38.23=−5.079; P≤.001) within the iCBT treatment group. The effects were also maintained at the 3-month follow-up (t 39.62=−4.668; P≤.001) for the treatment group (see Table 4). Also, LMM shows significant differences between the groups (t 197.54=−5.189; P≤.001) in favor of the treatment group.
Table 4.
Descriptive data for the Patient Health Questionnaire - 9 and Generalized Anxiety Disorder - 7 by group over time (intention to treat).
| Outcome measures | Treatment | Follow-up | |||||||||||
|
|
|
Baseline | Pretreatment | Posttreatment | Within-group effect size (95% CI) | Baseline | 3-month follow-up | Effect size (95% CI) | |||||
|
|
|
t (df) | P valuea | n | Mean (SD) | n | Mean (SD) |
|
t (df) | P valueb | n | mean (SD) |
|
| Patient Health Questionnaire - 9 | |||||||||||||
|
|
Treatment group | −5.079 (38.23) | ≤.000 | 107 | 14.22 (2.81) | 21 | 8.33 (5.71) | 1.44 (0.38 to 2.49) | −4.668 (39.62) | ≤.000 | 17 | 8.41 (5.98) | 1.81 (0.69 to 2.92) |
|
|
Waiting list group | N/Ac | N/A | 107 | 13.82 (2.93) | 54 | 13.09 (5.06) | 0.20 (−0.78 to 0.58) | N/A | N/A | N/A | N/A | N/A |
| Generalized Anxiety Disorder - 7 | |||||||||||||
|
|
Treatment group | −2.632 (37.83) | ≤.012 | 107 | 10.56 (4.380) | 21 | 7.19 (4.79) | 0.73 (0.08 to 1.37) | −2.486 (38.88) | ≤.017 | 17 | 7.83 (6.23) | 0.52 (−0.17 to 1.21) |
|
|
Waiting list group | N/A | N/A |
|
|
|
|
|
N/A | N/A | N/A | N/A | N/A |
aCompared to posttreatment.
bCompared to the 3-month follow-up.
cNot available.
The within-group results for the treatment group yielded a large effect size after treatment (d=1.44; P≤.001), and this was maintained at the 3-month follow-up (d=1.81; P≤.001). Similarly, the results showed a large effect size between groups (d=0.91; P≤.001). Figure 3 provides a graphical representation of the changes in depressive symptoms between groups pre- and posttreatment.
Figure 3.
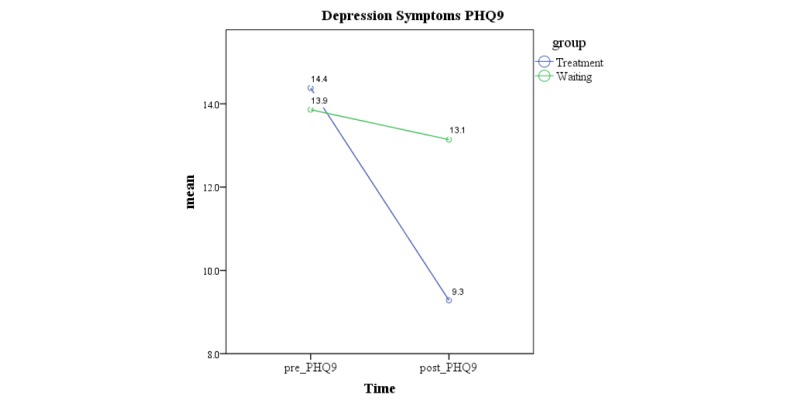
Changes in depression symptoms pre- to postintervention. PHQ-9: Patient Health Questionnaire - 9.
Generalized Anxiety Disorder - 7
Similarly, the iCBT group and WL control group samples were compared using LMM. Within the iCBT group, time point was a significant predictor of the GAD-7 score, with a significant effect from baseline to posttreatment (t 37.83=−2.632; P≤.012) and the 3-month follow-up (t 38.8=−2486; P≤.017; Table 4) within the treatment group. The interaction effect was also significant, representing significant differences in the GAD-7 score change observed from baseline to posttreatment between the groups (t 103.53=−2.229; P≤.03) in favor of the treatment group.
The within-group results for the treatment group yielded a medium-to-large effect size after treatment (d=0.73; P≤.001), and this was maintained at the 3-month follow-up (d=0.52; P≤.001). The mean scores indicated that the treatment group reported significantly lower levels of anxiety symptoms after treatment than those in the WL control group, yielding a medium posttreatment effect size between the groups for the intervention (d=0.60; P≤.001). Figure 4 provides a graphical representation of the changes in anxiety symptoms between groups.
Figure 4.
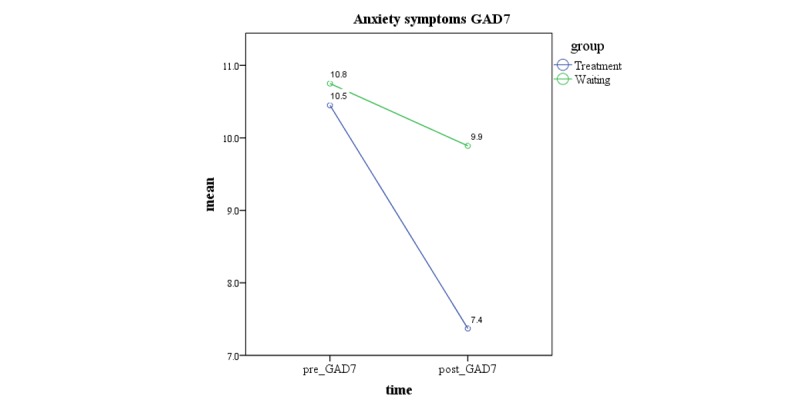
Changes in anxiety symptoms pre- to postintervention. GAD-7: Generalized Anxiety Disorder - 7.
Clinically Significant and Reliable Change
RCI values were calculated in this sample population. For the PHQ-9, change was needed to exceed the RCI value of 3.97, and for the GAD-7, a value of 3.63, to be considered reliable. The proportion of each group that showed reliable improvements (or deterioration) between baseline and posttreatment and the 3-month follow-up was determined using these reliable change criteria. The analysis included only the number of participants who provided follow-up measures.
In the iCBT group, 76% (n=16) achieved reliable change, compared with 32% (n=17) in the WL control group. The differences between groups were statistically significant (X22=10.519; P=.001). Reliable recovery from depression and anxiety was established by identifying the RCI and the percentage of participants who achieved a posttreatment score of ≤10 on the PHQ-9 and ≤8 on the GAD-7. In the iCBT group, 10 (n=10) participants met the criteria for reliable recovery on depression symptoms and 9 (n=9) met the criteria for the same on anxiety symptoms.
