Abstract
Von Hippel-Lindau (VHL) disease is an autosomal dominant inherited tumor syndrome. Clear cell chondrosarcoma (CCCS) is a rare variant of chondrosarcoma. Here, we report a case of CCCS in the talus occurring in a patient with VHL disease. A 32-year-old man presented with ankle pain for 2 years. MRI revealed a 4.2 cm mass in the talus, and needle biopsy was performed. The patient underwent curettage but the final diagnosis was CCCS. Adjuvant radiation therapy was performed without additional talectomy and the patient was alive without recurrence for a follow-up period of 2 years. To our knowledge, this is the first case in the English medical literature of a co-presentation of this rare disease and condition: i.e. CCCS with VHL disease in the unusual location of the talus. We cautiously suggest that CCCS may be associated with VHL disease based on their histologic similarity.
Keywords: Clear cell chondrosarcoma, talus, Von Hippel-Lindau disease
Introduction
Clear cell chondrosarcoma (CCCS) is a rare variant of chondrosarcoma, first described by Unni et al in 1976 [1] and characterized by proliferation of tumor cells with clear cytoplasm. CCCS comprises approximately 2% of all chondrosarcomas [2]. This tumor is most common in patients in the third to sixth decade, has a predilection for men, and typically arises at the ends of long bones [3].
Von Hippel-Lindau (VHL) disease is an autosomal dominant inherited tumor syndrome associated with germline mutation of the VHL tumor suppressor gene located on chromosome 3p25 [4]. It is characterized by the development of capillary hemangioblastoma of the central nervous system and retina, clear cell renal cell carcinoma, pheochromocytoma, and pancreatic and inner ear tumors [4]. VHL disease is estimated to occur at rates of 1:36,000 to 1:45,500 of the population [5].
We experienced an extremely rare case of CCCS in the talus with VHL disease. To the best of our knowledge, this is the first such case to be reported in the English literature.
Case presentation
Clinical features
A 32-year-old man presented with right ankle pain for 2 years, with symptoms aggravated over the previous 5 months. He had already undergone surgical removal of an hemangioblastoma in the medulla, and a bilateral partial nephrectomy for clear cell renal cell carcinoma 7 years prior, and a right adrenalectomy for pheochromocytoma 3 years prior. Cytogenetic analysis on peripheral blood at the time of the diagnosis for hemangioblastoma and renal cell carcinoma indicated VHL disease. On the initial bone scan during a metastasis work-up for the hemangioblastoma and renal cell carcinoma that were treated 7 years previously, a focal mildly increased uptake was observed in the talus, but this appeared non-specific. Two years later, a follow-up bone scan revealed a focally increased uptake in the right talus compared to the previous initial bone scan (Figure 1G) and the patient underwent magnetic resonance imaging (MRI). A round, eccentrically located, avidly-enhanced, 0.8 cm mass was detected in the right talar neck with a sclerotic rim on T1 and T2 weighted images (Figure 1A-C). Under the impression of a benign bone tumor such as osteoid osteoma or involvement of hemagioblastoma, the clinician decided to proceed with close follow-up observation. Follow-up bone scans over 5 years revealed a slowly growing mass in the talus (Figure 1H) and the last MRI revealed a well-marginated, slightly lobulated bony mass in the medial aspect of the talus, measuring about 4.4 × 2.0 × 4.2 cm (Figure 1D-F). The mass showed slightly inhomogeneous intermediate to high signal intensity with slightly inhomogeneous solid enhancement, containing focal hyper and low signal lesions. The radiologic impressions were primary bone tumor such as giant cell tumor, chondroblastoma, or osteoblastoma and less likely metastasis from renal cell carcinoma. A needle biopsy was performed and the tumor was initially diagnosed as chondroblastoma. After bone curettage, the diagnosis was changed to clear cell chondrosarcoma. Considering the patient’s history of renal cell carcinoma, no additional surgery for the talus was performed but additional radiation therapy was given. There has been no evidence of disease recurrence for 2 years.
Figure 1.
