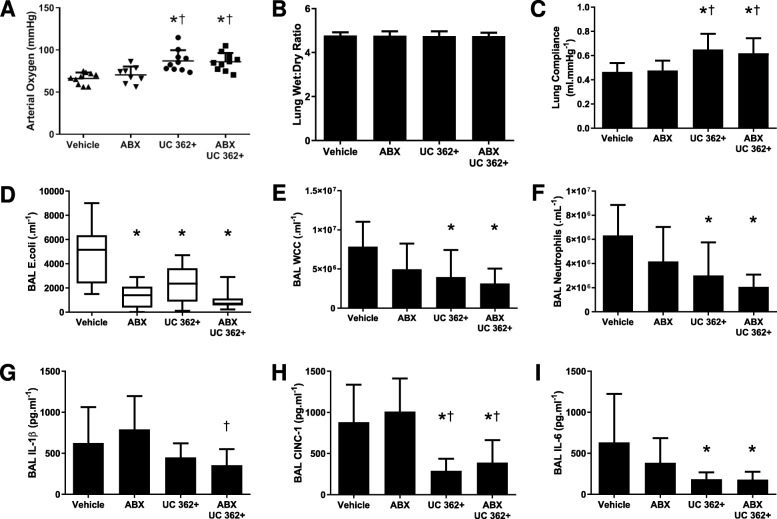
Fig. 2.
CD362+ UC-hMSCs decrease E. coli-induced lung injury in the presence of antibiotic therapy. CD362+ UC-hMSCs reduced the decrement in arterial oxygenation in the presence or absence of antibiotic therapy compared to vehicle, but antibiotic alone was ineffective (a). There was no effect of any treatment on lung wet to dry ratio (b). CD362+ UC-hMSCs, with or without antibiotics, reduced the decrease in lung static compliance (c), while all therapy groups reduced BAL E. coli bacterial load (d). CD362+ UC-hMSC therapy, with or without antibiotics, reduced both total leukocyte (e) and neutrophil (f) counts in the BAL, where antibiotic alone did not. No therapy regimen reduced IL-1β concentrations with respect to vehicle control, although CD362+ UC-hMSCs reduced levels compared to antibiotic therapy alone (g). CD362+ UC-hMSCs significantly reduced BAL CINC-1 (h), and IL-6 (i) concentrations in the presence or absence of antibiotic therapy where antibiotic therapy alone did not. Abbreviations: vehicle, treatment with vehicle alone; ABX, antibiotic therapy; UC 362+, umbilical cord-derived CD362+ hMSC. BAL, bronchoalveolar lavage; CINC-1, cytokine-induced neutrophil chemoattractant 1; IL-6, interleukin 6; IL-1β, interleukin 1 beta; vehicle, treatment with vehicle alone. Error bars represent standard deviation. *Significantly (P < 0.05) different from vehicle control group. †Significantly (P < 0.05) different from the ABx therapy group