Abstract
The role of forkhead box O3 (FOXO3) as a tumor suppressor gene and its association with the human lifespan is well documented. However, several studies have indicated that high expression of FOXO3 is also significantly associated with tumorigenesis. The aim of the present study was to determine the clinical significance of FOXO3 in the development and prognosis of hepatocellular carcinoma (HCC). mRNA expression data of FOXO3 from The Cancer Genome Atlas database was analyzed through the UALCAN online tool to compare the expression of FOXO3 between HCC and normal liver tissues. Subsequently, the expression of FOXO3 at the protein level was investigated via immunohistochemical staining of 314 HCC and 150 non-cancerous liver tissue samples. The association between protein expression and clinicopathological parameters was analyzed using the χ2 test, and the effect of FOXO3 expression on survival was assessed via Kaplan-Meier analysis. The expression of FOXO3 mRNA was significantly higher in HCC in comparison with healthy tissues. High FOXO3 protein expression was revealed in 43/150 non-cancerous liver tissues, and in 238/314 HCC samples. A significant association was demonstrated between FOXO3 expression and metastasis, Tumor-Node-Metastasis stage, Edmondson grade, α-fetoprotein level and overall survival. In conclusion, the high expression of FOXO3 predicts a poor prognosis in patients with HCC, indicating this protein as a potential therapeutic target in HCC.
Keywords: forkhead box O3, hepatocellular carcinoma, prognosis
Introduction
Hepatocellular carcinoma (HCC) is the most common primary malignant tumor affecting the digestive system. According to literature reports, the 2018 global cancer statistics show that the incidence of liver cancer ranks sixth among malignant tumors and the mortality rate ranks fourth globally (1). The global incidence of HCC has increased in the last 2 decades, with the primary risk factor being hepatitis C infection in Europe, North America and Japan, and hepatitis B virus in Asia and Africa (2,3). Non-viral risk factors for HCC include alcoholic cirrhosis, non-alcoholic steatohepatitis and hereditary hemochromatosis, but the specific pathogenesis is yet to be elucidated (4,5). The majority of patients with HCC are diagnosed at an advanced stage of the disease, and the most common treatments include liver transplantation, surgical resection, radio- and chemotherapy, and biological immunotherapy (6,7). However, current treatments are relatively ineffective, as reflected by the high recurrence rate and low 5-year survival rate of patients with HCC in China. Therefore, the identification of specific biomarkers and molecular mechanisms that influence the pathogenesis of HCC is critical to facilitate the early diagnosis of this disease. Potential biomarkers may include endogenous tumor factors, which regulate tumor cell proliferation, progression and invasiveness (8). Investigating these may result in a better understanding of the mechanisms underlying tumor progression and metastasis, and identify tumor markers specific to HCC.
The forkhead box (FOXO) family represents a group of transcription factors, which serve a critical function in higher organisms by regulating the antioxidant response, gluconeogenesis, apoptosis and autophagy (9). The FOXO family comprises four proteins: FOXO1, FOXO3, FOXO4 and FOXO6. Several studies have documented that FOXO proteins are crucial regulators in the progression of liver disease and influence the prognosis (10–12). In a healthy liver, FOXO regulates glucose and lipid metabolism, autophagy and the adaptation to starvation (11). The influence of FOXO expression on liver lipid metabolism has been demonstrated via simultaneous knockouts of the FOXO1 and FOXO3 proteins, which resulted in enhanced lipid secretion in the liver, an increase in serum triglyceride levels and increase the incidence of hepatic steatosis (12). Similarly, a liver-specific knockout of various combinations of FoxO1, FoxO3 and FoxO4 in mice, through downregulated expression of the nicotinamide phosphoribosyl transferase gene resulted in lipid accumulation in the liver (13), further indicating the role of FOXO in the regulation of lipid metabolism, with dysfunctional protein resulting in liver steatosis. However, despite mounting evidence that FOXO3 serves an important role in the pathogenesis of liver disease, the function of this protein as a tumor suppressor in HCC, is yet the be elucidated.
The FOXO3 gene, first identified in human placental cosmid, is located on chromosome 6q21 (14). Its protein product localizes within the nucleus and, upon activation, binds DNA, regulating the expression of genes such as FKHRP1and FKHRL1 that modulate metabolic state, cell cycle and apoptosis (15–17). FOXO3, also known as FOXO3a, is a member of the forkhead transcription factor family and serves an essential function in tumor progression. It has been revealed that FOXO3 is involved in neoplastic cell transformation, tumor progression and angiogenesis; these processes are mediated by specific activation of a coordinated transcriptional program and serve a vital role in the regulation of a variety of cellular processes, which may be associated with abnormal regulation of the PI3K/Akt pathway (18–20). The change in the expression of FOXO results in increased cell proliferation and DNA damage, promoting tumorigenesis. The change in the expression of FOXO is associated with abnormal post-translational regulation. Notably, a similar effect can result from the increased expression of FOXO3 (21). Recently, FOXO3 has been demonstrated to be associated with increased lymph node metastasis in esophageal squamous cell carcinoma (ESCC). This association is apparent in advanced clinical stages, in which FOXO3 upregulation inhibits the ability of microRNA-10b-3p to promote tumor invasion and metastasis (22), indicating that FOXO3 inhibits ESCC tumor growth and metastasis. Moreover, in colon cancer cell lines, increased expression and activation of epidermal growth factor receptor (EGFR) enhanced phosphorylation of FOXO3, promoting cancer cell proliferation (23). Together, the aforementioned results indicate that FOXO3 inhibits tumor growth. However, results to the contrary have also been reported. Overexpression of FOXO3 is associated with poor prognosis in patients with triple-negative breast cancer (24), glioblastoma (25) and gastric cancer (26), and low expression of FOXO3 was discovered in glioma and ovarian cancer cells (27,28). These contrasting results suggest that FOXO3 serves different roles in different types of tumors.
