Abstract
Background:
Recovery from dissociative identity disorder (DID) is associated with the process of integration, which includes an increasing sense of self-cohesion and ownership over one’s own emotions. Emotion perception is a construction based on interplay between stored knowledge (past experience), and incoming sensory inputs, suggesting changes in emotion perception might occur at different levels of integration – but this remains unexplored. Therefore, we examined the association between integration, psychiatric symptoms, and facial emotion perception. We hypothesized higher integration would be associated with fewer psychiatric symptoms, and differences in the perception of emotions.
Methods:
Participants were 82 respondents to a cross-sectional web-based study. All participants met self-report cutoff scores for posttraumatic stress disorder (PTSD) and DID using the PTSD Checklist for DSM-5 and Multiscale Dissociation Inventory, respectively. Participants completed a psychometrically-matched test of facial emotion perception for anger, fear, and happiness called the Belmont Emotion Sensitivity Test. Participants also completed the Beck Depression Inventory II, Childhood Trauma Questionnaire, and Integration Measure, a validated measure of self-cohesion.
Results:
Higher integration scores were associated with lower depression, PTSD, and autobiographical memory disturbance scores. Repeated-measures ANCOVA confirmed integration significantly interacted with emotion category on the facial emotion perception task. Specifically, higher integration scores were associated with greater accuracy to fearful and angry faces.
Conclusions:
While acknowledging the limitations of a cross-sectional design, our results suggest that the process of integration is associated with fewer psychiatric symptoms, and more accurate facial emotion perception. This supports treatment guidelines regarding integration as a therapeutic goal for DID.
Keywords: dissociation, dissociative identity disorder, web-based, emotion perception, PTSD/Posttraumatic Stress Disorder, trauma
Introduction
Recovery from dissociative identity disorder
Dissociative identity disorder (DID) is a posttraumatic coping response associated with chronic childhood trauma (Dalenberg et al., 2012; Putnam, 1997). Contrary to popular opinion, DID is relatively common, with an estimated 1 to 3% lifetime prevalence rate in the population (Dorahy et al., 2014), and upwards of 14% prevalence in psychiatric emergency departments (Sar et al., 2007). It is associated with both significant personal and societal burden. For example, individuals with dissociative disorders experience high levels of self-harm and suicidality (Foote, Smolin, Neft, & Lipschitz, 2008). Approximately three-quarters of individuals with DID report a history of at least one suicide attempt (Putnam, Guroff, Silberman, Barban, & Post, 1986). A Canadian healthcare study estimated a $75,000 cost to treat one person with DID for one year if they had not yet been properly diagnosed (Ross & Dua, 1993). Costs drop considerably as individuals receive specialized treatment (Myrick, Webermann, Langeland, Putnam, & Brand, 2017). However, on average someone with DID takes seven years to be diagnosed correctly (Putnam et al., 1986; Ross & Dua, 1993), and subsequently access this specialized treatment. Despite high prevalence rates and substantial burden, DID and DID recovery have remained understudied.
In addition to other posttraumatic symptoms, individuals with DID experience profound identity alteration in which their own thoughts, emotions, feelings, memories, bodily experience, and behaviors can feel non-autobiographical (Dell, 2006; Dell & Lawson, 2009). This occurs because childhood trauma has disrupted the typical developmental process of building a cohesive sense of self (Putnam, 1997). During traumatic episodes, experiencing some thoughts, feelings, and behaviors as not happening to oneself serves a protective role by limiting the psychological and biological impact of the traumatic events (van der Hart, Nijenhuis, & Steele, 2006; Weniger et al., 2013). This subjective experience suggests there has been an interruption in autobiographical memory formation. Because these same autobiographical memory systems are vital during development for building a cohesive sense of self, this acutely protective response may lead to long-term autobiographical memory dysfunction (Huntjens et al., 2014). Despite these consequences, this distancing effect from traumatic experiences and disruption in one’s sense of self may also help preserve attachment bonds to abusive caretakers (Freyd, 1996).
In contrast, recovery from DID is associated with the process of integration. The process of integration includes the development of a sense of self-ownership over one’s mental and bodily experience (i.e., “personification,” van der Hart et al., 2006). Past research has linked increased integration in DID samples to decreased amnesia, dissociative, somatoform, depressive, and posttraumatic stress disorder (PTSD) symptoms (Coons & Bowman, 2001; Ellason & Ross, 1997; Kluft, 1984). Behavioral tests also suggest integration is associated with a restoration of self-referential processing to one’s own face for individuals with DID (Lebois et al., 2019). These findings suggest that at the core of feeling integrated are properly functioning autobiographical memory systems, and that increasing levels of integration, at least in part, may reflect the restoration of properly-functioning autobiographical memory systems. Despite this foundational work, the relationship between integration and the perception of other peoples’ faces, in particular facial emotion perception, is unknown. Facial emotion perception is intricately tied to social perception and functioning (e.g., Chanes, Wormwood, Betz, & Barrett, 2018) – suggesting this might be a key behavioral marker of improved social functioning and recovery from DID.