Satisfaction With Treatment
After 7 weeks, the participants (n=40) also completed the SAT questionnaire. Most of the users were happy to use a computer to access their treatment (76%, n=30) and found the interventions easy to use (82%, n=32). Furthermore, the majority of participants (68%, n=27) found the Web-based treatment helpful (Table 5).
Table 5.
Results from the Satisfaction With Treatment questionnaire, (n=40).
| Questionnaire items |
Participants | ||
| Agree (%) | Disagree (%) | Neither (%) | |
| I was happy to use the computer to access the treatment | 76 | 8 | 16 |
| I found the intervention easy to use | 82 | 5 | 13 |
| I feel the treatment received will have a lasting effect | 63 | 8 | 29 |
| I would recommend the Web-based treatment to others | 68 | 16 | 16 |
| How helpful you found the Web-based treatment program | 68a | 23b | 10c |
aHelpful.
bA little helpful.
cNot at all helpful.
The final two questions in the satisfaction measure were qualitative and asked participants what they most and least liked about the Web-based treatment. The majority of the users reported its accessibility and flexibility (n=20, 50%) as the aspects they liked the most. The other aspects liked were the applicability of the program to their life, having a supporter, and the interactive tools and the activities:
The availability of all the material that it includes and the sense of security that it gives to know that I can receive help at any time.
The strategies proposed are very effective that allows us to question about the [negative] habits have [are unhelpful] to lead a happier life.
...That I could keep track of my emotions and moods.
When asked what they least liked about the Web-based treatment program, some participants reported that the program did not meet their individual needs, such as immediate feedback or synchronic interaction with the supporter (n=11, 28%) and lack of time (n=4, 10%).
The platform is impersonal. Perhaps, it was not what I needed to hear. Perhaps, nothing replaces being in touch in real life with someone.
Discussion
Principal Findings
The study aimed at evaluating the efficacy of a culturally adapted Yo puedo sentirme bien/I can feel better program for college students with depressive symptoms in Colombia. The results show a very high research attrition and treatment dropout in this sample. However, the treatment group demonstrated statistically significant decreases in depressive symptoms from baseline to posttreatment, relative to the pre-post change in the WL control group, and this reduction in symptoms was maintained at the 3-month follow up. Furthermore, a significantly larger proportion of the iCBT group achieved a reliable change, compared with the WL control group. The results from this study thus showed that the culturally adapted cognitive behavioral internet-delivered program, Space from Depression, is effective in reducing depressive symptoms in comparison with a WL control group. These results support previous research findings on the Space from Depression program in Ireland [59]. The findings presented here indicate that the program can potentially be used with other cultural groups, provided that it is modified to contain culturally adapted components.
The results in this study also showed that positive changes in depressive symptoms can be maintained by users at the 3-month follow-up. This is a relevant finding regarding maintenance of gains achieved from an internet-delivered intervention. Previous research [81,82] in culturally adapted internet interventions for depression with Arab and Chinese immigrants has been consistent in demonstrating lasting effects. For instance, a study [81] found that a reduction in depressive symptoms was still maintained at the 3-month follow-up within a population of Chinese immigrants.
Furthermore, this study found that the Yo puedo sentirme bien/I can feel better program is effective in reducing comorbid symptoms of anxiety in comparison with a WL control group. Statistically significant reductions were observed in anxiety symptoms for the intervention group from pre- to posttreatment, and these were maintained at the 3-month follow-up. The results support the efficacy of this internet-delivered cognitive behavioral intervention for depression and anxiety, as has been observed in a previous study of the intervention in English [59]. Similarly, a study [83] showed a significant reduction in depression and comorbid anxiety after treatment and at the 3-month follow-up in an RCT with Turkish immigrant residents in the Netherlands.
This RCT reports the results from the first culturally adapted internet-delivered program with asynchronous Web-based support in an LMIC in South America. The intervention showed similar outcomes to those established previously in Web-based treatments for depression and anxiety in HICs [51,59,84-86]. The evidence base for internet-delivered interventions for depression and anxiety symptoms comes mainly from people living in developed countries [56], whereas iCBT may be a valuable resource to reduce the treatment gap for those living in less developed countries, thus ameliorating social health inequalities between regions [58].
Furthermore, a reliable change was achieved by a greater percentage of those in the iCBT group (n=16, 76%), compared with those in the WL control group (n=17, 32%). The reliable change in internet-delivered interventions has showed greater percentage in different studies in the literature based on intention-to-treat (ITT) samples. For instance, a study of culturally adapted iCBT for depression reported a reliable change in the treatment group (32%) as measured using the Center for Epidemiological Studies-Depression [83]. In addition, a culturally adapted transdiagnostic iCBT for depression and anxiety [87] reported that participants made a 50% greater improvement on the PHQ-9 at posttreatment and the 3-month follow-up, respectively, using a posttreatment score at or below the clinical cutoff on the PHQ-9 (≥10) as a criterion for reliable change. A study of the internet-delivered treatment for depression upon which this cultural adaptation is based, the Space from Depression program, reported a 31% reliable change in the treatment group by using a criterion of change of ≥9 points on the Beck Depression Inventory-II from pre- to posttreatment [59].
The participants in the iCBT group spent an average of 3 hours and 18 min using the treatment and an average time of 18.2 min per session. Participants determined the amount of time they spent on the platform, which is a feature of internet-delivered interventions. A research study using the Space from Depression program with a sample from the general population in Ireland showed a greater mean time spent on the program in this population (5 hours 22 min) [59]. This difference in time spent using the intervention could be associated with time limitations within the college student sample in Colombia, where exam weeks and academic tasks can affect people’s use of the program. This time limitation among college students may have also compromised the success of the intervention (ie, the high dropout). Studies have identified factors that could influence the time spent on the Web, such as processing speed, cognitive ability, reading aptitude, and familiarity using computers [88].
High Levels of Depressive Symptoms and Suicidal Ideation
Both colleges reported high exclusion criteria at the beginning (64% of participants were excluded before they were randomized to treatment and WL control groups). For instance, in Bogota, a high proportion of students were excluded because of suicidal ideation (n=130, 24%) and drug/alcohol misuse (n=94, 17%). Similarly, in Bucaramanga, a high proportion of students reported suicidal ideation (n=23, 12%) and alcohol and drug misuse (18%, n=22). The exclusion might be considered higher compared with other studies in HICs [53,59,89]. In culturally adapted internet-delivered treatment for depression, high exclusion rates related to suicidal ideation have been reported in different populations [81,83]. Studies have supported that the reasons for the exclusion may include different interpretations that communities have about mental disorders that may not be considered in the measures used for depression [2,90]. More studies are needed in this area to develop validated measures considering cultural differences. In addition, college students typically report a higher prevalence of depression, suicidal ideation, and alcohol/drug misuse [20,28], and there are similar reports in South America [26,91].