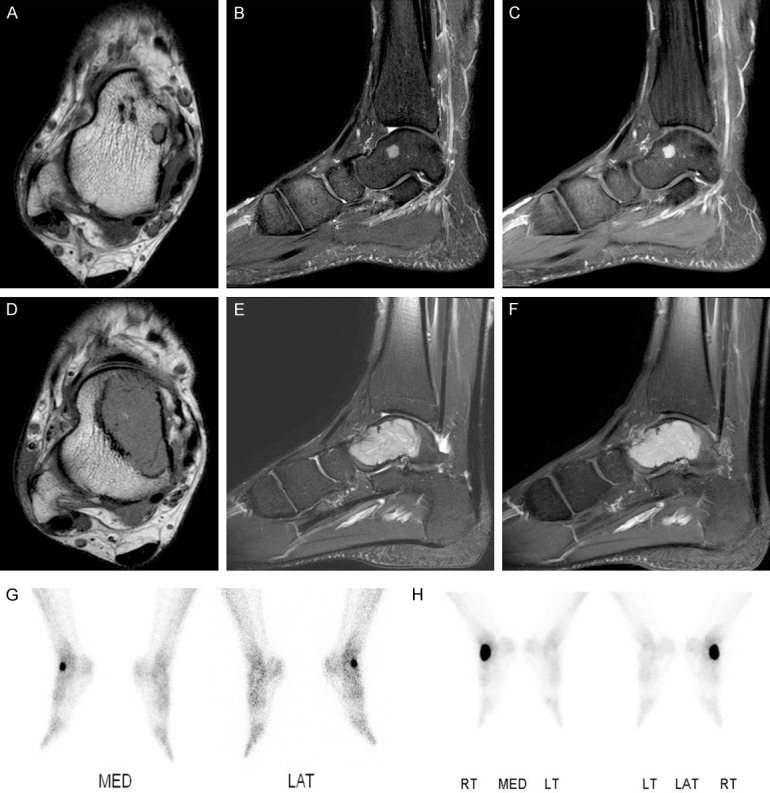
Radiologic findings. (A-F) Axial T1 weighted (A) and sagittal fat-saturated T2 weighted (B) images show a well-defined 0.8 cm, round mass with intermediate signal intensities eccentrically located in the right talar neck. (C) It shows prominent enhancement on sagittal enhanced fat-saturated T1 weighted image. Axial T1 weighted (D) and sagittal fat-saturated T2 weighted (E) images taken 5 years later show a slightly lobulated expansile 4.4 cm mass in the medial aspect of the talus. (F) The mass shows strong enhancement on sagittal enhanced fat-saturated T1 image. (G, H) Bone scans show focal increased uptake in the right talus initially (G) and an increased extent of hot uptake after 5 years (H), suggesting progression of the bone tumor.
Pathologic features
Grossly, the specimen was fragmented, pinkish brown, and soft but partly gritty. Microscopically, the tumor consisted of sheets of cells with large, round nuclei with central nucleoli. The cells had pale, clear or slightly eosinophilic cytoplasm with distinct cytoplasmic membranes (Figure 2A). The nuclear atypia was mild, and mitotic figures were seldom observed. Fine benign osteoid formation or woven bone was seen among the clear cells (Figure 2B). Osteoclast-like giant cells were occasionally present (Figure 2C). Mature hyaline cartilage was occasionally identified. No cystic changes were noted.
Figure 2.
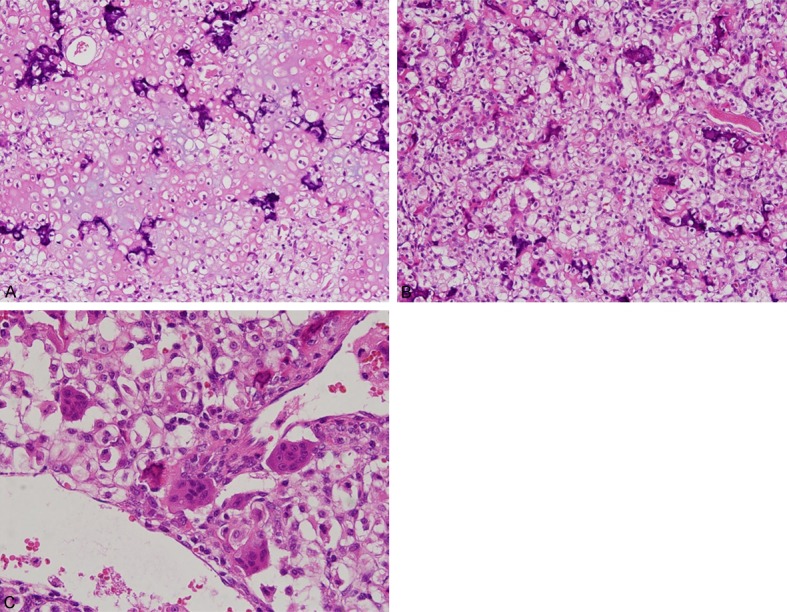
Microscopic findings. A. Low power photomicrograph shows sheets of clear cells with cartilaginous stroma. B. Sheets of clear cells are admixed with seams of woven bone. C. Osteoclastic type giant cells are scattered throughout the clear cells.