Emotion perception as a construction
There is reason to hypothesize that emotion perception may be impacted by the process of integration in DID. Namely, our emotion concepts are constructed over time based on stored memories of our prior experience (e.g., sensorimotor and interoceptive experience; Barrett & Simmons, 2015). These stored experiences are used to make predictions about incoming sensory input (Barrett & Simmons, 2015; Clark, 2013). In this way, our current (emotional) experience is a construction based on interplay between both stored knowledge (past experiences), and incoming sensory inputs (Barrett, 2017). Perception of another person’s emotion is this same process unfolding dynamically between two people (Gendron & Barrett, 2018). Therefore, our perception of another person’s emotion is shaped by our own prior experiences of that emotion. For individuals with DID, childhood maltreatment (da Silva Ferreira, Crippa, & de Lima Osorio, 2014), and a felt lack of ownership over feelings and emotions may impact their emotion concepts, and therefore their perception of other people’s emotions. Likewise, recovery from DID associated with increased integration might be accompanied by changes in emotion perception. To date, these associations remain unexplored. Greater understanding of the changes associated with integration would facilitate evaluation of treatment progress and point toward optimal or novel treatment strategies.
Experiment overview
To conduct a conceptual replication of symptom reductions associated with integration, and to also conduct a novel test of the relationship between integration and emotion perception, we recruited individuals with co-occurring PTSD and DID to participate in a web-based study. Participants completed a battery of self-report symptom measures, including the Integration Measure, and a test of emotion perception called the Belmont Emotion Sensitivity Test, which measures sensitivity to facial expressions of happiness, anger, and fear (Rutter et al., 2019). We hypothesized higher integration would be associated with lower depression, PTSD, and dissociative symptoms. We also predicted participants’ integration level would interact with emotion category on the Belmont Emotion Sensitivity Test.
Materials and Methods
Participants
Participants were 125 respondents to a cross-sectional web-based study. Participants were excluded for not being fluent in English (N=3), and not passing validity checks outlined below (N=16). Of the remaining participants (N=106), 82 met criteria for both provisional PTSD and DID diagnoses based on the PTSD Checklist for DSM-5 and the Multiscale Dissociation Inventory, respectively. The demographics and clinical characteristics of these 82 participants are outlined in Table 1 and 2. The results that follow are from only these 82 participants. All procedures, including consent were approved by the Partners Hospital Institutional Review Board, and in accordance with the ethical standards of the Declaration of Helsinki as revised 1989. Participants were not compensated for participation.
Table 1.
Participant Demographics
| Provisional Diagnosis, N (%) | |
| PTSD | 82 (100%) |
| DID | 82 (100%) |
| Age, mean ± SD | 40.14 ± 12.87 |
| Sex assigned at birth, N (%) | |
| Female | 80 (97.6%) |
| Missing | 2 (2.4%) |
| Gender, N (%) | |
| Male | 2 (2.4%) |
| Female | 57 (69.5%) |
| Transgender | 2 (2.4%) |
| Self-Identified | 1 (1.2%) |
| Nonbinary / Fluid / Queer / Gender Queer | 19 (23.2%) |
| Missing | 1 (1.2%) |
| Race, N (%) | |
| Asian | 1 (1.2%) |
| Black / African-American | 2 (2.4%) |
| Middle Eastern / North African (Non-White) | 1 (1.2%) |
| Multiracial | 6 (7.3%) |
| Native American / American Indian / Alaska Native / Indigenous | 1 (1.2%) |
| Other | 4 (4.9%) |
| Prefer not to answer | 3 (3.7%) |
| White | 61 (74.4%) |
| Missing | 3 (3.7%) |
| Ethnicity, N (%) | |
| Hispanic / Latinx | 6 (7.3%) |
| Non-Hispanic / Non-Latinx | 57 (69.5%) |
| Not Listed | 3 (3.7%) |
| Prefer not to answer | 3 (3.7%) |
| Unknown | 4 (4.9%) |
| Missing | 9 (11%) |
| Education, N (%) | |
| Grade 7 to 12 (without graduating high school) | 1 (1.2%) |
| Graduated high school or equivalent | 10 (12.2%) |
| Part of College | 26 (31.7%) |
| Graduated 2 Year College | 8 (9.8%) |
| Graduated 4 Year College | 12 (14.6%) |
| Part of Graduate/Professional School | 3 (3.7%) |
| Completed Graduate / Professional School | 22 (26.8%) |
Note. N = 82
Table 2.
