Abstract
INTRODUCTION:
Colorectal cancer (CRC) is a major cause of cancer-related morbidity and mortality in the United States. Although various interventions have improved screening rates, they often require abundant resources and can be difficult to implement. Social psychology and behavioral economics principles offer an opportunity for low-cost and easy-to-implement strategies but are less common in clinical settings.
METHODS:
We randomized 2,000 patients aged 50–75 years eligible for CRC screening to one of the 2 mailed interventions: a previously used text-based letter describing and offering fecal immunochemical testing (FIT) and colonoscopy (usual care arm); or a letter leveraging social psychology and behavioral economics principles (e.g., implied scarcity and choice architecture), minimal text, and multiple images to offer FIT and colonoscopy (intervention arm). We compared total screening uptake, FIT uptake, and colonoscopy uptake at 1-month intervals in each group.
RESULTS:
There were 1,882 patients included in the final analysis. The mean age was 69.3 years, and baseline characteristics in the 2 groups were similar. Screening completion at 26 weeks was 19.5% in the usual care arm (16.3% FIT vs 3.2% colonoscopy, P < 0.01) and 24.1% in the intervention arm (22.1% FIT vs 2.0% colonoscopy, P < 0.01) (P = 0.02).
DISCUSSION:
Among primary care patients aged 50–75 years in an academic setting, mailed CRC outreach employing social psychology and behavioral economics principles led to a higher participation in CRC screening than usual care mailed outreach.
TRANSLATIONAL IMPACT:
Mailed interventions to increase CRC screening should incorporate social psychology and behavioral economics principles to improve participation.
INTRODUCTION
Colorectal cancer (CRC) is a major cause of cancer-related morbidity and is the second most common cause of cancer-related mortality in the United States (1–4). Despite guidelines promoting universal CRC screening, national screening rates remain suboptimal—well under the goal of 80% set by the National Colorectal Cancer Roundtable (5). Screening programs have effectively improved CRC screening rates and appear to be most effective when they include patient-, provider-, and system-level interventions (6). Many successful patient-directed interventions involve the use of verbal communication, image, and media; yet, approach and optimal use of communication have not been well-characterized in the medical literature.
Behavioral economics and social psychology offer extensive literature on how to build highly persuasive communications (7–14). The term choice architecture has been coined to describe the concept that how messages are framed can have a significant impact on the outcome achieved (7,8). Effective messaging techniques in a variety of domains have included the use of social norms (9), default options (10), outcome framing (11), implied scarcity (12), and implied ownership or endowment (13,14) among others. If effective in changing patient behavior in medical environments, minor changes in messaging techniques potentially represent an inexpensive and easy-to-implement opportunity to modify patient behavior and for quality improvement interventions.
The application of these methods to healthcare and quality improvement has begun to garner attention, including its application to cancer screening (15,16). Examples of the successful use of these principles include message framing to increase sunscreen application for skin cancer prevention and automatic defaults to increase organ donations and reduce opiate prescribing (17–19). There are very few examples in CRC screening. Opt out has been effective in increasing screening rates when paired with mailed fecal immunochemical testing (FIT) kits (20); however, other attempts to incorporate behavioral science principles have been less impactful (21–23).
Given the success of behavioral economics and social psychology principles in other medical disciplines and their potential to increase CRC screening uptake without increasing cost, we aimed to incorporate targeted techniques that leverage these behavioral principles to increase participation in a mailed CRC screening outreach program in a large, academic center. We focused on techniques that did not increase cost per patient and that have previously been successful in clinical care. To evaluate the effectiveness of these strategies, we compared the screening outcomes for unscreened patients randomized to either our intervention or to usual care in a quality improvement initiative.