To investigate the role of FOXO3 in HCC, its influence on the genesis and progression of this type of tumor, as well as its association with clinical features and patient prognosis, was examined. To this purpose, the expression of FOXO3 in 314 HCC and 150 non-cancerous liver tissues was examined using immunohistochemistry (IHC). Additionally, a meta-analysis using The Cancer Genome Atlas (TCGA) database was performed to evaluate the association of FOXO3 expression with clinicopathological parameters. The present study may allow further insight into the biological function of FOXO3 in different types of cancers.
Materials and methods
UALCAN analysis of FOXO3 gene expression were conducted in HCC, including 371 cases of HCC and 50 cases of normal liver tissue. UALCAN was utilized to compare the difference in expression of FOXO3 between HCC and normal liver tissues, using datasets retrieved from TCGA database. All UALCAN data is publicly available from http://ualcan.path.uab.edu. This site facilitates analysis of the relative expression of query genes between tumor and normal tissues, and also between various subgroups, including tumor grade, individual cancer stage and other clinicopathological features.
Preliminary study on genes interacting with FOXO3
This database can be easily retrieved through the search function provided by the official website. Search by protein name, sequence, etc. The Search Tool for Retrieval of Interacting Genes and Proteins database (STRING-DB; www.bioconductor.org) was used to construct a protein-protein interaction (PPI) network in order to analyze the role of the FOXO3 gene in regulating the expression.
Patients and tissue samples
All human tissues and clinicopathological parameters were collected via surgical resection of 300 patients with HCC between April 2010 and September 2016 at Zhejiang Provincial People's Hospital (Hangzhou, China). The present study was approved by the Ethics Committee of Zhejiang Provincial People's Hospital and written informed consent was provided by all patients. All tissues were used for the preparation of a tissue microarray (TMA), which was constructed by Shanghai BioChip Co., Ltd. The TMAs included 314 cases of paraffin-embedded HCC tissues and 150 samples of non-cancerous liver tissue from healthy controls. The survival time was calculated from the date of surgery to the time of the follow-up deadline (death if patient) or the date at which patients succumbed to the disease, followed up by telephone once every three months.
Clinicopathological parameters
All patients' clinicopathological parameters were collected via surgical resection including α-fetoprotein (AFP), Tumor-Node-Metastasis (TNM) and Edmondson grade. The TNM tumor staging method was established by Pierr Denoix in 1943, the Japanese Liver Cancer Research Association first used to assess the prognosis of liver cancer (29). In 1988, the American Cancer Association (AJCC) and the International Union Against Cancer (UICC) began to use TNM staging. Tumor status (T), lymph node invasion (N), and presence or absence of distant metastases (M) to stage tumors (30). The Edmondson-Steiner classification (31) divides liver cancer into four types according to the degree of cancer cell differentiation. Type 1 cancer tissues are arranged in thin beams (trabecular cord type), with high degree of differentiation and long natural doubling time. Type 2 cancer cells have large nuclei, are densely stained, have a rich cytoplasm, are eosinophilic, and are often arranged in a glandular or acinar shape. Type 3 cancer cells have enlarged and densely stained nuclei, which are heavier than type 2 cells, and more tumor giant cells are found, which are poorly differentiated. Type 4 nucleus is strongly concentrated and occupies most of the cells, the cytoplasm is often lacking. It grows like a myeloid and is rarely beam-like. This type has the lowest differentiation (32).
IHC staining
IHC staining was performed using standard methodology. Briefly, 5-µm thick sections were excised from the TMAs and incubated at 70°C for 2 h. Subsequently, the sections were deparaffinized, rehydrated using a gradient of ethanol concentrations (95, 90 and 80%), microwaved in 10 mM citrate buffer for 15 min for antigen retrieval, blocked with 3% hydrogen peroxide for 10 min to inhibit endogenous peroxidase activity, and incubated with 10% non-immune goat serum (OriGene Technologies, Inc.) for 20 min to reduce non-specific background staining; these reactions were performed at room temperature. Sections were then incubated with the mouse anti-FOXO3 polyclonal antibody (1:800 dilution; cat. no. ab23683; Abcam) at 4°C overnight, followed by incubation with biotin-labeled secondary antibody (Goat anti-Mouse IgG HRP; cat. no. 32230; Invitrogen; Thermo Fisher Scientific, Inc.) at room temperature for 20 min, and horseradish peroxidase-conjugated streptavidin (Invitrogen; Thermo Fisher Scientific, Inc.) at room temperature for 20 min. The color was developed using a 3,3′-diaminobenzidine substrate kit (Dako; Agilent Technologies, Inc.). Finally, the sections were counterstained with haematoxylin for 5 min and dehydrated for 45 min at room temperature, and mounted. Images were captured using a light microscope at magnifications, ×40 and ×400.
The IHC staining of FOXO3 was randomly assigned to be scored independently by two pathologists, who were blinded to the study, based on the intensity and the proportion of positively stained cells. Staining intensity was evaluated using a four-tiered grading system: 0, negative; 1, weak; 2, moderate; and 3, strong. The percentage of positive cells stained were scored as follows: 0, no staining; 1, 1≤1<25%; 2, 25%≤2<50%; 3, 50%≤3<75%; and 4, ≥75% of cells stained. To obtain the final score, the intensity scores were multiplied by the percentage scores. Tumor samples with a score of ≤2 were termed low-FOXO3 expression, while a score of ≥3 defined tumors with high FOXO3 expression.