Immunohistochemistry
Tissues were fixed in buffered 10% formalin with decalcified solution and embedded in paraffin. The tissue blocks were sectioned at a thickness of 4 μm and mounted on precoated glass slides. The sections were deparaffinized, rehydrated and rinsed in distilled water. Immunohistochemical staining was performed for HIF1α (1:10,000, EPITOMICS, Cambridge, UK), IDH1 (1:100, DIANOVA, Hamburg, Germany), VEGF (1:500, PHARMINGEN, San Diego, CA), P16 (1:500, SANTACRUZ Biotechnology, Santa Cruz, CA), and S-100 protein (1:200, ZYMED, San Francisco, CA) using the Ventana NX automated immunohistochemistry system (Ventana Medical Systems, Tucson, AZ, USA). The tumor showed diffuse strong positivity for S-100 protein (data not shown) and, VEGF, and nuclear positivity for HIF1α with cytoplasmic staining of osteolclast-like giant cells. No IDH1 and p16 immunopositive tumor cells were identified (Figure 3A-D).
Figure 3.
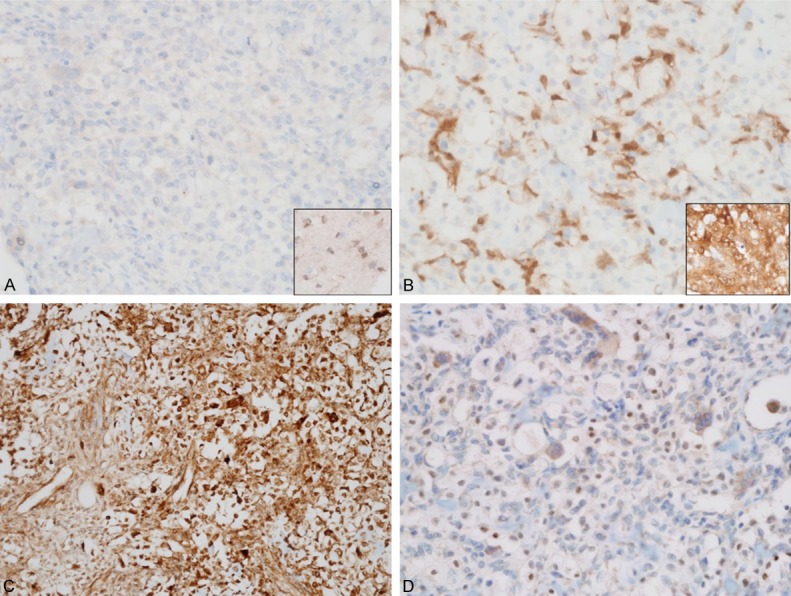
The tumor cells show immunonegativity for IDH1 (A) and p16 (B). The insets are control tissues: astrocytoma and cervical squamous cell carcinoma, respectively. (C, D) The tumor cells shows immunopositivity for VEGF (C) and HIF-1α (D), suggesting an indirect association of VHL disease.
Discussion
CCCS has been reported in long tubular bones including the skull, spine, hands and feet. The most frequent locations are the proximal femur (56%) and the head and neck area [6]. Only two cases of CCCS arising in talus have been reported in English [2,7]. Recognition of the usual site involvement of CCCS is important to prevent underdiagnosis and insufficient treatment.