METHODS
Setting and population
University of California, Los Angeles (UCLA) Health is a large, integrated academic medical center with a defined primary care population and robust referral-based care. The primary care population includes over 350,000 patients who receive primary care services from a primary care physician at UCLA. CRC screening is primarily performed in the primary care setting, and patients are screened by one of the several following methods: FIT, colonoscopy, computed tomography (CT) colonography, flexible sigmoidoscopy (FS), or FIT-DNA. For eligible patients, the primary care provider (PCP) will place an electronic request for the desired screening method. When ordered, FIT kits are provided directly to patients by the PCP office staff or the UCLA laboratory and returned in a prepaid and addressed envelope to the UCLA laboratory. When colonoscopy is requested, patients are contacted by schedulers to choose a procedure date. If not reached by phone, schedulers leave a voice message prompting the patient to call back. If a callback is not received, additional efforts include a second phone call and an electronic message to the PCP to rerefer the patient for colonoscopy when appropriate.
In addition to screening initiated by PCPs or their offices at the time of a patient encounter, UCLA Health designed and implemented, in 2015, a FIT Kit mailing program for the managed care primary care population overdue for screening. The intervention included a standard text-based letter describing and offering FIT, colonoscopy, and FS along with a preaddressed PolymedCo OC-Auto FIT-CHEK kit with instructions. The mailing was sent to all managed care patients aged 51–75 years who were overdue for screening according to electronic health record data and consistent with the National Committee for Quality Assurance Healthcare Effectiveness Data and Information Set (HEDIS) specifications (24).
Subject selection and randomization
With assistance from the UCLA Value Analytics team, we used electronic medical records, billings data, and claims data to identify a cohort of managed care patients due for CRC screening in March 2017. Like the current FIT kit mailing program, we targeted patients within the managed care population aged 51–75 years who were not up-to-date with screening, defined by a lack of FIT in the past year, FS in the past 5 years, colonoscopy in the past 10 years, CT colonography during the previous 5 years, or FIT-DNA test during the previous 3 years. Exclusion criteria included a personal history of CRC and previous total colectomy. Patients also required a valid mailing address to be included.
Randomization took place in May 2017. We used simple randomization with R software (version 3.4.3, 2017) to assign 2,000 subjects to one of the 2 intervention arms: (i) the standard text-based letter to encourage CRC screening participation (usual care group), and (ii) a new letter leveraging social psychology and behavioral economics principles (intervention group).
Intervention
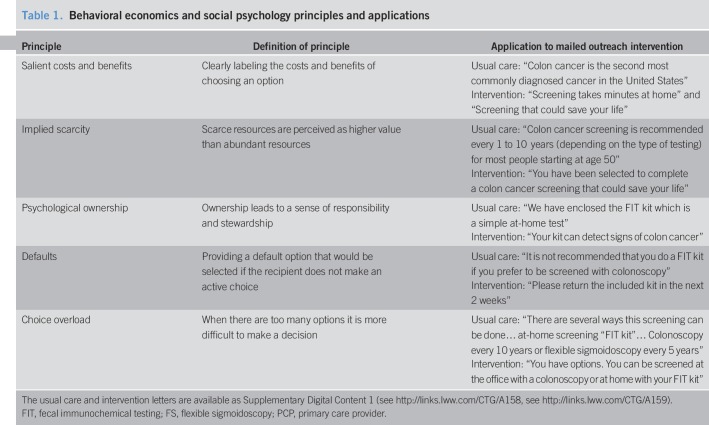
The usual care group received the traditional FIT kit mailing program letter. This letter explains the benefits of screening for CRC and includes a general invitation to participate in screening. The letter is text based without images, offers FIT, colonoscopy, and FS, and provides an opportunity to mail in medical records if screening was performed outside UCLA Health.
Like the usual care group, the intervention group received a letter explaining the benefits of screening and a general invitation to participate in CRC screening; however, multiple messaging techniques from the behavioral science literature were incorporated to increase participation: choice overload, defaults, implied scarcity, psychological ownership, and salient costs and benefits (Table 1). The letter reduced the number of screening options to avoid choice overload and instructed patients to return the FIT within 2 weeks, providing them with a default response. We used implied scarcity by encouraging patients that the receipt of a FIT was a unique opportunity (“you have been selected”) and psychological ownership of FIT was encouraged by changing all mentions of “the FIT kit” to “your FIT kit.” Finally, the letter framed the salient costs and benefits of screening specifically to the patient (i.e., cost as time to complete the FIT; benefit as longer life) rather than highlighting the more general benefits of early cancer diagnosis from the perspective of the larger U.S. population.