Furthermore, the iCBT program was tested for mild-to-moderate depressive symptoms, which shows the necessity of its use in higher levels of depression or more precise measures to assess participants with more significant levels of depression, given how common it was for people to be screened out for psychological symptoms. The Space from Depression program has also reported efficacy with this population [92]; future studies should be considered at this point.
Attrition
Research Attrition
In this study, only 20% of the participants completed measures after treatment and 17% completed them at the 3-month follow-up. This very high attrition is not easily comparable with other culturally adapted internet-delivered treatment for depression studies. For instance, a study [83] showed that 58% participants completed the posttreatment measures (6 weeks), and 38% filled the follow-up assessment at 4 months. In addition, Choi et al [81] reported that 92% of the users completed the posttreatment questionnaires, and 84% of participants completed the questionnaires at the 3-month follow-up. Internet-delivered interventions for depression have showed higher retention rates, for example, a study [93] reported 49% of participants providing data at posttreatment and 35% at follow-up. In a previous study using the Space from Depression program, 63% of participants completed measures after treatment (8 weeks), and 52% completed 3-month follow-up measures [59]. Procedural variables could be associated with the very high research attrition rate in this study, such as phone numbers of the participants not being available from the beginning of the study and limiting phone calls to the participants to encourage them to complete the measures after treatment.
In this study, recruitment was conducted by email, and therefore, there was no face-to-face contact with the participants. Personal contact at the beginning of the intervention would have, perhaps, encouraged the participants’ engagement and continuation with the program. This is also associated with another factor linked to attrition—lack of reminders [94]. In this study, users received emails and calls at the end of the study to encourage them to complete the measures. Some limitations were present, such as the calls being made from Ireland, where there is a significant time difference with Colombia. Therefore, it was not possible to call the participants during a specific time that they might be more likely to answer the phone. Moreover, it is likely that for some participants, reminder emails went to spam.
Studies have suggested personality factors, cognitive abilities, and motivation as relevant determinants for attrition [95]. We did not evaluate these elements in this study. Future studies should examine strategies to decrease attrition rates, which is a determinant of effectiveness in internet interventions.
Treatment Dropout
Only a small proportion of participants completed all modules; 80% (86/107) of the participants in the iCBT group began with module 1, and 9% (10/107) completed all modules. Treatment dropout has been found to be a problem in internet interventions [94,96]. However, studies have shown that having a supporter is associated with higher engagement and efficacy in Web-based interventions [51,97]. Unfortunately, that was not the case in this study. Despite the training provided to the supporters in the Web-based program and their experience in CBT, the population engagement was low. The possible reasons could include barriers related to accessing mental health treatments in Colombia, such as lack of motivation for change, negative perception of psychological treatments, and personal stigma [26]. In addition, this is the first study with internet-delivered interventions in Colombia and in South America, which might affect the engagement with the treatment.
Furthermore, possible cultural differences and specific characteristics of the college student sample could be considered in future studies in Colombia to try to improve engagement with the treatment. For instance, the structure of the year and competing demands on students, for example, exams and holiday periods, can have a detrimental impact on engagement and adherence to any intervention. In addition, a lack of reminders has been associated with participant dropout [94]. In this study, participants received an automatic alert email each week from their supporter. It is probable that these automatic alerts were received as spam, and consequently, the participants could have forgotten to use the program and dropped out from the intervention. In addition, 87 participants (41%) of the population in this study reported low IT confidence, which could be another dropout factor and may affect engagement with the intervention [98]. Studies have associated the low use of technology with attrition in Web-based interventions [95]. Future studies could assess and develop strategies to support participants with low IT confidence. Activities could involve training and calling the participants to clarify or guide them on how to use the internet intervention. Despite the fact that the Space from Depression program involves interactive videos and information on how to explore the program, the supporter could also reinforce and guide the user with this as part of the weekly feedback. Considering these points, the analysis also revealed that participants who completed posttreatment measures showed higher program usage (mean number of logins 11, SD 7.32), compared with those who did not (mean number of logins 3.28, SD 2.76). These outcomes may be reflective of the low IT confidence reported by the sample.
In addition to this inexperience with IT, the intervention was implemented into a sample largely inexperienced in using counseling. Only 20% of the participants in this study had received psychotherapy previously, which could be considered another factor for dropping out. It also highlights the opportunity the study provided for these populations to have access to a treatment program for depression, showing the potential of iCBT to reach different, typically inaccessible, populations.
Satisfaction With Treatment
The results from the satisfaction and user-experience questionnaires indicated that, in general, participants were satisfied with accessing an iCBT intervention. However, a minority of participants felt the treatment did not meet their individual needs, as they found it difficult to get motivated and engage with the program. Flexibility and accessibility were most liked by the participants, which is consistent with previous studies [72,79]. Participants found the intervention easy to use and were happy to access the Web-based treatment. It should be noted that the SAT response rate was low and might be biased toward those who were satisfied with the program and found it helpful.
One of the most significant aspects reported by the participants was presence of a supporter. Having a supporter was valuable to encourage the user to continue with the program and provided guidance and feedback. Some participants reported feeling relieved because of the supporter or having a space to express themselves. All the participants in this study reported positive comments about their supporters, which may reflect the importance of having a trained postgraduate student as an appropriate component to provide suitable feedback to the users. However, a limited number of users share information with their supporter, reflecting a sense of anonymity unique to a Web-based treatment [99].
Participants reported aspects of time as something they least liked about the internet-delivered intervention, which was related to difficulties in completing all the modules in the program. Users reported a lack of time because of academic commitments or personal circumstances. Participants also reported that they did not have enough time to complete the modules in the program and feeling rushed to review the content between sessions. Similar findings have been reported previously [79].
Strengths of the Research
First, the results show that the culturally adapted program Yo puedo sentirme bien/I can feel better was effective in reducing depressive symptoms and comorbid anxiety symptoms with college students in Colombia. The original Space from Depression program has been previously investigated with college students [100] and a community population [59], with significant improvement in depressive symptoms pre- to posttreatment in both populations. Most of the studies of internet-delivered interventions have been studied in HICs, which might not be generalizable to other populations worldwide. Therefore, knowing more of the effectiveness of internet interventions in LMICs may mean that this type of treatment can be an alternative for people who cannot access mental health services because of limited health insurance or personal stigma and is therefore relevant in Colombia [11,101].