Generally, CCCS belongs to the class of low grade sarcomas, and en-bloc excision with clear margin is usually curative. Marginal excision or curettage has been reported to have a high rate of local recurrence (86%) [3], with a number of patients eventually developing pulmonary metastases and died [8]. However, Present et al [2] reported that none of their patients with marginal or intralesional excision had recurrence during 5 to 9 years of follow-up. Based on the 5-year survival rates of stage I renal cell carcinoma is known to 81%, clear cell chondrosarcoma will not affect the survival of our patient. Thus, conservative surgery with adjuvant radiation therapy was acceptable in this case.
Radiologically, CCCS is typically lytic, although the lesion has areas of dense mineralization. Because this tumor extends to the epiphysis and articular cartilage, lytic lesions mimic chondroblastoma or giant cell tumor of the bone. Giant cell tumor of bone is easily excluded on microscopic examination. Histologically, major differential diagnoses are chondroblastoma, and chondroblastic osteosarcoma. In contrast to the marked pleomorphism, nuclear hyperchromasia, and brisk mitotic activity of chondroblastic osteosarcoma, the cells in CCCS are monomorphic and mitoses are rare. Compared to chondroblastoma, obviously malignant chondrocytes and large cells with clear cytoplasm often in a background of ossified bone are observed in CCCS.
VHL disease is an autosomal dominant multisystem syndrome associated with germline mutation of the VHL tumor suppressor gene at chromosome 3p25 [4]. The loss of functional VHL protein contributes to tumorigenesis in the central nervous system and internal organs, including the kidney, adrenal gland, and pancreas [4]. The current patient showed synchronous and metachronous existence of three primary tumors: hemangioblastoma, clear cell renal cell carcinoma, and pheochromocytoma. The relationship between VHL disease and CCCS is not well defined, because only one case report, which described chondrosarcoma and not clear cell chondrosarcoma, has been reported for VHL disease patient [9]. The mechanism of VHL syndrome in tumorigenesis involves hypoxia inducible factors (HIF1 and HIF2). Either hypoxia or absent or inactive VHL protein results in stabilization of HIF1 and HIF2, which then act as transcription factors that initiate the cellular cascade for a hypoxic response. This hypoxic response affects glucose uptake and metabolism, angiogenesis, extracellular matrix formation, chemotaxis and cell proliferation, and then activates downstream targets, including vascular endothelial growth factor (VEGF), platelet derived growth factor (PDGF), and transforming growth factor α [10]. Lin et al [11] reported that hypoxia induces HIF1α and VEGF expression in chondrosarcoma and Chen et al [12] reported that decreased VHL protein expression correlates with high grade chondrosarcoma. Our current case showed immunoreactivity for HIF1α and VEGF, indirectly suggesting a relationship between VHL disease and clear cell chondrosarcoma.
Clear cell chondrosarcoma also shares histologic similarity with other VHL disease-related tumors including epithelioid cell with clear cytoplasm and increased vascularity. Therefore, we cautiously suggest that clear cell chondrosarcoma in VHL syndrome is not an incidental coexistence, but rather that the VHL mutation may be related to the tumorigenesis of clear cell chondrosarcoma.
Similar to conventional chondrosarcoma, RB pathway is affected in the vast majority of CCCS, primarily through the loss of p16 protein expression [13]. In addition, it has been reported that mutations in IDH1/2 are absent in clear cell chondrosarcoma [14]. More specifically, protein expression of IDH1 by immunohistochemistry correlates with mutation in the IDH1 R132H gene (sensitivity 98% and specificity 100%) [15]. Our case showed also immunonegativity for p16 and IDH1, sharing common genetics with general clear cell chondrosarcoma.
In conclusion, clear cell chondrosarcoma can occur in VHL syndrome patients, and this is the first case to be reported in the English medical literature of this extremely rare combination, i.e. a rare subtype of chondrosarcoma, unusual location of the talus, and association with VHL disease.
Acknowledgements
This work was supported by a grant from National Research Foundation of Korea in 2017 (2017R1C1B5076919).
Disclosure of conflict of interest
None.