Table 1.
Behavioral economics and social psychology principles and applications
Usual care and intervention mailings included identical FIT kits and details about how to schedule colonoscopy if preferred. FIT kits were accompanied by a one-page handout with simple pictures on how to complete the kit, a prepaid return envelope for the kit, and a one-page form to report non-UCLA screening results. All FIT kit mailers contained a postal label for return to the UCLA clinical laboratory and were processed as per the manufacturer protocol. For positive results, a population health patient coordinator notified the patient's PCP of the result, and the PCP was responsible for generating a referral for diagnostic colonoscopy.
Outcomes and variables
Our primary outcome was CRC screening uptake. We determined the screening uptake for each one-month interval between June 22, 2017 and November 22, 2017. Patients were considered screened if they completed FIT, FS, colonoscopy, CT colonography, or FIT-DNA consistent with HEDIS.
For each participant, we also extracted demographic data from the electronic health record, including age at time of randomization, sex, race, and ethnicity. We combined the concepts of race and ethnicity into one composite variable called race/ethnicity with 5 mutually exclusive categories: non-Hispanic white (white), non-Hispanic black (black), Hispanic, Asian, other, and unknown.
Statistical analysis
We used frequencies and means to summarize demographic data for the cohort and each quality improvement (QI) arm. We then used the Student's t test and χ2 test to compare continuous and categorical demographic variables, respectively, across QI arms. For the primary outcome, we calculated the overall CRC screening completion rate and for each group at each time interval. We used χ2 tests to compare screening completion rates and uptake of FIT and colonoscopy across arms. A P-value of 0.05 was considered statistically significant. All analyses were performed with Stata/SE version 14.1 (StataCorp LP, College Station, TX). The UCLA institutional review board deemed our work exempt systems improvement consistent with ongoing hospital QI efforts.
RESULTS
Patient characteristics
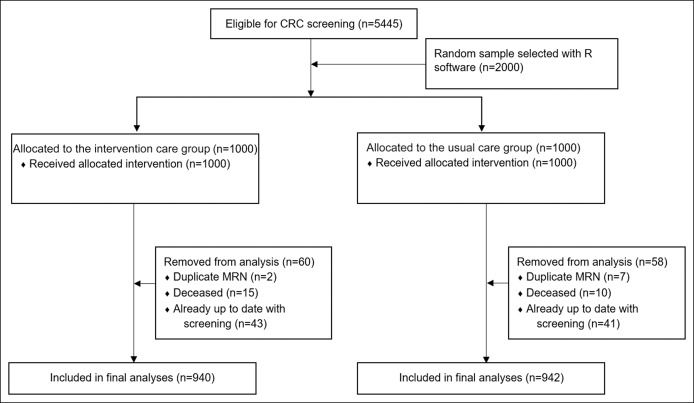
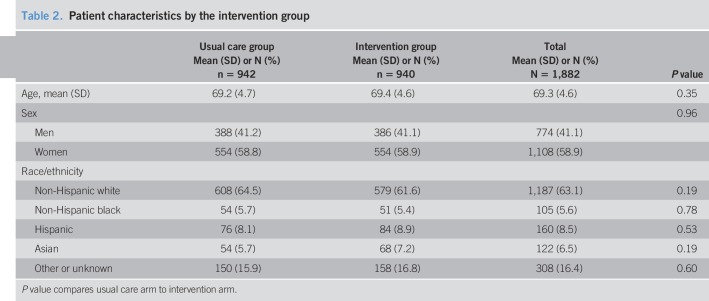
There were 1,882 patients included in our analyses. We excluded 118 individuals for the following reasons: duplicate patients (n = 9), patients completed screening in the interval between patient list acquisition and randomization (n = 84), and patients deceased (n = 25) (Figure 1). The mean age was 69.3 years, and 41.1% were men. The population was racially/ethnically diverse with 63.1% whites, 5.6% blacks, 8.5% Hispanics, and 6.5% Asians. Baseline characteristics were similar in the 2 groups (Table 2).
Figure 1.
Patient flow chart. CRC, colorectal cancer; MRN, medical record number.