Second, despite the high attrition rate found in this study, this type of treatment was an opportunity for students to have access to a psychological intervention. A recent report showed that only a small minority of college students receive adequate treatment for their mental disorders in low-income countries (6%), compared with HICs (23%) [28].
Third, this study adds supporting evidence for using trained student supporters in guided internet-delivered interventions for mild-to-moderate depressive symptoms. Several studies have reported that various levels and type of supporters can achieve positive outcomes in low-intensity internet-delivered interventions for depression [51,85]. Despite the high dropout rate in this study, the student supporters in the study might play an important role in increasing engagement with the program. Corroborating this, qualitative comments by the participants on the SAT were positive about the interaction with their supporters.
Finally, this type of intervention could be delivered through a counseling service with trained students in Colombia. Similarly, it may be employed as a potential alternative in primary care or other populations. Studies have evidenced that internet-delivered interventions might potentially reduce the barriers to treatment access in LMICs [30]. In addition, culturally adapted internet-delivered treatments could reduce cost and possibly personal stigma [102]. Therefore, the study alludes to the potential of a culturally adapted internet-delivered intervention, with support, to accomplish significant outcomes. In locations where mental health services are underdeveloped, health care structures do not exist, or there is a potential to offset risk and escalation of difficulties and benefit from early intervention, such a model of service provision could be feasible [103].
Limitations
A noted limitation is that the study did not include an official depression diagnosis of participants; however, it includes well-established measures of symptom severity that can allow us to establish the efficacy of low-intensity internet-delivered treatments for depression symptoms among college students in Colombia. Another concern is with regard to the problem of missing data.
Owing to the high attrition of research data, it would not have made sense to complete a true ITT analysis including appropriate imputation of missing values. Therefore, our ITT analysis is not as robust as we would have liked, and as a result, caution is advised in any interpretation of the results from this study.
The research attrition was high at posttreatment, and it was even higher at the follow-up. Reminders in the form of emails were sent (maximum four times) and phone calls were made with some participants who provided their contact details (maximum three times), but this did not result in a significant decrease in study dropout/attrition rate. The reasons for this high attrition rate are not entirely known. In addition, the cultural adaptation of the program was not further evaluated after the intervention with the participants, which might have allowed us to assess and identify potential factors related to the adaptation that could have affected dropout.
Future Research
Internet-delivered interventions for depression have shown significant effects post treatment [51], specifically, in high-income Western countries. LMICs around the world have scarce access to mental health services [26]. A strategy to utilize the internet to provide more widely available and low-cost mental health care has vast potential. In addition, internet-delivered treatments could contribute to the globalization of mental health services and psychological interventions, for which cultural adaptation is the key [33].
This study was the first contribution regarding the potential impact of a culturally adapted internet-delivered, low-intensity intervention on depressive symptoms for college students, as compared with a WL control group, in South America. Internet-delivered interventions could be a potential option for delivering evidence-based psychological interventions and may overcome some of the significant barriers to accessing mental health treatment in Colombia. Future research should focus on monitoring participants who drop out prematurely from the study at a follow-up to evaluate the reasons for withdrawal.
This study has demonstrated the potential for internet-delivered interventions to provide satisfactory, acceptable, and effective low-intensity treatments to individuals living with depression in South America. The accessibility and flexibility unique to a Web environment may increase the access to mental health interventions around the world, considering the cultural characteristics of the populations, and this may contribute to decreasing the mental health treatment gap in LMICs.
In future studies, analysis of the central characteristics of the sample, such as age, previous level of depression, familiarity with the technology, previous treatments, and the perceived usefulness of the treatment, among others, could show the extent to which different groups of people might benefit more from this type of Web-based treatment. In attempting to explain and understand the reasons for dropout in the sample, a number of reasons were speculated upon. However, future studies might analyze further the population’s previous knowledge about depression, any associated personal stigma, and their perception of how psychological treatment could help overcome it.
Conclusions
This study showed that the culturally adapted iCBT program Yo puedo sentirme bien/I can feel better could be employed in different cultural groups as a population-level intervention for mild-to-moderate symptoms of depression. Importantly, outcomes from the treatment group were maintained at the follow-up. The research attrition was high at posttreatment and at the follow-up in this study. Future research should focus on monitoring participants who drop out prematurely from the study at a follow-up to evaluate the reasons for withdrawal. The results from this study are encouraging for the implementation of the culturally adapted internet-delivered cognitive behavioral program, Space from Depression, for the treatment of depression symptoms in a culturally different population, helping disseminate evidence-based treatments in LMICs.
Acknowledgments
AS would like to acknowledge the Irish Research Council (IRC) for granting the scholarship [EPSPG/2014/98] under the Enterprise/Academia collaboration scheme. A special acknowledgment is also in place for all the collaborators and supporters in Bogota and Bucaramanga (Colombia) who participated in this study.
Abbreviations
- CBT
cognitive behavioral therapy
- CONSORT
Consolidated Standards of Reporting Trials
- CRQ
Cultural Relevance Questionnaire
- DSM IV
Diagnostic and Statistical Manual of Mental Disorders, fourth edition
- GAD-7
Generalized Anxiety Disorder - 7
- HIC
high-income country
- iCBT
internet-delivered cognitive behavioral therapy
- IRC
Irish Research Council
- IT
information technology
- ITT
intention-to-treat
- LMIC
low- and middle-income country
- LMM
linear mixed model
- PHQ-9
Patient Health Questionnaire - 9
- RCI
reliable change index
- RCT
randomized controlled trial
- REML
restricted maximum likelihood
- SAT
Satisfaction With Treatment
- WL
waiting list
Appendix
Screenshot of the Space from Depression program.
Tools - Space from Depression program.
CONSORT-EHEALTH checklist (V 1.6.1).
Footnotes
Authors' Contributions: AS is the principal investigator of the research. AS, DR, and LT conceptualized the initial trial design. The manuscript was written by AS, with significant contributions and revisions from DR, LT, SC, and LC. SC also contributed to the data analysis. Both MM and YP contributed to the design of the study through their contribution as site-specific investigators, and they reviewed the final version of this manuscript. AS distributed the manuscript to the group for discussion and revisions. The finalized manuscript was agreed upon by all authors.
Conflicts of Interest: AS was the recipient of an IRC scholarship award [EPSPG/2014/98] under the Enterprise/Academia collaboration scheme with SilverCloud Health. From March 2018 to March 2019, AS was a part-time employee in SilverCloud Health. DR is the Chief Science Officer at SilverCloud Health. LT provides a research consultancy for SilverCloud Health. SC worked as a data analyst at SilverCloud Health.
