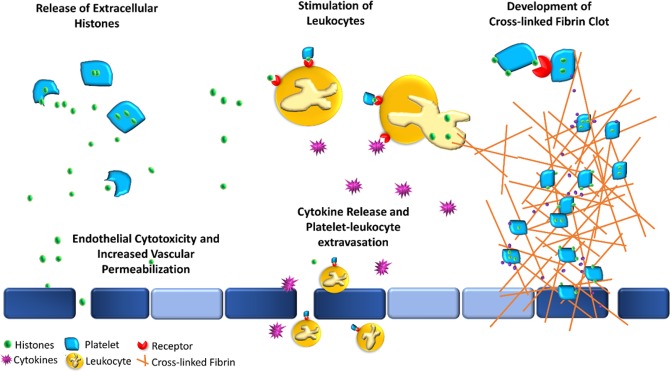
Figure 6.
Proposed potential sequela of platelet-associated histones. Visual representation of some of the potential interactions of platelet-associated histones (PAHs) with the immune and coagulation system. Platelets (light blue polygons) may either release extracellular histones (green circles) upon stimulation or express them on their cell membranes. The release of extracellular histones (top left) may result in direct cytotoxicity of endothelial and epithelial cells (dark blue rectangles), resulting in both, increased vascular permeability, and a prothrombotic surface. The presence of PAHs and extracellular histones may serve as an additional binding antigen between platelets and leukocytes (orange circle) (top middle) via various receptors (red), including TLRs, and may result in the development of circulating platelet-leukocyte aggregates (PLAs) and stimulate the cells to increase production and release inflammatory cytokines (purple stars). These PLAs can then either diapedese across the endothelium or escape through the increase endothelial permeability into extravascular tissue (bottom middle) and further propagate inflammation. Thrombosis may be initiated and propagated through various mechanisms (right), where PAHs can bind to each other through TLR receptors (top right) which can result in subsequent platelet activation and an increase in thrombin generation and release (purple circles). Circulating histones are also themselves, prothrombotic and anti-fibrinolytic, promoting thrombosis. These PAHs and free circulating histones may also stimulate leukocytes, such as neutrophils, to form extracellular traps, further propagating inflammation and coagulation.