Participant Characteristics
| Childhood Trauma Questionnaire (CTQ), mean ± SD | 85.73 ± 17.32 |
| Emotional Abuse | 19.63 ± 4.78 |
| Physical Abuse | 12.50 ± 5.27 |
| Sexual Abuse | 20.49 ± 5.13 |
| Emotional Neglect | 19.87 ± 3.86 |
| Physical Neglect | 13.49 ± 4.64 |
| PTSD Checklist for DSM-5 (PCL-5), mean ± SD | 55.11 ± 11.00 |
| Multiscale Dissociation Inventory (MDI), mean ± SD | 108.39 ± 20.67 |
| Disengagement | 20.15 ± 3.80 |
| Depersonalization | 16.71 ± 4.91 |
| Derealization | 16.87 ± 4.45 |
| Emotional Constriction | 16.49 ± 5.15 |
| Memory Disturbance | 16.33 ± 4.93 |
| Identity Dissociation | 21.85 ± 2.89 |
| Integration Measure (IM), mean ± SD | 10.70 ± 3.85 |
| Modified Beck Depression Inventory II, mean ± SD | 33.18 ± 10.73 |
Note. N = 82
Measures
The Belmont Emotion Sensitivity Test.
Participants completed a test of facial emotion perception called the Belmont Emotion Sensitivity Test (for further details, see Rutter et al., 2019). This test has three separate psychometrically-matched subtests for anger, fear, and happiness perception in which all the trials for each emotion are completed at one time. This test is specifically designed to eliminate response bias and reliability issues in standard emotion perception paradigms and is matched for difficulty across each emotion subtest.
As described further in Rutter et al (2019), the facial stimuli used in the task were the angry, fearful, and happy expressions of five face identities drawn from the Karolinska Directed Emotional Faces database (Lundqvist, Flykt, & Ohman, 1998). The faces were then morphed to include a mix of two emotions. For example, the fearful faces were morphed on a continuum to include angry faces and on a continuum to include happy faces.
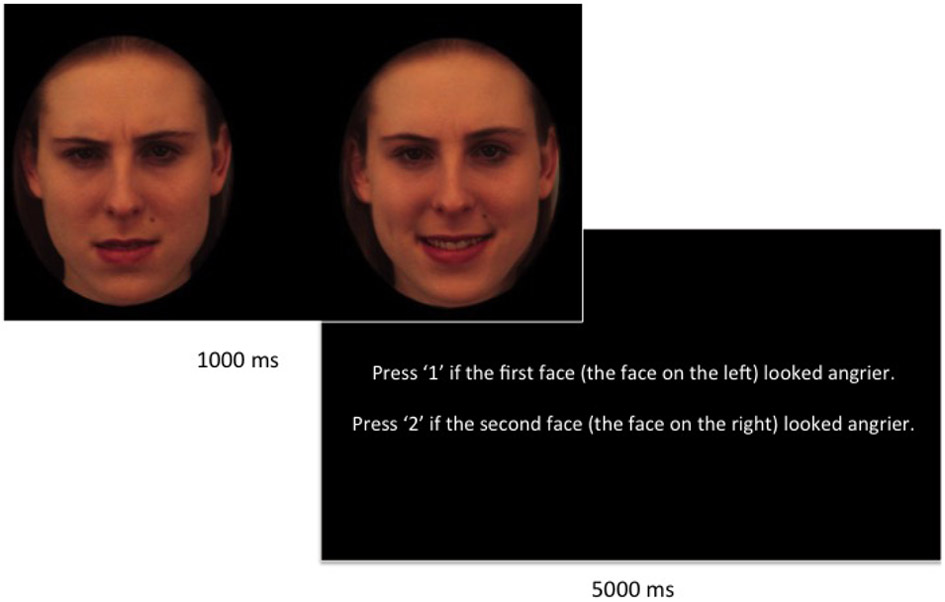
As illustrated in Figure 1, during each subtest, participants were shown two morphed faces at the same time, presented side-by-side, for 1000 ms. Their task was to judge which of the two faces was angrier during the anger test, which was more afraid during the fear test, and which was happier during the happiness test.
Figure 1.
An example easy anger trial on the Belmont Emotion Sensitivity Test. ms = milliseconds.
After the face screen disappeared, the response screen displayed the text, “Press ‘1’ if the first face (the face on the left) looked angrier. Press ‘2’ if the second face (the face on the right) looked angrier.” “Angrier” was replaced with “more afraid” and “happier” for the fear and happy tests, respectively. Participants had 5000 ms to indicate their response before the trial timed-out. If the participant did not make a response, the trial repeated itself until they made a response.
The trials varied in difficulty within each emotion subtest by changing the degree of difference between the two displayed morphed faces. For example, for an easy anger trial, one face would contain 70% more of an angry expression compared to the other face. In contrast, during a hard anger trial, one face would contain only 20% more of an angry expression compared to the other face. The first 8 trials in each subtest were easy, the next 20 were of medium difficulty, and the final 28 trials were hard. In total, each participant completed two practice trials, and 56 test trials for each emotion subtest. The order of emotion subtests was randomized for each participant.
Childhood trauma questionnaire (CTQ).
The CTQ is a 28-tem self-report retrospective measure of childhood maltreatment severity (Bernstein et al., 1994). The CTQ asks participants to indicate how often experiences occurred when they were growing up on a 5-point Likert scale ranging from “never true” to “very often true”. The CTQ has five subscales measuring emotional, physical, and sexual abuse, and physical and emotional neglect. The CTQ has good reliability and validity in a variety of clinical and nonclinical samples (e.g., Bernstein et al., 1994). Subscale scores range from 5 to 25, and total scores range from 25 to 125. Higher scores indicate greater childhood trauma severity.