References
- 1.Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Vos T, Whiteford HA. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013 Dec;10(11):e1001547. doi: 10.1371/journal.pmed.1001547. http://dx.plos.org/10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirmayer LJ, Gomez-Carrillo A, Veissière S. Culture and depression in global mental health: an ecosocial approach to the phenomenology of psychiatric disorders. Soc Sci Med. 2017 Jun;183:163–8. doi: 10.1016/j.socscimed.2017.04.034. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–38. doi: 10.1146/annurev-publhealth-031912-114409. http://europepmc.org/abstract/MED/23514317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, de Graaf R, Demyttenaere K, Hu C, Iwata N, Karam AN, Kaur J, Kostyuchenko S, Lépine JP, Levinson D, Matschinger H, Mora ME, Browne MO, Posada-Villa J, Viana MC, Williams DR, Kessler RC. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011 Jul 26;9:90. doi: 10.1186/1741-7015-9-90. https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler. Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Ustün TB, Wang PS. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/S1121189X00001421. http://europepmc.org/abstract/MED/19378696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation . Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organisation; 2017. [Google Scholar]
- 7.Gómez-Restrepo C, Bohórquez A, Masis DP, Laverde JF, Sepúlveda MR, Díaz-Granados N. [The prevalence of and factors associated with depression in Colombia] Rev Panam Salud Publica. 2004 Dec;16(6):378–86. doi: 10.1590/s1020-49892004001200003. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, Sampson N, Andrade LH, de Girolamo G, Demyttenaere K, Haro JM, Karam AN, Kostyuchenko S, Kovess V, Lara C, Levinson D, Matschinger H, Nakane Y, Browne MO, Ormel J, Posada-Villa J, Sagar R, Stein DJ. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depress Anxiety. 2010 May;27(4):351–64. doi: 10.1002/da.20634. http://europepmc.org/abstract/MED/20037917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Üstün Tb, Wang Ps. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiol Psichiatr Soc. 2011 Apr 11;18(1):23–33. doi: 10.1017/S1121189X00001421. https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/global-burden-of-mental-disorders-an-update-from-the-who-world-mental-health-wmh-surveys/FCE4DE10C9FB1A9FFDDDBA3C5264F445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan American Health Organization . The Burden of Mental Disorders in the Region of the Americas, 2018. Washington, DC: PAHO; 2018. [Google Scholar]
- 11.Ministry of Health . National Mental Health survey. Bogota, Colombia: Ministry of Health; 2015. pp. 1–344. [Google Scholar]
- 12.Ministry of Health and Social Protection. 2017. [2017-03-01]. Boletín de salud mental Depresión Subdirección de Enfermedades No Transmisibles. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENT/boletin-depresion-marzo-2017.pdf.
- 13.Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. J Affect Disord. 2014 Jan;152-154:45–51. doi: 10.1016/j.jad.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. J Am Med Assoc. 2016 Dec 6;316(21):2214–36. doi: 10.1001/jama.2016.17324. http://europepmc.org/abstract/MED/27923088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sargent JT, Crocker J, Luhtanen RK. Contingencies of self–worth and depressive symptoms in college students. J Soc Clinical Psychol. 2006;25(6):628–46. doi: 10.1521/jscp.2006.25.6.628. [DOI] [Google Scholar]
- 16.Rankin JA, Paisley CA, Mulla MM, Tomeny TS. Unmet social support needs among college students: relations between social support discrepancy and depressive and anxiety symptoms. J Couns Psychol. 2018 Jul;65(4):474–89. doi: 10.1037/cou0000269. [DOI] [PubMed] [Google Scholar]
- 17.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. 2006 May;81(4):354–73. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Shadowen NL, Williamson AA, Guerra NG, Ammigan R, Drexler ML. Prevalence and correlates of depressive symptoms among international students: implications for university support offices. J Int Stud. 2019;9(1):129–49. doi: 10.32674/jis.v9i1.277. [DOI] [Google Scholar]
- 19.Cuijpers P, Cristea IA, Ebert DD, Koot HM, Auerbach RP, Bruffaerts R, Kessler RC. Psychological treatment of depression in college students: a metaanalysis. Depress Anxiety. 2016 May;33(5):400–14. doi: 10.1002/da.22461. http://europepmc.org/abstract/MED/26682536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013 Mar;47(3):391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Solar FC, Alvial SW, Aro DM, Bonifetti DA, Hernández M, Rodríguez C. Problemas de Salud Mental en Estudiantes de la Universidad de Concepción. Ter Psicol. 2007;25(2):105–12. doi: 10.4067/S0718-48082007000200001. [DOI] [Google Scholar]
- 22.Melo-Carrillo A, van Oudenhove L, Lopez-Avila A. Depressive symptoms among Mexican medical students: high prevalence and the effect of a group psychoeducation intervention. J Affect Disord. 2012 Mar;136(3):1098–103. doi: 10.1016/j.jad.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 23.Morales CF, Pérez VP, León SO, Medrano AJ, Aguilar ME, Guevara-Guzmán R. Síntomas depresivos y rendimiento escolar en estudiantes de Medicina. Salud Ment. 2013;36(1):59–65. doi: 10.17711/SM.0185-3325.2013.008. [DOI] [Google Scholar]
- 24.Nogueira-Martins LA, Neto RF, Macedo PM, Cítero VA, Mari J. The mental health of graduate students at the Federal University of São Paulo: a preliminary report. Braz J Med Biol Res. 2004 Oct;37(10):1519–24. doi: 10.1590/s0100-879x2004001000011. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-879X2004001000011&lng=en&nrm=iso&tlng=en. [DOI] [PubMed] [Google Scholar]