Statistical analysis
Statistical analysis was performed using the Statistical Program for Social Sciences software v13.0 (SPSS, Inc.). The χ2 test was used to assess the statistical significance of associations between FOXO3 protein expression and various clinicopathological parameters. Survival curves were evaluated using the Kaplan-Meier method, and the log-rank test was used to determine the statistical significance of the differences between the curves. P<0.05 was considered to indicate a statistically significant difference. For groups comprising ≥3 members, ANOVA with Dunnett's post-hoc test was used when data were normally distributed, and Kruskal-Wallis with Dunn's post hoc test was used if the data were not normally distributed.
Results
Analysis of FOXO3 expression based on TCGA database
The difference in the expression of FOXO3 between HCC (n=371) and normal liver tissue (n=50) was determined using TCGA database. The expression level of FOXO3 in HCC was significantly higher compared with that in non-cancerous liver tissue (P<0.001; Fig. 1A).
Figure 1.
Expression of FOXO3 according to The Cancer Genome Atlas database. (A) Expression of FOXO3 in normal liver and HCC tissues. Association between FOXO3 expression and (B) clinical TNM staging of HCC, and (C) histological grade of HCC. ***P<0.001. FOXO3, forkhead box O3; HCC, hepatocellular carcinoma.
Association between FOXO3 expression and clinicopathological parameters
The association between the expression of FOXO3 and various clinical variables is listed in Table I. A statistically significant association was found between the expression of FOXO3 and Edmondson grade, presence of metastases, Tumor-Node-Metastasis (TNM) stage, survival status, and level of α-fetoprotein (AFP). No significant associations were observed between Foxo3 expression and other clinical pathological parameters. The analysis of TCGA datasets revealed the expression of FOXO3 varied between different clinical TNM stages (Fig. 1B). The median expression was 5.558 in normal (n=50), 6.387 in stage 1 (n=168), 6.42 in stage 2 (n=84), 6.819 in stage 3 (n=82) and 7.639 in stage 4 (n=6). The positive rate of FOXO3 is higher in the III and IV stages compared with stages I and II. Furthermore, analysis of TCGA database indicated that the expression of FOXO3 in HCC was associated with pathological grade (Fig. 1C). The median expression of FOXO3 at various tumor grades was as follows: 1, 6.108 (n=54); 2, 6.765 (n=173); 3, 6.964 (n=118); and 4, 7.132 (n=12). The expression of FOXO3 in tumors with high Edmondson grade, presence of metastasis, high TNM stage and high AFP level was significantly higher compared with that in tumors with low Edmondson grade and low AFP level.
Table I.
Association between FOXO3 expression and clinicopathological parameters of patients with hepatocellular carcinoma recruited for this study.
| FOXO3 expression | ||||
|---|---|---|---|---|
| Clinical parameters | Total, n | Low | High | P-value |
| Age, years | ||||
| <55 | 120 | 71 | 49 | 0.395 |
| ≥55 | 194 | 119 | 75 | |
| Sex | ||||
| Male | 255 | 155 | 100 | 0.474 |
| Female | 59 | 35 | 24 | |
| Size, cm | ||||
| <5 | 168 | 104 | 64 | 0.392 |
| ≥5 | 139 | 83 | 56 | |
| Tumor number | ||||
| Single | 257 | 152 | 105 | 0.184 |
| Multiple | 57 | 38 | 19 | |
| Edmondson Grade | ||||
| I+II | 195 | 138 | 57 | <0.001 |
| III | 116 | 49 | 67 | |
| Metastasis | ||||
| M0 | 282 | 175 | 107 | 0.026 |
| M1 | 27 | 11 | 16 | |
| Microvascular invasion | ||||
| Absence | 136 | 87 | 49 | 0.061 |
| Presence | 91 | 48 | 43 | |
| TNM Stage | ||||
| I + II | 196 | 139 | 57 | <0.001 |
| III+IV | 116 | 49 | 67 | |
| AFP, µg/l | ||||
| <50 | 138 | 104 | 34 | <0.001 |
| ≥50 | 117 | 43 | 74 | |
| Status | ||||
| Alive | 141 | 101 | 30 | <0.001 |
| Dead | 72 | 30 | 42 | |
The clinical information of a small number of patients was lost during the statistical analysis. FOXO3, forkhead box O3.
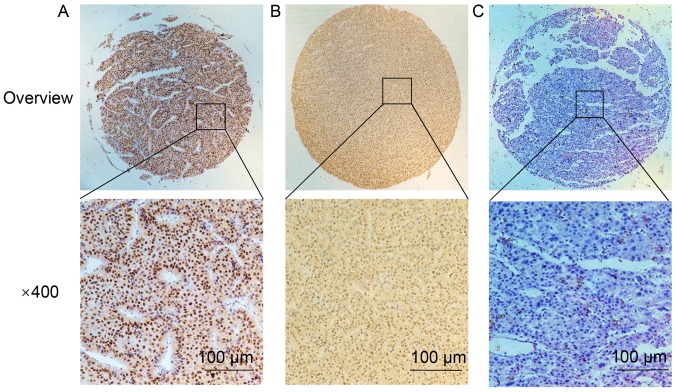
Analysis of FOXO3 expression via IHC
IHC staining demonstrated that FOXO3 protein was upregulated in HCC tissues, with strong staining localized in the nucleus (Fig. 2). FOXO3 was upregulated in 238/314 (75.80%) HCC tissues. The expression of FOXO3 was significantly lower in non-cancerous liver tissue; FOXO3 was upregulated in 43/150 (28.67%) samples. The difference in expression of FOXO3 protein was statistically significant, with higher IHC scores in cancerous tissues (P=0.0081; Table II).