References
- 1.Unni KK, Dahlin DC, Beabout JW, Sim FH. Chondrosarcoma: clear-cell variant: a report of sixteen cases. J Bone Joint Surg Am. 1976;58:676–683. [PubMed] [Google Scholar]
- 2.Present D, Bacchini P, Pignatti G, Picci P, Bertoni F, Campanacci M. Clear cell chondrosarcoma of bone: a report of 8 cases. Skeletal Radiol. 1991;20:187–191. doi: 10.1007/BF00241664. [DOI] [PubMed] [Google Scholar]
- 3.Bjornsson J, Unni KK, Dahlin DC, Beabout JW, Sim FH. Clear cell chondrosarcoma of bone: observations in 47 cases. Am J Surg Pathol. 1984;8:223–230. doi: 10.1097/00000478-198403000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, Oldfield EH. von Hippel-Lindau disease. Lancet. 2003;361:2059–2067. doi: 10.1016/S0140-6736(03)13643-4. [DOI] [PubMed] [Google Scholar]
- 5.Maddock IR, Moran A, Maher ER, Teare MD, Norman A, Payne SJ, Whitehouse R, Dodd C, Lavin M, Hartley N, Super M, Evans DG. A genetic register for von Hippel-Lindau disease. J Med Genet. 1996;33:120–127. doi: 10.1136/jmg.33.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F. WHO classification of tumors of soft tissue and bone. Lyon: IARC; 2013. [Google Scholar]
- 7.Ogose A, Motoyama T, Hotta T, Emura I, Inoue Y, Morita T, Watanabe H. Clear cell chondrosarcomas arising from rare sites. Pathol Int. 1995;45:684–690. doi: 10.1111/j.1440-1827.1995.tb03522.x. [DOI] [PubMed] [Google Scholar]
- 8.Itala A, Leerapun T, Inwards C, Collins M, Scully SP. An institutional review of clear cell chondrosarcoma. Clin Orthop Relat Res. 2005;440:209–212. doi: 10.1097/01.blo.0000174686.70003.e0. [DOI] [PubMed] [Google Scholar]
- 9.Marinozzi A, Papapietro N, Barnaba SA, Di Martino A, Tonini G, Denaro V. Chondrosarcoma of the iliac wing in Von Hippel-Lindau disease. J Exp Clin Cancer Res. 2007;26:599–601. [PubMed] [Google Scholar]
- 10.Kaelin WG Jr. The von Hippel-Lindau tumour suppressor protein: O2 sensing and cancer. Nat Rev Cancer. 2008;8:865–873. doi: 10.1038/nrc2502. [DOI] [PubMed] [Google Scholar]
- 11.Lin C, McGough R, Aswad B, Block JA, Terek R. Hypoxia induces HIF-1alpha and VEGF expression in chondrosarcoma cells and chondrocytes. J Orthop Res. 2004;22:1175–1181. doi: 10.1016/j.orthres.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Zhou H, Liu X, Liu Z, Ma Q. Reduced expression of von Hippel-Lindau protein correlates with decreased apoptosis and high chondrosarcoma grade. J Bone Joint Surg Am. 2011;93:1833–1840. doi: 10.2106/JBJS.I.01553. [DOI] [PubMed] [Google Scholar]
- 13.Meijer D, de Jong D, Pansuriya TC, van den Akker BE, Picci P, Szuhai K, Bovee JV. Genetic characterization of mesenchymal, clear cell, and dedifferentiated chondrosarcoma. Genes Chromosomes Cancer. 2012;51:899–909. doi: 10.1002/gcc.21974. [DOI] [PubMed] [Google Scholar]
- 14.Nishio J, Reith JD, Ogose A, Maale G, Neff JR, Bridge JA. Cytogenetic findings in clear cell chondrosarcoma. Cancer Genet Cytogenet. 2005;162:74–77. doi: 10.1016/j.cancergencyto.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Jabbar KJ, Luthra R, Patel KP, Singh RR, Goswami R, Aldape KD, Medeiros LJ, Routbort MJ. Comparison of next-generation sequencing mutation profiling with BRAF and IDH1 mutation-specific immunohistochemistry. Am J Surg Pathol. 2015;39:454–461. doi: 10.1097/PAS.0000000000000325. [DOI] [PubMed] [Google Scholar]