- 25.Arrivillaga-Quintero M, Cortés-Garcia C, Goicochea-Jiménez Vl. Caracterización de la Depresión en Jóvenes Universitarios. Characterization of Depression in University Young People. Universitas Psychologica. 2004;3(1):17–26. https://www.redalyc.org/pdf/647/64730103.pdf. [Google Scholar]
- 26.Richards D, Sanabria AS. Point-prevalence of depression and associated risk factors. J Psychol. 2014;148(3):305–26. doi: 10.1080/00223980.2013.800831. [DOI] [PubMed] [Google Scholar]
- 27.Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, Sammut S. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. 2015 Mar 1;173:90–6. doi: 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- 28.Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, Kessler RC, Liu H, Mortier P, Nock MK, Pinder-Amaker S, Sampson NA, Aguilar-Gaxiola S, Al-Hamzawi A, Andrade LH, Benjet C, Caldas-de-Almeida JM, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, Haro JM, Karam EG, Kiejna A, Kovess-Masfety V, Lee S, McGrath JJ, O'Neill S, Pennell B, Scott K, Ten Have M, Torres Y, Zaslavsky AM, Zarkov Z, Bruffaerts R. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016 Oct;46(14):2955–70. doi: 10.1017/S0033291716001665. http://europepmc.org/abstract/MED/27484622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodriguez J. La atención de Salud Mental en América Latina y el caribe. Rev Psiquiatr Urug. 2007;71(2):117–24. http://www.spu.org.uy/revista/dic2007/04_asm.pdf. [Google Scholar]
- 30.Cuijpers P, Karyotaki E, Reijnders M, Purgato M, Barbui C. Psychotherapies for depression in low- and middle-income countries: a meta-analysis. World Psychiatry. 2018 Mar;17(1):90–101. doi: 10.1002/wps.20493. doi: 10.1002/wps.20493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vally Z, Maggott C. Evaluating the outcome of cultural adaptations of cognitive-behavioural therapy for adult depression: a meta-analysis of treatment studies in developing countries. Int J Adv Counsel. 2015;37(4):293–304. doi: 10.1007/s10447-015-9244-5. [DOI] [Google Scholar]
- 32.Castro-Camacho L, Moreno JD, Naismith I. Contextual adaptation of the unified protocol for the transdiagnostic treatment of emotional disorders in victims of the armed conflict in colombia: a case study. Cogn Behav Pract. 2018;26(2):366–80. doi: 10.1016/j.cbpra.2018.09.002. [DOI] [Google Scholar]
- 33.Arjadi R, Nauta MH, Chowdhary N, Bockting CLH. A systematic review of online interventions for mental health in low and middle income countries: a neglected field. Glob Ment Health (Camb) 2015;2:e12. doi: 10.1017/gmh.2015.10. http://europepmc.org/abstract/MED/28596860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martínez P, Rojas G, Martínez V, Lara MA, Pérez JC. Internet-based interventions for the prevention and treatment of depression in people living in developing countries: A systematic review. J Affect Disord. 2018 Jul;234:193–200. doi: 10.1016/j.jad.2018.02.079. [DOI] [PubMed] [Google Scholar]
- 35.Colombia TIC. 2015. [2019-10-31]. Boletín trimestral de las TIC - Cifras cuarto trimestre de 2015 https://colombiatic.mintic.gov.co/679/w3-article-15179.html.
- 36.Karyotaki E, Smit Y, Holdt Henningsen K, Huibers M, Robays J, de Beurs D, Cuijpers P. Combining pharmacotherapy and psychotherapy or monotherapy for major depression? A meta-analysis on the long-term effects. J Affect Disord. 2016 May;194:144–52. doi: 10.1016/j.jad.2016.01.036. [DOI] [PubMed] [Google Scholar]
- 37.Karyotaki E, Smit Y, de Beurs DP, Henningsen KH, Robays J, Huibers MJ, Weitz E, Cuijpers P. The long-term efficacy of acute-phase psychotherapy for depression: a meta-analysis of randomized trials. Depress Anxiety. 2016 May;33(5):370–83. doi: 10.1002/da.22491. [DOI] [PubMed] [Google Scholar]
- 38.Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. 2013 Jul;12(2):137–48. doi: 10.1002/wps.20038. doi: 10.1002/wps.20038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cuijpers P, Andersson G, Donker T, van Straten A. Psychological treatment of depression: results of a series of meta-analyses. Nord J Psychiatry. 2011 Dec;65(6):354–64. doi: 10.3109/08039488.2011.596570. [DOI] [PubMed] [Google Scholar]
- 40.Cuijpers P, van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol. 2008 Dec;76(6):909–22. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- 41.Boumparis N, Karyotaki E, Kleiboer A, Hofmann SG, Cuijpers P. Corrigendum to 'The effect of psychotherapeutic interventions on positive and negative affect in depression: A systematic review and meta-analysis'. J Affect Disord. 2017 Apr 15;213:223. doi: 10.1016/j.jad.2017.01.040. [DOI] [PubMed] [Google Scholar]
- 42.Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry. 2013 Jul;58(7):376–85. doi: 10.1177/070674371305800702. [DOI] [PubMed] [Google Scholar]
- 43.Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, Hollon SD. Component studies of psychological treatments of adult depression: a systematic review and meta-analysis. Psychother Res. 2019 Jan;29(1):15–29. doi: 10.1080/10503307.2017.1395922. [DOI] [PubMed] [Google Scholar]
- 44.Titov N. Internet-delivered psychotherapy for depression in adults. Curr Opin Psychiatry. 2011 Jan;24(1):18–23. doi: 10.1097/YCO.0b013e32833ed18f. [DOI] [PubMed] [Google Scholar]
- 45.Ritterband LM, Thorndike F. Internet interventions or patient education web sites? J Med Internet Res. 2006 Oct 29;8(3):e18; author reply e19. doi: 10.2196/jmir.8.3.e18. https://www.jmir.org/2006/3/e18/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Institute for Health and Care Excellence National Institute for Health and Care Excellence. 2009. [2019-10-31]. Depression in Adults: Recognition and Management. https://www.nice.org.uk/guidance/cg90/resources/depression-in-adults-recognition-and-management-pdf-975742638037.
