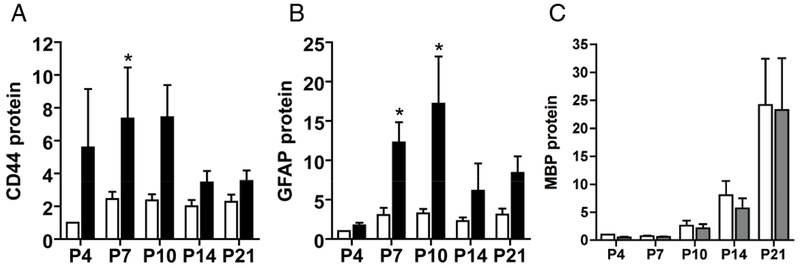
Figure 1. CD44 protein levels rapidly increase following neonatal hypoxic-ischemic injury.
To define how reactive gliosis, myelination and ECM remodeling are temporally related in evolving WMI, expression of GFAP (as a marker of reactive gliosis and injury), Myelin Basic Protein (MBP, as a marker of myelination) and the HA receptor CD44 was analyzed by western blot at five successive time points (n=18 animals/time point) after H-I between P4 and P21. H-I was induced as previously described (82) and generated unilateral WMI with the contralateral hemisphere serving as control. The data is presented as the mean fold-change for the 18 animals relative to the controls. (A, B) Chronic WMI led to a rapid increase in CD44 protein levels (panel A) in the lesions (black bars) compared to controls (unfilled bars). Note that increase in CD44 levels precede that of GFAP (panel B) suggesting that it could be used as a more sensitive indicator of WMI. C) The protein levels of the myelination marker, MBP, were lower in lesions relative to controls through P10. Additional studies employed area fraction analysis, which revealed significantly lower levels of MBP at P14 and P21 (70) in the WM lesions. Western blots did not detect such changes, which may have been related to the reduced sensitivity of this approach in anatomically complex white matter lesions.