PTSD Checklist for DSM-5 (PCL-5).
The PCL-5 is a 20-item self-report measure of PTSD symptom severity for the past month (Blevins, Weathers, Davis, Witte, & Domino, 2015). The PCL-5 asks participants to indicate, “How much you were bothered by” various PTSD symptoms on a 5-point Likert scale ranging from “not at all” to “extremely.” The PCL-5 has good reliability and validity (Blevins et al., 2015). The total score ranges from 0-80, and scores above 32 were used as a cut-point for a provisional diagnosis of PTSD in our sample (Bovin et al., 2016).
Multiscale Dissociation Inventory (MDI).
The MDI is a 30-item self-report measure of past month dissociative symptom severity (Briere, 2002). The MDI asks participants to indicate “how often” various dissociative symptoms occurred on a 5-point Likert scale ranging from “never” to “very often.” The MDI measures six types of dissociation: disengagement, depersonalization, derealization, emotional constriction/numbing, memory disturbance, and identity dissociation. It has good reliability and validity in clinical and community samples (Briere, 2002; Briere, Weathers, & Runtz, 2005). An Identity Dissociation score greater than 14 has been found to identify 93% of those with a DID diagnosis and 92% of those without DID (Briere, 2002). Therefore, this score was used as a cut-point in our sample for a provisional DID diagnosis.
Integration Measure (IM).
The IM is an 18-item self-report questionnaire designed specifically for individuals with DID to measure the degree of cohesion vs. fragmentation in their sense of self (Barlow & Chu, 2014). Five multiple choice items make up the integration subscale. These five questions ask about the degree of communication, awareness, and cooperation among the individual’s identity states on a 5-point Likert scale ranging from “never, or with none of the parts” to “always, or with all of the parts.” In our sample, the integration subscale had good internal consistency (α=.82). Integration subscale scores range from 0 to 20. Higher scores indicate greater levels of integration.
Modified Beck Depression Inventory II (BDI-II).
The BDI-II is a 21-item self-report measure of past month depression symptoms (Beck, Steer, & Brown, 1996). It asks participants to rate “your worst feelings of depression” on a 4-point Likert scale. It has good reliability and validity across samples (Wang & Gorenstein, 2013). Given our data collection was not monitored in real-time, we removed the item asking about suicidal thoughts or wishes. Thus, our modified BDI-II was a 20-item measure. Higher scores indicate greater depression severity.
Validity checks.
Participants also completed two validity check items. Specifically, “Was this your first time completing this task?” and “Did you have any technical or other problems that may have influenced your results?” These items were used to exclude participants if they completed the task multiple times or if they reported technical or other difficulties.
Procedure
Participants were recruited through advertisements placed on the listserv and Facebook page of an Infinite Mind, an organization for individuals with DID. All procedures were web-based. Participants read a study information sheet, and provided implied consent by clicking the “agree to participate” button. After consent, participants completed a battery of cognitive tasks in a randomized order, including the Belmont Emotion Sensitivity Test. After the tasks, participants completed a series of self-report measures, including a demographic questionnaire, measures of childhood trauma (CTQ), PTSD symptoms (PCL-5), dissociative symptoms (MDI), integration (IM), depression symptoms (modified BDI-II), and validity checks. In case participants were distressed after the experiment, the closing text offered web-links to international crisis hotlines and resources for adult survivors of childhood abuse.
Data Analysis
Accuracy was calculated separately for each Belmont Emotion Sensitivity Test emotion (fear, anger, happy) using MATLAB version 2018a. All practice and timed-out trials were removed. For each emotion subtest, three accuracy scores were calculated for each participant, namely, one for easy, medium, and hard trials. We calculated each score by adding the total number correct in that category and dividing it by the total number of trials for that category (e.g., 8 for easy vs. 20 for medium). All self-report scores were calculated as recommended by published scoring guidelines. In addition, integration scores were transformed into standardized z-scores.
To test the interaction between standardized integration scores and emotion category on the Belmont Emotion Sensitivity Test, we completed a series of repeated measure analyses of covariance (ANCOVA) on accuracy scores. For significant interactions, we then computed pairwise comparisons of the estimated marginal means to test for differences between anger, fear, and happy emotion subtests while holding integration scores constant at one standard deviation below (“lower integration”), one standard deviation above the mean (“higher integration +1SD”), and two standard deviations above the mean (“higher integration +2SD”). Reported p-values for the pairwise comparisons are Sidak-corrected and 2-tailed. All calculations were completed using SPSS version 24.
Results
Integration and Psychiatric Symptoms
Correlation analyses revealed higher integration scores were associated with lower depression severity on the modified BDI-II, r(80) = −.34, p = .002, lower overall PTSD symptom severity on the PCL-5, r(80) = −.23, p = .014, and lower autobiographical memory disturbance severity on the MDI, r(80) = −.27, p = .015. No associations were found between integration and childhood trauma severity or the other MDI dissociation subscales(p’s >.05).