- 47.Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res. 2012 Dec;12(6):745–64. doi: 10.1586/erp.12.67. [DOI] [PubMed] [Google Scholar]
- 48.Spek V, Nyklícek I, Smits N, Cuijpers P, Riper H, Keyzer J, Pop V. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med. 2007 Dec;37(12):1797–806. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 49.Morgan AJ, Jorm AF, Mackinnon AJ. Protocol for a randomised controlled trial investigating self-help email messages for sub-threshold depression: the Mood Memos study. Trials. 2011 Jan 13;12:11. doi: 10.1186/1745-6215-12-11. https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ebert D, Berking M, Cuijpers P, Lehr D, Pörtner M, Baumeister H. Increasing the acceptance of internet-based mental health interventions in primary care patients with depressive symptoms. A randomized controlled trial. J Affect Disord. 2015 May 1;176:9–17. doi: 10.1016/j.jad.2015.01.056. [DOI] [PubMed] [Google Scholar]
- 51.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jul;32(4):329–42. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 52.Ebert D, Tarnowski T, Gollwitzer M, Sieland B, Berking M. A transdiagnostic internet-based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom. 2013;82(4):246–56. doi: 10.1159/000345967. [DOI] [PubMed] [Google Scholar]
- 53.Montero-Marín J, Araya R, Pérez-Yus MC, Mayoral F, Gili M, Botella C, Baños R, Castro A, Romero-Sanchiz P, López-Del-Hoyo Y, Nogueira-Arjona R, Vives M, Riera A, García-Campayo J. An internet-based intervention for depression in primary care in Spain: a randomized controlled trial. J Med Internet Res. 2016 Aug 26;18(8):e231. doi: 10.2196/jmir.5695. https://www.jmir.org/2016/8/e231/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lara MA, Tiburcio M, Abrego AA, Sánchez-Solís A. A four-year experience with a web-based self-help intervention for depressive symptoms in Mexico. Rev Panam Salud Publica. 2014;35(5-6):399–406. [PubMed] [Google Scholar]
- 55.Espinosa HD, Carrasco Á, Moessner M, Cáceres C, Gloger S, Rojas G, Perez JC, Vanegas J, Bauer S, Krause M. Acceptability study of 'Ascenso': an online program for monitoring and supporting patients with depression in Chile. Telemed J E Health. 2016 Jul;22(7):577–83. doi: 10.1089/tmj.2015.0124. [DOI] [PubMed] [Google Scholar]
- 56.Schröder J, Berger T, Westermann S, Klein JP, Moritz S. Internet interventions for depression: new developments. Dialogues Clin Neurosci. 2016 Jun;18(2):203–12. doi: 10.31887/DCNS.2016.18.2/jschroeder. http://europepmc.org/abstract/MED/27489460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.World Health Organisation. [2019-10-31]. Comprehensive Mental Health Action Plan 2013–2020. https://www.who.int/mental_health/action_plan_2013/en/
- 58.Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res. 2017 Apr 27;19(4):e136. doi: 10.2196/jmir.6731. https://www.jmir.org/2017/4/e136/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Richards D, Timulak L, O'Brien E, Hayes C, Vigano N, Sharry J, Doherty G. A randomized controlled trial of an internet-delivered treatment: its potential as a low-intensity community intervention for adults with symptoms of depression. Behav Res Ther. 2015 Dec;75:20–31. doi: 10.1016/j.brat.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 60.Salamanca-Sanabria. Richards. Timulak L. Adapting an internet-delivered intervention for depression for a Colombian college student population: an illustration of an integrative empirical approach. Internet Interv. 2019 Mar;15:76–86. doi: 10.1016/j.invent.2018.11.005. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(18)30035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bernal G, Domenech-Rodríguez M. Cultural Adaptations: Tools for Evidence-Based Practice With Diverse Populations. Washington, DC, US: American Psychological Association; 2012. [Google Scholar]
- 62.Helms JE. An examination of the evidence in culturally adapted evidence-based or empirically supported interventions. Transcult Psychiatry. 2015 May;52(2):174–97. doi: 10.1177/1363461514563642. [DOI] [PubMed] [Google Scholar]
- 63.Salamanca-Sanabria A, Richards D, Timulak L, Castro-Camacho L, Mojica-Perilla M, Parra-Villa Y. Assessing the efficacy of a culturally adapted cognitive behavioural internet-delivered treatment for depression: protocol for a randomised controlled trial. BMC Psychiatry. 2018 Feb 27;18(1):53. doi: 10.1186/s12888-018-1634-x. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-018-1634-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Richards D, Timulak L, Hevey D. A comparison of two online cognitive-behavioural interventions for symptoms of depression in a student population: The role of therapist responsiveness. Counsel Psychother Res. 2013;13(3):184–93. doi: 10.1080/14733145.2012.733715. [DOI] [Google Scholar]
- 65.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9):509–15. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- 66.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Oct;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2001&volume=16&issue=9&spage=606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Merz EL, Malcarne VL, Roesch SC, Riley N, Sadler GR. A multigroup confirmatory factor analysis of the Patient Health Questionnaire-9 among English- and Spanish-speaking Latinas. Cultur Divers Ethnic Minor Psychol. 2011 Jul;17(3):309–16. doi: 10.1037/a0023883. http://europepmc.org/abstract/MED/21787063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007 Dec;22(11):1596–602. doi: 10.1007/s11606-007-0333-y. http://europepmc.org/abstract/MED/17874169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, Herzberg PY. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74. doi: 10.1097/mlr.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 70.Kroenke K, Spitzer RL, Williams JB, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345–59. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 71.García-Campayo J, Zamorano E, Ruiz MA, Pardo A, Pérez-Páramo M, López-Gómez V, Freire O, Rejas J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes. 2010 Jan 20;8:8. doi: 10.1186/1477-7525-8-8. https://hqlo.biomedcentral.com/articles/10.1186/1477-7525-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Richards D, Timulak L. Satisfaction with therapist-delivered vs self-administered online cognitive behavioural treatments for depression symptoms in college students. Br J Guid Counc. 2013;41(2):193–207. doi: 10.1080/03069885.2012.726347. [DOI] [Google Scholar]
- 73.Field A. Discovering Statistics using SPSS. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 74.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Soft. 2014;67(1) doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- 75.GitHub. [2019-11-06]. lme4/lme4. https://github.com/lme4/lme4/
- 76.West BT, Welch KB, Galecki AT. Linear Mixed Models: A Practical Guide Using Statistical Software. Boca Raton, FL: CRC Press; 2014. [Google Scholar]
- 77.Kuznetsova A, Brockhoff PB, Christensen RH. lmerTest package: tests in linear mixed effects models. J Stat Soft. 2017;82(13) doi: 10.18637/jss.v082.i13. [DOI] [Google Scholar]
- 78.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Second Edition. Hillsdale, NJ: Laurence Erlbaum Associates; 1988. [Google Scholar]