Table 2.
Patient characteristics by the intervention group
Screening completion
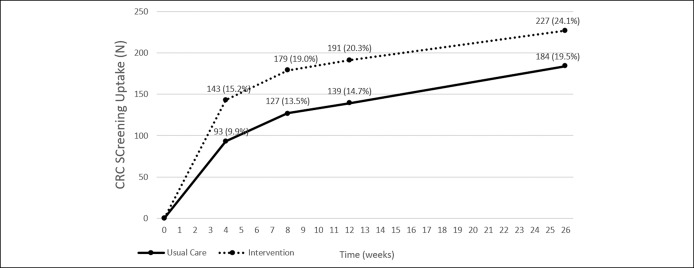
Overall screening uptake was significantly higher in the intervention arm at each time interval (Figure 2). At month 1, uptake was 9.9% in the usual care arm and 15.2% in the intervention arm (P < 0.01). At month 6, uptake was 19.5% in the usual care arm and 24.1% in the intervention arm (P = 0.02). There were no statistically significant differences in uptake by race/ethnicity, sex, or age (Table 2).
Figure 2.
Overall CRC screening uptake (FIT plus colonoscopy) in each study arm. CRC, colorectal cancer; FIT, fecal immunochemical testing.
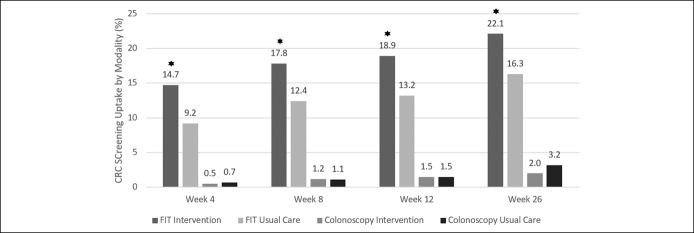
Screening modalities
Patient participation in FIT was higher than participation in colonoscopy in both arms at each time interval (Figure 3). Participation in FIT also was higher in the intervention group than in the usual care group at each time interval (Figure 3). At 1 month, the FIT screening rate was 9.2% in the usual care group and 14.7% in the intervention group (P < 0.01). Uptake improved in both groups over time; FIT uptake was 16.3% in the usual care group and 22.1% in the intervention group at 6 months (P < 0.01) (Figure 3). A higher proportion of individuals chose FIT in the intervention group (91.7%) than in the usual care group (83.6%) (P = 0.01). There were 15 (9.7%) positive FIT results in the usual care arm, and 3 (20%) underwent subsequent colonoscopy by the end of the study period. There were 10 (4.8%) positive FIT results in the intervention arm; 4 (40%) underwent colonoscopy by the end of the study period.
Figure 3.
Overall CRC screening uptake by modality in each study arm. *Denotes a significant difference in FIT uptake between intervention and usual care groups. CRC, colorectal cancer; FIT, fecal immunochemical testing.
Participation in colonoscopy was similar in both groups (Figure 3). At 1 month, the colonoscopy screening rate was 0.7% in the usual care group vs 0.5% in the intervention group (P = 0.57). Uptake improved in both groups over time, and the colonoscopy screening rate was 3.2% in the usual care group vs 2.0% in the intervention group at 6 months (P = 0.10) (Figure 3). No patients underwent screening with FS, CT colonography, or FIT-DNA.
DISCUSSION
We found that the use of behavioral principles aimed to improve patient participation in a mailed CRC screening outreach program led to higher screening uptake than our traditional mailed outreach. Participation in FIT was higher than participation in colonoscopy in both arms, and screening by colonoscopy was similar in the 2 groups. The proportion of patients that choose FIT as a screening modality was higher in the intervention group than in the usual care group.
The composition changes to the mailed outreach incorporated several principles from social psychology and behavioral economics literature. Research on default options suggests that individuals are more likely to comply with a standard course of action rather than actively choose from several competing options (25,26). Inaction in the face of multiple options is further compounded by choice overload (27), which we minimized in our intervention letter by emphasizing FIT as the default option and offering fewer screening modalities. Procrastination to complete a task is reduced when short time windows are provided as specific deadlines (28,29). Other messaging options that prompt faster action are those that make salient the personal costs and benefits of performing the prescribed action, such as highlighting the possible life-saving benefits of completing the preventive measure (30). Finally, messages that imply that the recipient is special based on the receipt of a scarce item (12) and that reinforce the perceptions of individual ownership and control over that item (14) can increase the perceived value and importance of the request, thus leading to more engagement and responsiveness.