Belmont Emotion Sensitivity Test Accuracy
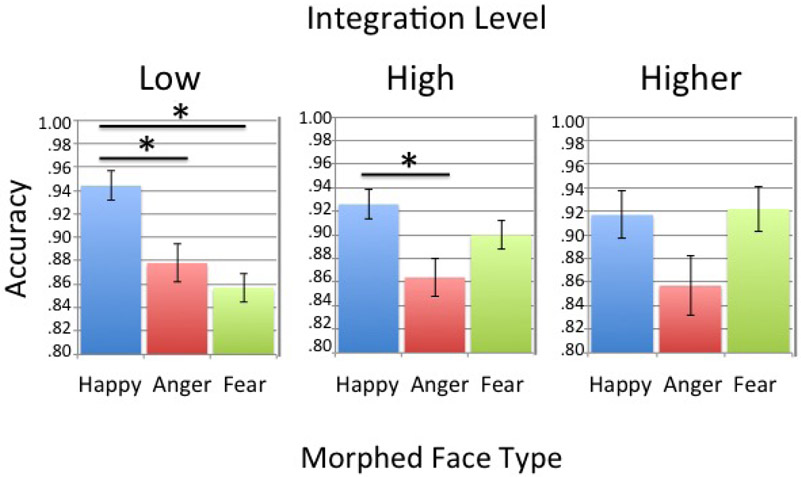
We hypothesized there would be a significant interaction between integration and emotion category on the Belmont Emotion Sensitivity Test. As illustrated in Figure 2, our hypothesis was confirmed for trials of medium difficulty, F(1.89, 151.15) = 3.59, p = .032. Pairwise comparisons indicated individuals with lower integration scores (−1SD) performed significantly worse on both anger, M difference = .07, t(81) = 3.5, SE = .02, p = .001, and fear trials, M difference = .09, t(81) = 4.5 , SE = .02, p < .001, compared to happy trials. However, individuals with higher integration scores (+1SD) performed significantly worse only on angry trials compared to happy trials, M difference = .06, t(81) = 3.00, SE = .02, p = .001. Individuals with even higher integration scores (+2SD) performed similarly on all emotion tests (p’s >.05). Conversely, there was no integration by emotion category interaction on easy, F(1.44, 115.14) = 2.27, p = .123, or hard trials, F(1.88, 150.22) = 2.38, p = .100.
Figure 2.
The estimated marginal means for accuracy on trials of medium difficulty in the Belmont Emotion Sensitivity Test. The left panel represents one standard deviation below the mean on standardized integration scores. The middle panel represents one standard deviation above the mean on standardized integration scores. The right panel represents two standard deviations above the mean on standardized integration scores. Error bars represent +/− 1 standard error of the mean. *indicates p < .05
Discussion
Recovery from DID is associated with integration, a process that includes a felt sense of self-ownership over one’s thoughts, emotions, and bodily experiences (van der Hart, Nijenhuis, & Steele, 2006). A small body of foundational work suggests integration is associated with improvement in dissociative, PTSD, and depressive symptoms (Coons & Bowman, 2001; Ellason & Ross, 1997; Kluft, 1984), and increased self-referential processing to one’s own face (Lebois et al., 2019). However, small sample sizes and inadequate objective markers of integration limit this work. Greater understanding of the changes associated with integration would facilitate consistent, nuanced measurement of integration across studies, and it would enable treatment progress evaluation within and across individuals with DID. Therefore, we tested the relationship between integration and 1) other common trauma-related symptoms, and 2) facial emotion perception in a large sample of individuals with co-occurring PTSD and DID. Our hypothesis that higher integration would be associated with fewer psychiatric symptoms and differences in emotion perception was confirmed.
Integration is associated with fewer psychiatric symptoms
We found that higher integration was associated with lower depression, PTSD, and dissociative memory disturbances. Of note, the memory disturbances measured by the MDI are autobiographical. This suggests the process of integration, least in part, likely reflects restoration in proper functioning of one’s autobiographical memory systems. Similar to previous work (Barlow & Chu, 2014), we also found integration was not related to childhood trauma severity. Our findings indicated the relationships between integration and depression, PTSD, and memory disturbances had small to medium effect sizes. These associations may have been impacted by the fact that everyone in our sample still met criteria for a provisional diagnosis of both PTSD and DID. This suggests larger effect sizes may be present in samples including individuals who have fully recovered from DID. Likewise, we may also have seen associations with other dissociation subscales (e.g., disengagement, depersonalization, derealization, emotional constriction, identity dissociation) if we included individuals who had fully recovered. Our findings replicate previous work associated with integration, but now using a standardized self-report measure of integration and a larger sample. Furthermore, our work measured integration as a continuous variable instead of a dichotomous integrated vs. not. This allowed us to capture gradation in the experience of self-ownership over mental experience, which may be more informative for clinical practice.