- 79.Richards D, Murphy T, Viganó N, Timulak L, Doherty G, Sharry J, Hayes C. Acceptability, satisfaction and perceived efficacy of 'Space from Depression' an internet-delivered treatment for depression. Internet Interv. 2016 Oct;5:12–22. doi: 10.1016/j.invent.2016.06.007. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(16)30034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Little RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- 81.Choi I, Zou J, Titov N, Dear DB, Li S, Johnston L, Andrews G, Hunt C. Culturally attuned Internet treatment for depression amongst Chinese Australians: a randomised controlled trial. J Affect Disord. 2012 Mar;136(3):459–68. doi: 10.1016/j.jad.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 82.Kayrouz R, Dear BF, Johnston L, Gandy M, Fogliati VJ, Sheehan J, Titov N. A feasibility open trial of guided internet-delivered cognitive behavioural therapy for anxiety and depression amongst Arab Australians. Internet Interv. 2015;2(1):32–8. doi: 10.1016/j.invent.2014.12.001. [DOI] [Google Scholar]
- 83.Ince BU, Cuijpers P, van 't Hof E, van Ballegooijen W, Christensen H, Riper H. Internet-based, culturally sensitive, problem-solving therapy for Turkish migrants with depression: randomized controlled trial. J Med Internet Res. 2013 Oct 11;15(10):e227. doi: 10.2196/jmir.2853. https://www.jmir.org/2013/10/e227/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Andersson G. Internet interventions: past, present and future. Internet Interv. 2018 Jul;12:181–8. doi: 10.1016/j.invent.2018.03.008. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(18)30015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wells MJ, Owen JJ, McCray LW, Bishop LB, Eells TD, Brown GK, Richards D, Thase ME, Wright JH. Computer-assisted cognitive-behavior therapy for depression in primary care: systematic review and meta-analysis. Prim Care Companion CNS Disord. 2018 Mar 1;20(2) doi: 10.4088/PCC.17r02196. http://www.psychiatrist.com/PCC/article/Pages/2018/v20n02/17r02196.aspx. [DOI] [PubMed] [Google Scholar]
- 86.Wright JH, Owen JJ, Richards D, Eells TD, Richardson T, Brown GK, Barrett M, Rasku MA, Polser G, Thase ME. Computer-assisted cognitive-behavior therapy for depression: a systematic review and meta-analysis. J Clin Psychiatry. 2019 Mar 19;80(2) doi: 10.4088/JCP.18r12188. http://www.psychiatrist.com/JCP/article/Pages/2019/v80/18r12188.aspx. [DOI] [PubMed] [Google Scholar]
- 87.Kayrouz R, Dear BF, Karin E, Fogliati VJ, Titov N. A pilot study of a clinician-guided internet-delivered cognitive behavioural therapy for anxiety and depression among Arabs in Australia, presented in both English and Arabic languages. Internet Interv. 2016 Oct;5:5–11. doi: 10.1016/j.invent.2016.06.002. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(16)30015-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011 Aug 5;13(3):e52. doi: 10.2196/jmir.1772. https://www.jmir.org/2011/3/e52/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Titov N, Andrews G, Davies M, McIntyre K, Robinson E, Solley K. Internet treatment for depression: a randomized controlled trial comparing clinician vs technician assistance. PLoS One. 2010 Jul 8;5(6):e10939. doi: 10.1371/journal.pone.0010939. http://dx.plos.org/10.1371/journal.pone.0010939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kleinman A. Culture and depression. N Engl J Med. 2004 Oct 2;351(10):951–3. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- 91.Alarcón ME, Mojica NF, Serrano LG. Prevalencia de consumo de alcohol en estudiantes universitarios / Prevalence of alcohol consumption in university students. RIDE Revista Iberoamericana para la Investigación y el Desarrollo Educativo. 2016;6(12):491–504. doi: 10.23913/ride.v6i12.213. [DOI] [Google Scholar]
- 92.Richards D, Richardson T, Timulak L, Viganò N, Mooney J, Doherty G, Hayes C, Sharry J. Predictors of depression severity in a treatment-seeking sample. Int J Clin Health Psychol. 2016;16(3):221–9. doi: 10.1016/j.ijchp.2016.02.001. https://linkinghub.elsevier.com/retrieve/pii/S1697-2600(16)30001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Meyer B, Berger T, Caspar F, Beevers C, Andersson G, Weiss M. Effectiveness of a novel integrative online treatment for depression (Deprexis): randomized controlled trial. J Med Internet Res. 2009 May 11;11(2):e15. doi: 10.2196/jmir.1151. https://www.jmir.org/2009/2/e15/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Eysenbach G. The law of attrition. J Med Internet Res. 2005 Mar 31;7(1):e11. doi: 10.2196/jmir.7.1.e11. https://www.jmir.org/2005/1/e11/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Henkemans OAB, Rogers WA, Dumay AMC. Personal characteristics and the law of attrition in randomized controlled trials of eHealth services for self-care. Gerontechnology. 2011;10(3):157–68. doi: 10.4017/gt.2011.10.3.004.00. [DOI] [Google Scholar]
- 96.Christensen H, Mackinnon A. The law of attrition revisited. J Med Internet Res. 2006 Oct 29;8(3):e20; author reply e21. doi: 10.2196/jmir.8.3.e20. https://www.jmir.org/2006/3/e20/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Meyer B, Bierbrodt J, Schröder J, Berger T, Beevers CG, Weiss M, Jacob G, Späth C, Andersson G, Lutz W, Hautzinger M, Löwe B, Rose M, Hohagen F, Caspar F, Greiner W, Moritz S, Klein JP. Effects of an Internet intervention (Deprexis) on severe depression symptoms: Randomized controlled trial. Internet Interv. 2015;2(1):48–59. doi: 10.1016/j.invent.2014.12.003. [DOI] [Google Scholar]
- 98.Sieverink F, Kelders SM, van Gemert-Pijnen JE. Clarifying the concept of adherence to eHealth technology: systematic review on when usage becomes adherence. J Med Internet Res. 2017 Dec 6;19(12):e402. doi: 10.2196/jmir.8578. https://www.jmir.org/2017/12/e402/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Efstathiou G. Students’ psychological web consulting: function and outcome evaluation. Br J Guid Counc. 2009;37(3):243–55. doi: 10.1080/03069880902956983. [DOI] [Google Scholar]
- 100.Doherty G, Coyle D, Sharry J. Engagement With Online Mental Health Interventions: An Exploratory Clinical Study of a Treatment for Depression. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI'12; May 5-10, 2012; Austin, Texas, USA. 2012. pp. 1421–30. https://dl.acm.org/citation.cfm?doid=2207676.2208602. [DOI] [Google Scholar]
- 101.Richards D, Timulak L, Doherty G, Sharry J, Colla A, Joyce C, Hayes C. Internet-delivered treatment: its potential as a low-intensity community intervention for adults with symptoms of depression: protocol for a randomized controlled trial. BMC Psychiatry. 2014 May 21;14:147. doi: 10.1186/1471-244X-14-147. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-14-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mohr DC, Ho J, Duffecy J, Baron KG, Lehman KA, Jin L, Reifler D. Perceived barriers to psychological treatments and their relationship to depression. J Clin Psychol. 2010 May;66(4):394–409. doi: 10.1002/jclp.20659. http://europepmc.org/abstract/MED/20127795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Richards D, Duffy D, Burke J, Anderson M, Connell S, Timulak L. Supported internet-delivered cognitive behavior treatment for adults with severe depressive symptoms: a secondary analysis. JMIR Ment Health. 2018 Oct 2;5(4):e10204. doi: 10.2196/10204. https://mental.jmir.org/2018/4/e10204/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Screenshot of the Space from Depression program.
Tools - Space from Depression program.
CONSORT-EHEALTH checklist (V 1.6.1).