Our findings are consistent with previous studies that demonstrate successful application of behavioral science principles to clinical care. The use of defaults has been effective in topics ranging from childhood obesity, opiate prescribing, HIV care, and organ donations (18,19,31–33). Message framing, or changing the focus of the salient costs and benefits, has shown success in skin cancer, mental health, and breast feeding (17,34–36). Despite the widespread success of these principles in other fields, positive studies in CRC screening are lacking. Defaults have previously been demonstrated to increase the uptake of FIT screening, but not colonoscopy (18–20,23). Other techniques, including active choice and message framing, failed to improve participation in both colonoscopy and FIT (21,22). Previous literature has proposed, however, that clear presentation of complex choices may be particularly important in CRC screening (16). Patients may be less likely to accept a default option of colonoscopy, a complex, invasive procedure involving multiple steps. On the other hand, defaulting to FIT screening, a relatively easy and risk-free test, may lead to an increase in participation. Although it is difficult to say which of the changes we implemented contributed most to the higher screening rate we observed in the intervention group, we hypothesize that the use of defaults, limited time windows, and alternative overload reduction had the largest impact because these changes focused on simplifying the choice of how and when to get screened.
There were several limitations to this intervention. First, it was performed in a single academic healthcare system, which limits the generalizability of our findings. Second, the development of the intervention required input from expert consultants in behavioral science, who might not be universally accessible. However, we feel that the principles applied in our letter construction address challenges that are ubiquitous in screening programs. Third, the response rate to the intervention was modest compared with usual care—a 24% relative increase in screening uptake and 4.6% absolute increase. Nonetheless, this response is higher than uptake with previous iterations of our mailed screening outreach and is consistent with response rates in other mailed outreach programs nationally (6,37,38). The study groups include individuals who are overdue for screening and likely represent a particularly challenging population to screen. Finally, because we incorporated several changes to the mailed letter at once, it is difficult for us to determine the specific changes that led to increased participation in screening.
Despite these challenges, our QI initiative has several strengths. First, it was a randomized intervention, performed on a diverse population of patients already overdue for screening. This patient population tends to be a more challenging group to engage and might benefit most from innovative strategies to encourage screening uptake. Second, it is a low-cost, feasible, and automated intervention that can be adapted and applied in various healthcare settings. Although mailed outreach has become more common in CRC screening programs, there has been little focus on how to best communicate with patients in mailings. Finally, our QI effort demonstrates that FIT participation rates might improve disproportionately with like efforts, which may benefit health systems with a high proportion of patients uninterested in colonoscopy or with limited access to colonoscopy.
In conclusion, our large randomized study in an academic institution demonstrated that small changes in how we communicate screening options with patients in mailed outreach programs have the potential to improve screening uptake. Thus, it may be beneficial to consider behavioral economics and social psychology techniques to optimize mailed outreach for CRC screening. Future QI efforts and studies should incorporate these and other low-cost strategies to increase participation in screening in diverse clinical settings.
CONFLICTS OF INTEREST
Guarantor of the article: Folasade P. May, MD, PhD.
Specific author contributions: O.M.: study concept and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, statistical analysis, critical revision of the manuscript for important intellectual content, and approval of the final version. N.A.-M.: study concept and design, drafting and modification of intervention letter, critical revision of the manuscript for important intellectual content, and approval of the final version. N.R.: study concept and design, critical revision of the manuscript for important intellectual content, and approval of the final version. A.D.: administrative, technical, and material support; critical revision of the manuscript for important intellectual content; and approval of the final version. N.J.G.: study concept and design, drafting and modification of intervention letter, critical revision of the manuscript for important intellectual content, and approval of the final version. S.B.S.: study concept and design, drafting and modification of intervention letter, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and approval of the final version. F.P.M.: study concept and design, analysis and interpretation of data, drafting of the manuscript, statistical analysis, study supervision, critical revision of the manuscript for important intellectual content, and approval of the final version.