Integration is associated with differences in emotion perception
We found that integration scores were associated with differences in accuracy on a measure of facial emotion perception to angry, fearful, and happy faces. In particular, higher integration scores were associated with better performance to fearful faces compared to individuals with lower integration scores. Prior work demonstrates individuals with DID have reduced habituation of the startle reflex, a marker of hypervigilance and altered fear responding (Dale, Flaten, Elden, & Holte, 2008). Our results suggest these differences in fear responding may resolve as individuals with DID become more integrated.
Angry face performance was not statistically different from fear and happy face performance in individuals with higher integration, but only in individuals two standard deviations above the mean in integration scores (not at one standard deviation). Previous work demonstrates childhood maltreatment is associated with differential behavioral and brain responses to angry faces (da Silva Ferreira et al., 2014). For individuals with histories of severe interpersonal childhood trauma, the concept of anger in particular may be strongly associated with their perpetrator(s) (Steele, Boon, & van der Hart, 2016). That is, the perpetrator’s anger may have often preceded or followed abuse, and the individual may be reluctant to express or experience anger themselves because they worry it may make them like their abuser. For this reason, feeling a sense of ownership over one’s own experience of anger may be especially difficult and may require even higher levels of integration, as suggested by our findings.
Error management theory may provide further explanation for the weaker anger findings and development of different emotion concepts for individuals who have experienced childhood trauma. This theory posits that humans develop biases in their decision-making that are adaptive for survival even if these biases produce more overall errors (Haselton & Buss, 2000; Haselton & Nettle, 2006). For example, in abusive families, it may be difficult to predict when the abuse will occur because caregivers may hide their anger until the last moment or other facial expressions may precede abuse. Children in these contexts may be biased to perceive even a hint of anger in facial expressions as an adaptive survival mechanism. That is, it would be better to have a “false positive” in anger detection than to have a “false negative” and miss the opportunity to flee, fight, or freeze. However, this bias may then interfere with detecting subtle differences in the magnitude of angry faces in our paradigm, even at higher levels of integration.
More generally, our work suggests a greater sense of self-ownership over emotions and feelings is associated with differences in an individual’s emotion concepts. Their emotion concepts, and in turn, their emotion perception is impacted by this new learning. This corresponds with previous evidence that learning plays a central role in emotion (Lebois, Wilson-Mendenhall, Simmons, Barrett, & Barsalou, 2018).
Limitations
We acknowledge several limitations of this work that constrain our conclusions. First, we implemented a cross-sectional design. Thus, we have measured associations with different levels of integration, but cannot conclude definitively that these same differences would manifest within an individual. However, our findings resonate with existing longitudinal work. Future work should seek to replicate these findings in a longitudinal design.
Second, we employed a web-based design in which individuals participated anonymously outside the laboratory. This may have impacted our findings, however, research suggests cognitive web-based samples can be as reliable as traditional lab-based samples (Germine et al., 2012; Hartshorne & Germine, 2015; Meyerson & Tryon, 2003). Additionally, this design may have facilitated broader, more diverse participation given the dearth of DID research opportunities and high levels of stigma associated with DID. In addition, because measures were web-based, diagnoses for PTSD and DID were provisional based on established self-report cutoff scores. Given this, the risk of both false positives and false negatives in diagnoses is possible. Future research should seek to replicate these findings in lab-based studies with gold-standard diagnostic interviews. Furthermore, we did not ask participants to be in a particular identity state when completing the emotion perception tasks. It is plausible that identity state could modulate responses on these tasks. Future work may wish to test this hypothesis.
Conclusions and Clinical Implications
This was the first study of its kind to measure the impact of integration on facial emotion perception in co-occurring PTSD and DID. We have contributed to theoretical accounts of emotion in that our results suggest learning underlies emotion. That is, emotional conceptualizations entrenched in memory from repeated abuse and neglect may be changed by learning more adaptive conceptualizations over time (e.g., in psychotherapy). We have also identified a potential objective behavioral marker of changes associated with recovery from DID, namely, greater accuracy on tests of facial emotion perception. Emotion perception is linked to social functioning (Chanes et al., 2018). Consequently, this work supports expert-consensus guidelines that integration is a therapeutic goal of treatment for DID (International Society for the Study of Trauma and Dissociation, 2011).
Highlights.
Higher integration was associated with lower depression, PTSD, and amnesia
Higher integration was associated with more accurate facial emotion perception
Empirical support for dissociative identity disorder expert treatment guidelines
Acknowledgments:
The authors would like to thank our study participants, Jaime Pollack and an Infinite Mind for recruitment facilitation, and Kerry Ressler for feedback.
Funding Sources: The work was supported by National Institute of Mental Health (NIMH) grant K01MH118457 to LAML, and the McLean Hospital Trauma Scholars and Trauma Initiative Funds to MLK.
Role of Funding Source: Funding sources had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data Sharing: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflict of Interest
The authors declared no conflicts of interest with respect to the authorship or the publication of this article. Dr. Lauren Lebois reports grants from the National Institute of Mental Health during the conduct of the study. Dr. Kaufman reports support from the Trauma Initiative Fund and the Trauma Scholars Fund at McLean Hospital during the conduct of the study.