Figure 2.
Results of FOXO3 immunohistochemistry. Staining of HCC tissues revealed (A) Strong expression; (B) moderate expression; and (C) no expression of FOXO3 in HCC tissues. Magnifications, ×40 and ×400. FOXO3, forkhead box O3.
Table II.
Expression of FOXO3 in HCC and non-cancerous liver tissues.
| FOXO3 expression | ||||
|---|---|---|---|---|
| Tissue type | Total, n | Low | High | P-value |
| HCC | 314 | 76 | 238 | 0.0081 |
| Healthy liver | 150 | 107 | 43 | |
HCC, hepatocellular carcinoma; FOXO3, forkhead box O3.
Identification of genes interacting with FOXO3 and gene set functional enrichment analysis
Genes that interact with FOXO3 include CDKN1B, AKT1, SMAD4, SOD2, BCL2L11, SIRT1, EP300, SGK1, AKT2 and CREBBP. Functional enrichment analysis of genes interacting with FOXO3 revealed that the FOXO3 gene serves a key role in the transcription and regulation via PPI enrichment; 11 nodes were identified (P=2.83×10−5; Fig. 3).
Figure 3.
Location of the FOXO3 gene in the mitochondrial gene transcription and its interaction genes. The functional enrichment analysis of genes interacting with FOXO3 revealed that the FOXO3 gene serves a key role in the transcription and regulation of genes. FOXO3, forkhead box O3.
Survival analysis
The mean survival time of patients with high FOXO3 expression in HCC tissue was 30.17±1.74 months, which was significantly shorter compared with patients in the low-FOXO3 expression group, 50.60±2.82 months (P<0.001; Fig. 4A). These results are consistent with TCGA database, the higher expression of FOXO3 in cancer tissues the survival rate was lower (P=0.0083; Fig. 4B).
Figure 4.
Kaplan-Meier survival curves of patients with HCC with high or low FOXO3 expression. (A) Kaplan-Meier survival curves of patients recruited in the present study with HCC and high or low FOXO3 expression. (B) Kaplan-Meier analysis of TCGA dataset describing the effect of FOXO3 expression level on survival time of patients with HCC. The present results are consistent with TCGA database, the higher expression of FOXO3 in cancer tissues the survival rate was lower. HCC, hepatocellular carcinoma; FOXO3, forkhead box O3; TGCA, The Cancer Genome Atlas.
Discussion
In China, there is a high incidence of liver cancer and HCC represents the most frequent subtype of cancer of the liver and is characterized by poor prognosis. In 2015, 466,100 people were diagnosed with liver cancer and 422,100 individuals succumbed to this disease in China (33). At present, surgery is the most effective option for the treatment of localized HCC; however, when HCC metastasizes, the effectiveness of surgery significantly decreases, in addition to the patient survival rate (34). Therefore, identification of specific molecular markers that are involved in the malignant progression of HCC is crucial to facilitate the early diagnosis and treatment of the disease (35–37).
Following investigation into the molecular basis and pathogenesis of liver cancer, it has been confirmed that signal transduction pathways and increased neovascular proliferation are involved the occurrence, development and metastasis of liver cancer (38). In the past years, molecular targeted drugs have attracted attention and become novel research hotspots. As a class of molecular targeted drugs, small molecule tyrosine kinase inhibitors (TKIs) have become one of the mainstream drugs used in anti-hepatocarcinoma research (39). TKIs block signaling pathways by inhibiting kinase activity, tumor growth and cell proliferation, resulting in antitumor effects (40), and improving the prognosis of patients with cancer. Sorafenib, replilinide, lenvatinib and cabozantinib are TKIs that are partially targeted to vascular endothelial growth factor receptors and are approved worldwide for the treatment of advanced HCC. A disadvantage of TKIs is that their use can result in adverse side effects, including fatigue, diarrhea, hand-foot skin reaction, nausea, vomiting, loss of appetite, high blood pressure and weight loss (41). The clinical application of TKIs requires careful consideration of safety and efficacy (42). Therefore, it is particularly important to explore novel targeted therapies for HCC.
FOXO3 has a relative molecular mass of ~71 kDa and contains five domains: a highly conserved forked-winged helix-turn-helix DNA binding domain (FKH), two nuclear localization sequences (NLS), one nuclear export sequence and one C-terminal transactivation domain (TAD) (43). The highly conserved FKH domain primarily regulates the interaction between FOXO3 and DNA, and also mediates its interaction with estrogen receptor α (44) and tumor protein p53 (p53) protein (45). The translocation of FOXO3 from the cytoplasm to the nucleus requires the NLS domain, which mediates the release of FOXO3 from the nucleus. The C-terminal TAD domain is critical for the transactivation of FOXO3 target genes. FOXO3 is phosphorylated by upstream kinases such as AKT, ERK, serum/glucocorticoid regulated kinase 1, inhibitor of nuclear factor-κB kinase subunit β and inhibitor of nuclear factor-κB kinase subunit ε. The dysregulation of these kinases often occurs in different types of cancer and facilitates tumor progression by promoting the FOXO nuclear-cytoplasmic shuttle or ubiquitin-dependent protein kinase degradation (46–49). The carcinogenic effects of FOXO3 dysfunction are mediated by a variety of mechanisms that involve several genes associated with apoptosis, such as Bim, Noxa, Puma, Fasl and TRAIL, in addition to genes controlling cell proliferation, such as p21, p27, p130, cyclin G2 and GADD45 (45). Therefore, the increased expression of the FOXO3 gene is associated with the incidence of cancer.