Financial support: None to report.
Potential competing interests: None to report.
Study Highlights.
WHAT IS KNOWN
✓ CRC is a major cause of cancer-related morbidity and mortality.
✓ CRC screening is universally recommended; however, uptake is suboptimal.
✓ Behavioral economics and social psychology interventions have had positive impacts in clinical care but are under-explored for CRC screening.
WHAT IS NEW HERE
✓ Application of behavioral economics and social psychology principles to a mailed outreach CRC screening intervention improved screening uptake.
✓ The intervention was low-cost, automated, and feasible.
TRANSLATIONAL IMPACT
✓ Behavioral economics and social psychology techniques should be incorporated into mailed CRC screening outreach to improve screening uptake.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/A158, http://links.lww.com/CTG/A159
REFERENCES
- 1.Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010;116(3):544–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin 2014;64(2):104–17. [DOI] [PubMed] [Google Scholar]
- 3.Smith RA, Andrews K, Brooks D, et al. Cancer screening in the United States, 2016: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2016;66(2):96–114. [DOI] [PubMed] [Google Scholar]
- 4.US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for colorectal cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2016;315(23):2564–75. [DOI] [PubMed] [Google Scholar]
- 5.80% by 2018. National Colorectal Cancer Roundtable (http://nccrt.org/what-we-do/80-percent-by-2018/). Accessed February 4, 2019.
- 6.Yu C, Skootsky S, Grossman M, et al. A multi-level fit-based quality improvement initiative to improve colorectal cancer screening in a managed care population. Clin Transl Gastroenterol 2018;9(8):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. Revised & Expanded edn Penguin Books: New York, 2009. [Google Scholar]
- 8.Goldstein NJ, Martin SJ, Cialdini RB. Yes!: 50 Scientifically Proven Ways to Be Persuasive. Reprint edn Free Press: Ottawa, Canada, 2008. [Google Scholar]
- 9.Goldstein NJ, Cialdini RB, Griskevicius V. A room with a viewpoint: Using social norms to motivate environmental conservation in hotels. J Consum Res 2008;35(3):472–82. [Google Scholar]
- 10.Johnson EJ, Goldstein D. Medicine. Do defaults save lives? Science 2003;302(5649):1338–9. [DOI] [PubMed] [Google Scholar]
- 11.Levin IP, Gaeth GJ. How consumers are affected by the framing of attribute information before and after consuming the product. J Consumer Res 1988;15(3):374–8. [Google Scholar]
- 12.Cialdini RB. Influence: Science and Practice. 4th edn Allyn & Bacon: Boston, MA, 2000. [Google Scholar]
- 13.Kahneman D, Knetsch JL, Thaler RH. Experimental tests of the endowment effect and the coase theorem. J Polit Economy 1990;98(6):1325–48. [Google Scholar]
- 14.Peck J, Shu SB. Psychological Ownership and Consumer Behavior. Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar]
- 15.Loewenstein G, Asch DA, Volpp KG. Behavioral economics holds potential to deliver better results for patients, insurers, and employers. Health Aff (Millwood) 2013;32(7):1244–50. [DOI] [PubMed] [Google Scholar]
- 16.Purnell JQ, Thompson T, Kreuter MW, et al. Behavioral economics: “Nudging” underserved populations to be screened for cancer. Prev Chronic Dis 2015;12:E06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Detweiler JB, Bedell BT, Salovey P, et al. Message framing and sunscreen use: Gain-framed messages motivate beach-goers. Health Psychol 1999;18(2):189–96. [DOI] [PubMed] [Google Scholar]
- 18.Johnson EJ, Goldstein DG. Defaults and donation decisions. Transplantation 2004;78(12):1713–6. [DOI] [PubMed] [Google Scholar]
- 19.Zivin K, White JO, Chao S, et al. Implementing electronic health record default settings to reduce opioid overprescribing: A pilot study. Pain Med 2019;20(1):103–12. [DOI] [PubMed] [Google Scholar]
- 20.Mehta SJ, Khan T, Guerra C, et al. A randomized controlled trial of opt-in versus opt-out colorectal cancer screening outreach. Am J Gastroenterol 2018;113(12):1848–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta SJ, Feingold J, Vandertuyn M, et al. Active choice and financial incentives to increase rates of screening colonoscopy: A randomized controlled trial. Gastroenterology 2017;153(5):1227–9.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwartz PH, Perkins SM, Schmidt KK, et al. Providing quantitative information and a nudge to undergo stool testing in a colorectal cancer screening decision aid: A randomized clinical trial. Med Decis Making 2017;37(6):688–702. [DOI] [PubMed] [Google Scholar]
- 23.Narula T, Ramprasad C, Ruggs EN, et al. Increasing colonoscopies? A psychological perspective on opting in versus opting out. Health Psychol 2014;33(11):1426–9. [DOI] [PubMed] [Google Scholar]
- 24.Colorectal Cancer Screening. NCQA. (https://www.ncqa.org/hedis/measures/colorectal-cancer-screening/). Accessed February 4, 2019.