References
- Barlow MR, & Chu JA (2014). Measuring fragmentation in dissociative identity disorder: the integration measure and relationship to switching and time in therapy. European Journal of Psychotraumatology, 5, 1–8. 10.3402/ejpt.v5.22250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett LF (2017). The theory of constructed emotion: an active inference account of interoception and categorization. Social Cognitive and Affective Neuroscience, 12(11), 1833–1856. 10.1093/scan/nsx060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett LF, & Simmons WK (2015). Interoceptive predictions in the brain. Nature Reviews. Neuroscience, 16(7), 419–429. 10.1038/nrn3950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, … Ruggiero J (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry, 151(8), 1132–1136. 10.1176/ajp.151.8.1132 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders--fifth edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379. [DOI] [PubMed] [Google Scholar]
- Briere J (2002). MDI, Multiscale Dissociation Inventory: Professional Manual. [Google Scholar]
- Briere J, Weathers FW, & Runtz M (2005). Is dissociation a multidimensional construct? Data from the Multiscale Dissociation Inventory. Journal of Traumatic Stress, 18(3), 221–231. 10.1002/jts.20024 [DOI] [PubMed] [Google Scholar]
- Chanes L, Wormwood JB, Betz N, & Barrett LF (2018). Facial expression predictions as drivers of social perception. Journal of Personality and Social Psychology, 114(3), 380–396. 10.1037/pspa0000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A (2013). Whatever next? Predictive brains, situated agents, and the future of cognitive science. The Behavioral and Brain Sciences, 36(3), 181–204. 10.1017/S0140525X12000477 [DOI] [PubMed] [Google Scholar]
- Coons PM, & Bowman EAS (2001). Ten-Year Follow-Up Study of Patients with Dissociative Identity Disorder. Journal of Trauma & Dissociation: The Official Journal of the International Society for the Study of Dissociation , 2(1), 73–89. 10.1300/J229v02n01_09 [DOI] [Google Scholar]
- Dale KY, Flaten MA, Elden A, & Holte A (2008). Dissociative identity disorder and prepulse inhibition of the acoustic startle reflex. Neuropsychiatric Disease and Treatment, 4(3), 653–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalenberg CJ, Brand BL, Gleaves DH, Dorahy MJ, Loewenstein RJ, Cardena E, … Spiegel D (2012). Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychological Bulletin, 138(3), 550–588. 10.1037/a0027447 [DOI] [PubMed] [Google Scholar]
- da Silva Ferreira GC, Crippa JAS, & de Lima Osório F (2014). Facial emotion processing and recognition among maltreated children: a systematic literature review. Frontiers in Psychology, 5, 1460 10.3389/fpsyg.2014.01460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell PF (2006). A new model of dissociative identity disorder. The Psychiatric Clinics of North America, 29(1), 1–26, vii. https://doi.org/10.1016Zj.psc.2005.10.013 [DOI] [PubMed] [Google Scholar]
- Dell P, & Lawson D (2009). Empirically delineating the domain of pathological dissociation In Dell PF& O’Neil JA (Ed.), Dissociation and the dissociative disorders: DSM-Vand beyond (pp. 667–692). Routledge. [Google Scholar]
- Dorahy MJ, Brand BL, Sar V, Krüger C, Stavropoulos P, Martinez-Taboas A, … Middleton W (2014). Dissociative identity disorder: An empirical overview. The Australian and New Zealand Journal of Psychiatry, 48(5), 402–417. 10.1177/0004867414527523 [DOI] [PubMed] [Google Scholar]
- Ellason JW, & Ross CA (1997). Two-year follow-up of inpatients with dissociative identity disorder. The American Journal of Psychiatry, 154(6), 832–839. 10.1176/ajp.154.6.832 [DOI] [PubMed] [Google Scholar]
- Foote B, Smolin Y, Neft DI, & Lipschitz D (2008). Dissociative disorders and suicidality in psychiatric outpatients. The Journal of Nervous and Mental Disease, 196(1), 29–36. 10.1097/NMD.0b013e31815fa4e7 [DOI] [PubMed] [Google Scholar]
- Freyd JJ (1996). Betrayal Trauma: The Logic of Forgetting Childhood Abuse. [Google Scholar]
- Gendron M, & Barrett LF (2018). Emotion Perception as Conceptual Synchrony. Emotion Review: Journal of the International Society for Research on Emotion, 10(2), 101–110. 10.1177/1754073917705717 [DOI] [Google Scholar]
- Germine L, Nakayama K, Duchaine BC, Chabris CF, Chatterjee G, & Wilmer JB (2012). Is the Web as good as the lab? Comparable performance from Web and lab in cognitive/perceptual experiments. Psychonomic Bulletin & Review, 19(5), 847–857. 10.3758/s13423-012-0296-9 [DOI] [PubMed] [Google Scholar]