FOXO3 has been revealed as a potential biomarker for the diagnosis, prognosis and monitoring of treatment in a variety of malignancies. For example, FOXO3 high expression was identified as a biomarker in cells with Hodgkin's lymphoma phenotype (50), and the potential of FOXO3 high expression as a prognostic biomarker for a variety of cancer types has been demonstrated in several studies, such as in breast cancer and glioblastoma (24–26,51). The current study identified that FOXO3 was significantly upregulated in HCC, compared with normal liver tissue, this may indicate that the expression of FOXO3 in HCC cancer is tissue-specific. Notably, the current results also revealed that high expression of FOXO3was found in 28.67% of normal tissues and it was ~24.2% lower in HCC tissues. This may be attributable to differences in the population recruited for the present study. Therefore, further large-scale studies are required to confirm the utility of FOXO3 as a biomarker for HCC.
The increased expression of phosphorylated FOXO3 was also identified as a prognostic biomarker for ovarian cancer and acute myeloid leukemia (52), and its nuclear localization was demonstrated to be a prognostic biomarker for ductal carcinoma of the breast (53). In addition, the subcellular localization of FOXO3 was revealed to be a predictor of response to chemo- and radiotherapy in cervical, breast and esophageal cancer (54). The present study revealed that the expression level of FOXO3 was significantly associated with Edmondson grade (P<0.001), TNM stage (P<0.001), presence of metastases (P<0.05) and increased AFP level (P<0.001). Additionally, the mean survival time and 5-year survival rate were significantly lower in patients with high FOXO3 expression, compared with the lower expression group. High expression of FOXO3 was significantly associated with a poor prognosis, indicating that FOXO3 may serve as a prognostic marker in patients with HCC, and may influence tumor progression. Notably, FOXO3 is highly expressed in HCC and is associated with poor prognosis. The results of the IHC analysis in the present study were consistent with the data retrieved from TCGA repository.
FOXO3 serves as a transcription factor, which binds the transcriptional regulatory binding domain of various target genes in the nucleus through the PI3K-AKT signaling pathway (55). Therefore, FOXO3 regulates multiple signaling pathways as key nodes in tumor cells. HCC is characterized by activation of the Wnt signaling pathway, which serves an important role in the development and malignant progression of liver cancer (56). In addition, FOXO3 interacts with multiple intracellular signaling factors such as β-catenin, P53 and MYC proto-oncogene bHLH transcription factor, in the Wnt pathway (57–60). Therefore, FOXO3 serves a multi-step regulatory role in cells; involved in self- and mutual regulation, and selective expression of target genes, such as insulin-like growth factor receptor 1 and PI3KCA. Notably, the importance of investigating its role as a regulatory factor in the field of HCC treatment has been demonstrated in the aforementioned literature, and may provide theoretical evidence for improving the limitations in HCC treatment, and assist with elucidating the underlying biological characteristics of FOXO3.
In conclusion, the evaluation of FOXO3 expression may represent a potential auxiliary test for use in the diagnosis of HCC. Moreover, since upregulation of FOXO3 in HCC is associated with shorter survival time and lower survival rate, it may be used as a novel indicator of prognosis in patients with HCC. The current study did not investigate the molecular mechanisms underlying this association; hence, the specific role of FOXO3 in the pathogenesis of HCC requires elucidation in future studies.
Acknowledgements
Not applicable.
Funding
This work was supported by the grants from the Zhejiang Province Bureau of Health (grant nos. WKJ-ZJ-1812, 2018ZZ002 and WKJ-ZJ-1710), National Science Foundation of China (grant nos. 81602174 and 81672430), Funds of Science Technology Department of Zhejiang Province (grant no. LGF18H160024 and LGF18H160025), Zhejiang Provincial Natural Science Foundation of China (grant no. LY17H160062).
Availability of data and materials
The microarray datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request. The dataset analyzed during the current study are available in the TGCA repository (https://portal.gdc.cancer.gov).
