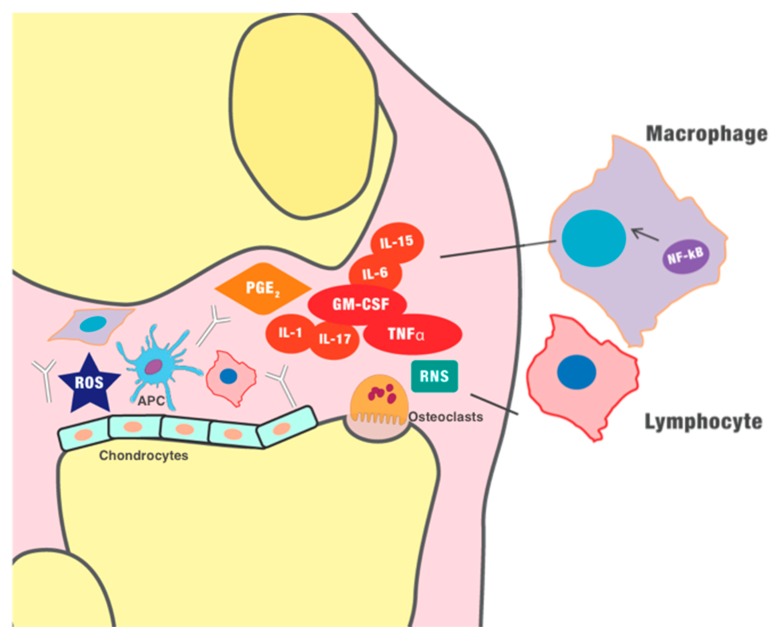
Figure 2.
Pathogenesis of inflammatory arthritides. Self-reactive T helper cells seem involved in the maintenance of inflammation, further sustained by B cells, especially in rheumatoid arthritis (RA), where it is possible to detect autoantibodies ( ), such as the rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibodies. Furthermore, innate immunity is involved in chronic inflammation. Granulocyte-macrophage colony-stimulating factor (GM-CSF) induces the differentiation of the macrophages. Monocytes and macrophages, as well as dendritic cells, seem to play a vital role in the pathogenesis of inflammatory arthritis, as antigen-presenting cells (APCs), and they can express several pro-inflammatory cytokines. In early stages of inflammation, hypoxia and the production of ROS (reactive oxygen species) and RNS (reactive nitrogen species) seems to play a role in the initiation of the inflammatory process and induction of angiogenesis. The new blood vessels further maximize the recruitment of immune cells, amplifying the inflammatory process. The chronic inflammation finally perpetuates the production of pro-inflammatory cytokines (such as tumor necrosis factor-α (TNF-α)) and other mediators, such as prostaglandin E2, which ultimately generate vasodilation, infiltration of immune cells, and destruction of the cartilage.
), such as the rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibodies. Furthermore, innate immunity is involved in chronic inflammation. Granulocyte-macrophage colony-stimulating factor (GM-CSF) induces the differentiation of the macrophages. Monocytes and macrophages, as well as dendritic cells, seem to play a vital role in the pathogenesis of inflammatory arthritis, as antigen-presenting cells (APCs), and they can express several pro-inflammatory cytokines. In early stages of inflammation, hypoxia and the production of ROS (reactive oxygen species) and RNS (reactive nitrogen species) seems to play a role in the initiation of the inflammatory process and induction of angiogenesis. The new blood vessels further maximize the recruitment of immune cells, amplifying the inflammatory process. The chronic inflammation finally perpetuates the production of pro-inflammatory cytokines (such as tumor necrosis factor-α (TNF-α)) and other mediators, such as prostaglandin E2, which ultimately generate vasodilation, infiltration of immune cells, and destruction of the cartilage.  , dendritic cell/APC;
, dendritic cell/APC;  , osteoclast;
, osteoclast;  , chondrocyte.
, chondrocyte.