- Hartshorne JK, & Germine LT (2015). When Does Cognitive Functioning Peak? The Asynchronous Rise and Fall of Different Cognitive Abilities Across the Life Span. Psychological Science, Vol. 26, pp. 433–443. 10.1177/0956797614567339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haselton MG, & Buss DM (2000). Error management theory: A new perspective on biases in cross-sex mind reading. Journal of personality and social psychology, 78(1,81–91. 10.1037/0022-3514.78.1.81 [DOI] [PubMed] [Google Scholar]
- Haselton MG, & Nettle D (2006). The paranoid optimist: An integrative evolutionary model of cognitive biases. Personality and social psychology review, 10(1), 47–66. 10.1207/s15327957pspr1001_3 [DOI] [PubMed] [Google Scholar]
- Huntjens RJC, Wessel I, Hermans D, & van Minnen A (2014). Autobiographical memory specificity in dissociative identity disorder. Journal of Abnormal Psychology, 123(2), 419–428. 10.1037/a0036624 [DOI] [PubMed] [Google Scholar]
- International Society for the Study of Trauma and Dissociation. (2011). Guidelines for treating dissociative identity disorder in adults, third revision. Journal of Trauma & Dissociation: The Official Journal of the International Society for the Study of Dissociation , 12(2), 115–187. 10.1080/15299732.2011.537247 [DOI] [PubMed] [Google Scholar]
- Kluft RP (1984). Treatment of multiple personality disorder. A study of 33 cases. The Psychiatric Clinics of North America, 7(1), 9–29. [PubMed] [Google Scholar]
- Lebois LAM, Wilson-Mendenhall CD, Simmons WK, Barrett LF, & Barsalou LW (2018). Learning situated emotions. Neuropsychologia. 10.1016/j.neuropsychologia.2018.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebois LAM, Wolff JD, Hill SB, Bigony CE, Winternitz S, Ressler KJ, & Kaufman ML (2019). Preliminary Evidence of a Missing Self Bias in Face Perception for Individuals with Dissociative Identity Disorder. Journal of Trauma & Dissociation: The Official Journal of the International Society for the Study of Dissociation , 20(2), 140–164. 10.1080/15299732.2018.1547807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundqvist D, Flykt A, & Ohman A (1998). KDEF. Stockholm: Karolinska Hospital. [Google Scholar]
- Meyerson P, & Tryon WW (2003). Validating internet research: a test of the psychometric equivalence of internet and in-person samples. Behavior Research Methods, Instruments, & Computers: A Journal of the Psychonomic Society, Inc, 35(4), 614–620. Retrieved from http.www.ncbi.nlm.nih.gov/pubmed/14748506 [DOI] [PubMed] [Google Scholar]
- Myrick AC, Webermann AR, Langeland W, Putnam FW, & Brand BL (2017). Treatment of dissociative disorders and reported changes in inpatient and outpatient cost estimates. European Journal of Psychotraumatology, 5(1), 1375829 10.1080/20008198.2017.1375829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam FW (1997). Dissociation in Children and Adolescents: A Developmental Perspective. [PubMed] [Google Scholar]
- Putnam FW, Guroff JJ, Silberman EK, Barban L, & Post RM (1986). The clinical phenomenology of multiple personality disorder: review of 100 recent cases. The Journal of Clinical Psychiatry, 47(6), 285–293. Retrieved from http.www.ncbi.nlm.nih.gov/pubmed/3711025 [PubMed] [Google Scholar]
- Ross CA, & Dua V (1993). Psychiatric health care costs of multiple personality disorder. American Journal of Psychotherapy, 47(1), 103–112. 10.1176/appi.psychotherapy.1993.47.1.103 [DOI] [PubMed] [Google Scholar]
- Rutter LA, Dodell-Feder D, Vahia IV, Forester BP, Ressler KJ, Wilmer JB, & Germine L (2019). Emotion sensitivity across the lifespan: Mapping clinical risk periods to sensitivity to facial emotion intensity. Journal of Experimental Psychology. General. 10.1037/xge0000559 [DOI] [PubMed] [Google Scholar]
- Sar V, Koyuncu A, Ozturk E, Yargic LI, Kundakci T, Yazici A, … Aksut D (2007). Dissociative disorders in the psychiatric emergency ward. General Hospital Psychiatry, 29(1), 45–50. 10.1016/j.genhosppsych.2006.10.009 [DOI] [PubMed] [Google Scholar]
- Steele K, Boon S, & van der Hart O (2016). Treating Trauma-Related Dissociation: A Practical, Integrative Approach (Norton Series on Interpersonal Neurobiology). [Google Scholar]
- van der Hart O, Nijenhuis ERS, & Steele K (2006). The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization. [Google Scholar]
- Wang Y-P, & Gorenstein C (2013). Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Revista Brasileira de Psiquiatria (Sao Paulo, Brazil : 1999), 35(4), 416–431. 10.1590/1516-4446-2012-1048 [DOI] [PubMed] [Google Scholar]
- Weniger G, Siemerkus J, Barke A, Lange C, Ruhleder M, Sachsse U, … Irle E (2013). Egocentric virtual maze learning in adult survivors of childhood abuse with dissociative disorders: evidence from functional magnetic resonance imaging. Psychiatry Research, 212(2), 116–124. 10.1016/j.pscychresns.2012.11.004 [DOI] [PubMed] [Google Scholar]