Authors' contributions
SSS and JFY performed the experiments and wrote the manuscript. XZM and XBD made substantial contributions to the conception of the study. YNZ and HYP participated in the design and coordination of experimental work and acquisition of data. XLH, HJW and ZMH participated in the study design, data collection and analysis of data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the Review Board of the Ethics Committee of Zhejiang Provincial People's Hospital (Hangzhou, China), and written informed consent was provided by each participant prior to data collection.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. J CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Liver Cancer Collaboration. Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C, Al-Raddadi R, Alvis-Guzman N, Amoako Y, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results From the global burden of disease study 2015. JAMA Oncol. 2017;3:1683–1691. doi: 10.1001/jamaoncol.2017.3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Comprehensive Cancer Network, corp-author. NCCN clinical practice guidelines in oncology (NCCN guidelines): Hepatobiliary cancers (version 2.2016) https://www.nccn.org/about/news/ebulletin/ebulletindetail.aspx?ebulletinid=1085. [Jun 27;2016 ];2016
- 4.Keating GM. Sorafenib: A review in hepatocellular carcinoma. Target Oncol. 2017;12:243–253. doi: 10.1007/s11523-017-0484-7. [DOI] [PubMed] [Google Scholar]
- 5.Samji H, Yu A, Kuo M, Alavi M, Woods R, Alvarez M, Dore GJ, Tyndall M, Krajden M, Janjua NZ, BC Hepatitis Testers Cohort Team Late hepatitis B and C diagnosis in relation to disease decompensation and hepatocellular carcinoma development. J Hepatol. 2017;67:909–917. doi: 10.1016/j.jhep.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 6.Ang C, O'Reilly EM, Abou-Alfa GK. Targeted agents and systemic therapy in hepatocellular carcinoma. Recent Results Cancer Res. 2013;190:225–246. doi: 10.1007/978-3-642-16037-0_15. [DOI] [PubMed] [Google Scholar]
- 7.Xue F, Liu Y, Chu H, Wen Y, Yan L, Tang Q, Xiao E, Zhang D, Zhang H. eIF5A2 is an alternative pathway for cell proliferation in cetuximab-treated epithelial hepatocellular carcinoma. Am J Transl Res. 2016;8:4670–4681. [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Ao X, Ding W, Ponnusamy M, Wu W, Hao X, Yu W, Wang Y, Li P, Wang J. Critical role of FOXO3a in carcinogenesis. Mol Cancer. 2018;17:104. doi: 10.1186/s12943-018-0856-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burgering BM. A brief introduction to FOXOlogy. Oncogene. 2008;27:2258–2262. doi: 10.1038/onc.2008.29. [DOI] [PubMed] [Google Scholar]
- 10.Wang PS, Chou CH, Lin CH, Yao YC, Cheng HC, Li HY, Chuang YC, Yang CN, Ger LP, Chen YC, et al. A novel long non-coding RNA linc-ZNF469-3 promotes lung metastasis through miR-574-5p-ZEB1 axis in triple negative breast cancer. Oncogene. 2018;37:4662–4678. doi: 10.1038/s41388-018-0293-1. [DOI] [PubMed] [Google Scholar]
- 11.Tikhanovich I, Cox J, Weinman SA. Forkhead box class O transcription factors in liver function and disease. J Gastroenterol Hepatol. 2013;28(Suppl 1):S125–S131. doi: 10.1111/jgh.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang K, Li L, Qi Y, Zhu X, Gan B, DePinho RA, Averitt T, Guo S. Hepatic suppression of Foxo1 and Foxo3 causes hypoglycemia and hyperlipidemia in mice. Endocrinology. 2012;153:631–646. doi: 10.1210/en.2011-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tao R, Wei D, Gao H, Liu Y, DePinho RA, Dong XC. Hepatic FoxOs regulate lipid metabolism via modulation of expression of the nicotinamide Phosphoribosyltransferase gene. J Biol Chem. 2011;286:14681–14690. doi: 10.1074/jbc.M110.201061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zanella F, Rosado A, García B, Carnero A, Link W. Chemical genetic analysis of FOXO nuclear-cytoplasmic shuttling by using image-based cell screening. Chem Biochem. 2008;9:2229–2237. doi: 10.1002/cbic.200800255. [DOI] [PubMed] [Google Scholar]
- 15.Anderson MJ, Viars CS, Czekay S, Cavenee WK, Arden KC. Cloning and characterization of three human forkhead genes that comprise an FKHR-like gene subfamily. Genomics. 1998;47:187–199. doi: 10.1006/geno.1997.5122. [DOI] [PubMed] [Google Scholar]
- 16.Birkenkamp KU, Coffer PJ. FOXO transcription factors as regulators of immune homeostasis: Molecules to die for? J Immunol. 2003;171:1623–1629. doi: 10.4049/jimmunol.171.4.1623. [DOI] [PubMed] [Google Scholar]
- 17.Burgering BM, Kops GJ. Cell cycle and death control: Long live Forkheads. Trends Biochem Sci. 2002;27:352–360. doi: 10.1016/S0968-0004(02)02113-8. [DOI] [PubMed] [Google Scholar]
- 18.Greer EL, Brunet A. FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene. 2005;24:7410–7425. doi: 10.1038/sj.onc.1209086. [DOI] [PubMed] [Google Scholar]
- 19.Hu MC, Lee DF, Xia W, Golfman LS, Ou-Yang F, Yang JY, Zou Y, Bao S, Hanada N, Saso H, et al. IkappaB kinase promotes tumorigenesis through inhibition of forkhead FOXO3a. Cell. 2004;117:225–237. doi: 10.1016/S0092-8674(04)00302-2. [DOI] [PubMed] [Google Scholar]