- 25.Madrian BC, Shea DF. The Power of Suggestion: Inertia in 401(k) Participation and Savings Behavior. National Bureau of Economic Research: 2000. 10.3386/w7682. [DOI] [Google Scholar]
- 26.Samuelson W, Zeckhauser R. Status quo bias in decision making. J Risk Uncertainty 1988;1(1):7–59. [Google Scholar]
- 27.Schwartz B, Kliban K. The Paradox of Choice: Why More Is Less. Unabridged edn Brilliance Audio: Grand Rapids, MI, 2014. [Google Scholar]
- 28.Ariely D, Wertenbroch K. Procrastination, deadlines, and performance: Self-control by precommitment. Psychol Sci 2002;13(3):219–24. [DOI] [PubMed] [Google Scholar]
- 29.Shu SB, Gneezy A. Procrastination of enjoyable experiences. J Marketing Res 2010;47(5):933–44. [Google Scholar]
- 30.Chapman GB. The psychology of medical decision making. In: Blackwell Handbook of Judgment and Decision Making. John Wiley & Sons, Ltd: 2008, pp 585–603. 10.1002/9780470752937.ch29. [DOI] [Google Scholar]
- 31.Loeb KL, Radnitz C, Keller KL, et al. The application of optimal defaults to improve elementary school lunch selections: Proof of concept. J Sch Health 2018;88(4):265–71. [DOI] [PubMed] [Google Scholar]
- 32.Montoy JCC, Dow WH, Kaplan BC. Cash incentives versus defaults for HIV testing: A randomized clinical trial. PLoS One 2018;13(7):e0199833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wagner Z, Montoy JCC, Drabo EF, et al. Incentives versus defaults: Cost-effectiveness of behavioral approaches for HIV screening. AIDS Behav 2019. 10.1007/s10461-019-02425-8. [DOI] [PubMed] [Google Scholar]
- 34.Lee MJ, Kang H. Designing skin cancer prevention messages: Should we emphasize gains or losses? Message framing, risk type, and prior experience. Am J Health Promot 2018;32(4):939–48. [DOI] [PubMed] [Google Scholar]
- 35.Mavandadi S, Wright E, Klaus J, et al. Message framing and engagement in specialty mental health care. Psychiatr Serv 2018;69(3):308–14. [DOI] [PubMed] [Google Scholar]
- 36.Merdasi F, Araban M, Saki MA. The effect of message-framing on breastfeeding self-efficacy among nulliparous women in Shushtar, Iran. Electron Physician 2017;9(1):3554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coronado GD, Petrik AF, Vollmer WM, et al. Effectiveness of a mailed colorectal cancer screening outreach program in community health clinics: The STOP CRC cluster randomized clinical trial. JAMA Intern Med 2018;178(9):1174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brenner AT, Rhode J, Yang JY, et al. Comparative effectiveness of mailed reminders with and without fecal immunochemical tests for Medicaid beneficiaries at a large county health department: A randomized controlled trial. Cancer 2018;124(16):3346–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.