- 20.van der Vos KE, Gomez-Puerto C, Coffer PJ. Regulation of autophagy by Forkhead box (FOX) O transcription factors. Adv Biol Regul. 2012;52:122–136. doi: 10.1016/j.advenzreg.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Wang YQ, Cao Q, Wang F, Huang LY, Sang TT, Liu F, Chen SY. SIRT1 protects against oxidative stress-induced endothelial progenitor cells apoptosis by inhibiting FOXO3a via FOXO3a ubiquitination and degradation. Cell Physiol. 2015;230:2098–2107. doi: 10.1002/jcp.24938. [DOI] [PubMed] [Google Scholar]
- 22.Lu YF, Yu JR, Yang Z, Zhu GX, Gao P, Wang H, Chen SY, Zhang J, Liu MY, Niu Y, et al. Promoter hypomethylation mediated upregulation of MicroRNA-10b-3p targets FOXO3 to promote the progression of esophageal squamous cell carcinoma (ESCC) J Exp Clin Cancer Res. 2018;37:301. doi: 10.1186/s13046-018-0966-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bullock MD, Bruce A, Sreekumar R, Curtis N, Cheung T, Reading I, Primrose JN, Ottensmeier C, Packham GK, Thomas G, Mirnezami AH. FOXO3 expression during colorectal cancer progression: Biomarker potential reflects a tumour suppressor role. Br J Cancer. 2013;109:387–394. doi: 10.1038/bjc.2013.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rehman A, Kim Y, Kim H, Sim J, Ahn H, Chung MS, Shin SJ, Jang K. FOXO3a expression is associated with lymph node metastasis and poor disease-free survival in triple-negative breast cancer. J Clin Pathol. 2018;71:806–813. doi: 10.1136/jclinpath-2018-205052. [DOI] [PubMed] [Google Scholar]
- 25.Qian Z, Ren L, Wu D, Yang X, Zhou Z, Nie Q, Jiang G, Xue S, Weng W, Qiu Y, Lin Y. Overexpression of FoxO3a is associated with glioblastoma progression and predicts poor patient prognosis. Int J Cancer. 2017;140:2792–2804. doi: 10.1002/ijc.30690. [DOI] [PubMed] [Google Scholar]
- 26.Yu S, Yu Y, Sun Y, Wang X, Luo R, Zhao N, Zhang W, Li Q, Cui Y, Wang Y, et al. Activation of FOXO3a suggests good prognosis of patients with radically resected gastric cancer. Int J Clin Exp Pathol. 2015;8:2963–2970. [PMC free article] [PubMed] [Google Scholar]
- 27.Shi J, Zhang L, Shen A, Zhang J, Wang Y, Zhao Y, Zou L, Ke Q, He F, Wang P, et al. Clinical and biological significance of forkhead class box O 3a expression in glioma: Mediation of glioma malignancy by transcriptional regulation of p27kip1. J Neurooncol. 2010;98:57–69. doi: 10.1007/s11060-009-0045-8. [DOI] [PubMed] [Google Scholar]
- 28.Fei M, Zhao Y, Wang Y, Lu M, Cheng C, Huang X, Zhang D, Lu J, He S, Shen A. Low expression of Foxo3a is associated with poor prognosis in ovarian cancer patients. Cancer Invest. 2009;27:52–59. doi: 10.1080/07357900802146204. [DOI] [PubMed] [Google Scholar]
- 29.Beahrs OH, Henson DE, Hulter RVP, Meyers MH, editors. Manual for Staging of Cancer. JB Lippincott; Philadelphia, PA: 1988. Liver including intrahepatic bile ducts; pp. 87–92. [Google Scholar]
- 30.Izumi R, Shimizu K, li T, Yagi M, Matsui O, Nonomura A, Miyazaki I. Prognostic factors of hepatocellular carcinoma in patients undergoing hepatic resection. Gastroenterology. 1994;106:720–727. doi: 10.1016/0016-5085(94)90707-2. [DOI] [PubMed] [Google Scholar]
- 31.Edmondson HA, Steiner PE. Primary carcinoma of the liver: A study of 100 cases among 48,900 necropsies. Cancer. 1954;7:462–503. doi: 10.1002/1097-0142(195405)7:3<462::AID-CNCR2820070308>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 32.Zhou L, Rui JA, Zhou WX, Wang SB, Chen SG, Qu Q. Edmondson-Steiner grading: A crucial predictor of recurrence and survival in hepatocellular carcinoma without microvascular invasion. Pathol Res Pract. 2017;213:824–830. doi: 10.1016/j.prp.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 34.Toyoda H, Kumada T, Tada T. Changes in patient backgrounds may increase the incidence of HCC after SVR in the era of IFN-free therapy for HCV. Hepatology. 2016;64:1818–1819. doi: 10.1002/hep.28632. [DOI] [PubMed] [Google Scholar]
- 35.Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: Worldwide incidence and trends. Gastroenterology. 2004;127(Suppl 1):S5–S16. doi: 10.1053/j.gastro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 36.Galun D, Basaric D, Zuvela M, Bulajic P, Bogdanovic A, Bidzic N, Milicevic M. Hepatocellular carcinoma: From clinical practice to evidence-based treatment protocols. World J Hepatol. 2015;7:2274–2291. doi: 10.4254/wjh.v7.i20.2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.He TC, Zhou S, da Costa LT, Yu J, Kinzler KW, Vogelstein B. A simplified system for generating recombinant adenoviruses. Proc Natl Acad Sci USA. 1998;95:2509–2514. doi: 10.1073/pnas.95.5.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9:28–39. doi: 10.1038/nrc2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hojjat-Farsangi M. Small-molecule inhibitors of the receptor tyrosine kinases: Promising tools for targeted cancer therapies. Int J Mol Sci. 2014;15:13768–13801. doi: 10.3390/ijms150813768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verweij J, Casali PG, Zalcberg J, LeCesne A, Reichardt P, Blay JY, Issels R, van Oosterom A, Hogendoorn PC, Van Glabbeke M, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: Randomized trial. Lancet. 2004;364:1127–1134. doi: 10.1016/S0140-6736(04)17098-0. [DOI] [PubMed] [Google Scholar]
- 41.Rimassa L, Danesi R, Pressiani T, Merle P. Management of adverse events associated with tyrosine kinase inhibitors: Improving outcomes for patients with hepatocellular carcinoma. Cancer Treat Rev. 2019;77:20–28. doi: 10.1016/j.ctrv.2019.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Tsai KL, Sun YJ, Huang CY, Yang JY, Huang MC, Hsiao CD. Crystal structure of the human FOXO3a-DBD/DNA complex suggests the effects post-translational modification. Nucleic Acids Res. 2007;35:6984–6994. doi: 10.1093/nar/gkm703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zou Y, Tsai WB, Cheng CJ, Hsu C, Chung YM, Li PC, Lin SH, Hu MC. Forkhead box transcription factor FOXO3a suppresses estrogen-dependent breast cancer cell proliferation and tumorigenesis. Breast Cancer Res. 2008;10:R21. doi: 10.1186/bcr1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang F, Marshall CB, Yamamoto K, Li GY, Plevin MJ, You H, Mak TW, Ikura M. Biochemical and structural characterization of an intramolecular interaction in FOXO3a and its binding with p53. J Mol Biol. 2008;384:590–603. doi: 10.1016/j.jmb.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 45.Luo J, Liang A, Liang M, Xia R, Rizvi Y, Wang Y, Cheng J. Serum glucocorticoid-regulated kinase 1 blocks CKD-induced muscle wasting via inactivation of FOXO3a and Smad2/3. J Am Soc Nephrol. 2016;27:2797–2808. doi: 10.1681/ASN.2015080867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu J, Zhang R, Hong H, Yang Z, Sun D, Sun S, Guo X, Ye J, Li Z, Liu P. The poly(ADP-ribosyl) ation of FOXO3 mediated by PA R P1 participates in isoproterenol-induced cardiac hypertrophy. J Biochim Biophys Acta. 2016;1863:3027–3039. doi: 10.1016/j.bbamcr.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 47.Sanchez AM, Csibi A, Raibon A, Cornille K, Gay S, Bernardi H, Candau R. AMPK promotes skeletal muscle autophagy through activation of forkhead FOXO3a and interaction with UIK2. J Cell Biochem. 2012;113:695–710. doi: 10.1002/jcb.23399. [DOI] [PubMed] [Google Scholar]
- 48.van Grevenynghe J, Cubas RA, DaFonseca S, Metcalf T, Tremblay CL, Trautmann L, Sekaly RP, Schatzle J, Haddad EK. Foxo3a: An integrator of immune dysfunction during HIV infection. Cytokine Growth Factor Rev. 2012;23:215–221. doi: 10.1016/j.cytogfr.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ikeda J, Tian T, Wang Y, Hori Y, Honma K, Wada N, Morii E. Expression of FoxO3a in clinical cases of malignant lymphoma. Pathol Res Pract. 2013;209:716–720. doi: 10.1016/j.prp.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 50.Shou Z, Lin L, Liang J, Li JL, Chen HY. Expression and prognosis of FOXO3a and HIF-1α in nasopharyngeal carcinoma. J Cancer Res Clin Oncol. 2012;138:585–593. doi: 10.1007/s00432-011-1125-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu M, Xiang J, Xu F, Wang Y, Yin Y, Chen D. The expression and significance of pThr32-FOXO3a in human ovarian cancer. Med Oncol. 2012;29:1258–1264. doi: 10.1007/s12032-011-9919-7. [DOI] [PubMed] [Google Scholar]
- 52.Stan SD, Hahm ER, Warin R, Singh SV. Withaferin A causes FOXO3a- and Bim-dependent apoptosis and inhibits growth of human breast cancer cells in vivo. Cancer Res. 2008;68:7661–7669. doi: 10.1158/0008-5472.CAN-08-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim HJ, Lee SY, Kim CY, Kim YH, Ju W, Kim SC. Subcellular localization of FOXO3a as a potential biomarker of response to combined treatment with inhibitors of PI3K and autophagy in PIK3CA-mutant cancer cells. Oncotarget. 2017;8:6608–6622. doi: 10.18632/oncotarget.14245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eijkelenboom A, Burgering BM. FOXOs: Signaling integrators for homeostasis maintenance. Nat Rev Mol Cell Biol. 2013;14:83–97. doi: 10.1038/nrm3507. [DOI] [PubMed] [Google Scholar]
- 55.Jia Q, Bu Y, Wang Z, Chen B, Zhang Q, Yu S, Liu Q. Maintenance of stemness is associated with the interation of LRP6 and heparin-binding protein CCN2 autocrined by hepatocellular carcinoma. J Exp Clin Cancer Res. 2017;36:117. doi: 10.1186/s13046-017-0576-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.You H, Yamamoto K, Mak TW. Regulation of transactivation-independent proapoptotic activity of p53 by FOXO3a. Proc Natl Acad Sci USA. 2006;103:9051–9056. doi: 10.1073/pnas.0600889103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kloet DE, Burgering BM. The PKB/FOXO switch in aging and cancer. Biochim Biophys Acta. 2011;1813:1926–1937. doi: 10.1016/j.bbamcr.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Hoogeboom D, Burgering BM. Should I stay or should I go: Beta-catenin decides under stress. Biochim Biophys Acta. 2009;1796:63–74. doi: 10.1016/j.bbcan.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 59.Essers MA, de Vries-Smits LM, Barker N, Polderman PE, Burgering BM, Korswagen HC. Functional interaction between beta-catenin and FOXO in oxidative stress signaling. Science. 2005;308:1181–1184. doi: 10.1126/science.1109083. [DOI] [PubMed] [Google Scholar]
- 60.Lasagna N, Fantappiè O, Solazzo M, Morbidelli L, Marchetti S, Cipriani G, Ziche M, Mazzanti R. Hepatocyte growth factor and inducible nitric oxide synthase are involved in multidrug resistance-induced angiogenesis in hepatocellular carcinoma cell lines. Cancer Res. 2006;66:2673–2682. doi: 10.1158/0008-5472.CAN-05-2290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The microarray datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request. The dataset analyzed during the current study are available in the TGCA repository (https://portal.gdc.cancer.gov).