Abstract
Background:
The process of returning to work after cartilage treatment has not been studied in depth, even though a better understanding of potential outcomes could lead to significant benefits for the general population.
Purpose:
To determine which surgical interventions are most effective in helping patients return to work after cartilage repair and to identify factors that affect the ability to return to work.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
This systematic review followed PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines in analyzing reports on articular cartilage treatment and return to work published from January 1966 (when the first system of classifying articular cartilage injuries based on the mechanism of injuries and type of lesions was developed) to January 2019. General surgical information and available clinical scores were used to assess outcomes.
Results:
Only 5 studies describing 283 patients were found to be relevant to our objectives and were therefore included in the analysis. Autologous chondrocyte implantation (ACI) and osteochondral allografts were the only 2 procedures for which information was included regarding patient return to work rates. The mean (overall) return-to-work time after a cartilage repair operation was 4.80 ± 3.02 months. ACI was the most common procedure (3 studies; 227 patients). Return to work after ACI or ACI with high tibial osteotomy (HTO) occurred in almost 100% of cases, whereas the rate of return to work was 51.78% for patients who underwent osteochondral allograft (P < .01); further, patients who had ACI or ACI+HTO returned to work sooner compared with patients who underwent osteochondral allograft. The Knee injury and Osteoarthritis Outcome Score (KOOS) and Single Assessment Numerical Evaluation (SANE) scores were significantly higher in patients who fully returned to work. No significant difference was found in rates of return to work after ACI related to sex, area of the lesion, or size of the defect.
Conclusion:
The vast majority of published results on articular cartilage repair do not include data on return to work. Although available data on articular cartilage repair in the general population reveal a high rate of return to work, including those patients treated with ACI, the data do not stratify patients by the type and demand of work. No randomized studies have examined return-to-work rates. Hence, authors should include these data in future studies. A refined definition of work intensity, rather than just return to work, may provide a clearer picture of the relative effectiveness of different surgical interventions. To that end, the authors propose a return to work prognostic score called the Prognostic Cartilage Repair Return to Work Score, or PROCART-RTW score.
Keywords: cartilage, injury, repair, return to work, autologous chondrocyte implantation, high tibial osteotomy, allograft, PROCART-RTW score
Articular cartilage injuries are among the most common injuries in the knee and can be observed in all age groups.3,4 Cartilage has low self-repair capacity due to the lack of a blood supply.5 As a result, injured cartilage may progress to a full degeneration.8 In 1966, articular cartilage injuries were classified into 3 main categories by O’Donoghue.23 A number of strategies have been developed to deal with this problem, including palliative, reparative, and restorative interventions. However, the morbidity resulting from an injury may remain even after treatment interventions and may force patients to adapt their lifestyle, including reduction of daily life activities. Because many people are now living a more active lifestyle, including increased participation in sports at both recreational and competitive levels, interest in studying return to work and return to sports after articular cartilage repair has increased. Several studies, including systematic reviews, have shown that return to participation in sports by athletes is possible after articular cartilage repair intervention.6,9,19–22 Surgical interventions, such as microfracture, osteochondral autograft transplant (OAT), osteochondral allograft transplant, and autologous chondrocyte implantation (ACI), have been shown to improve knee pain and functional scores in athletes.6,7,14,22 The time to return to sports after cartilage repair has been widely studied. The mean period before return to sports after various procedures has been reported to be in the range of 7.1 to 16 months.6 The time to return to sports in athletes is shortest in patients undergoing OAT, followed by microfracture, allograft, and ACI.6 A better prognosis after surgery has been observed in patients with small defects, younger age, a short preoperative period, no previous surgical interventions, and strict adherence to rehabilitation measures.6
However, because people generally spend more time working than they do participating in sports activities, the return-to-work period is an important consideration. Based on available data, it appears that studying return to work has been of much less interest even though it may potentially lead to great benefits for a large segment of the general population. To that end, it is crucial that surgical outcomes be assessed in order to optimize the return-to-work capacity.
This study aimed to determine which surgical interventions are most effective in helping patients return to work and to identify specific factors that significantly affect the ability to return to work.
Methods
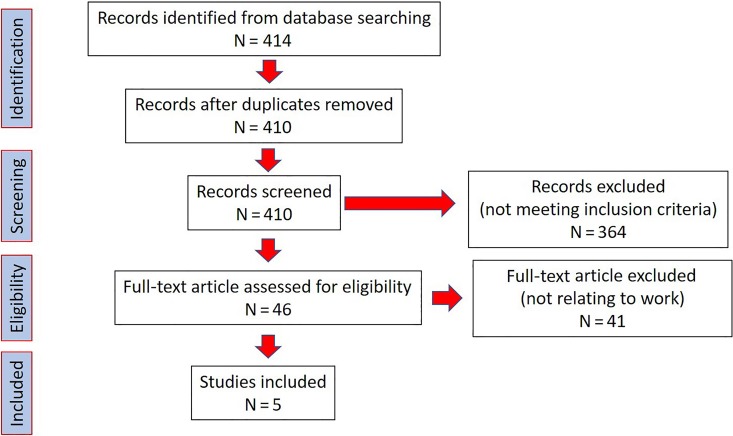
A search for relevant medical databases for articular cartilage treatment and return to work in the English language was conducted during the period from January 1966, when articular cartilage injuries were first classified into 3 main categories by O’Donoghue23 based on the mechanism of injuries and type of lesions, to January 2019. The medical databases were searched using MEDLINE/PubMed with the terms knee defect, knee lesion, articular cartilage repair, return, sick, leave, absenteeism, rest, work, job, activity, debridement, microfracture, marrow stimulation, chondroplasty, abrasive, osteochondral allograft, osteochondral autograft, tibial osteotomy, femoral osteotomy, autologous chondrocyte implantation, stem cells, and articular cartilage repair. Searches were performed in other databases, including EMBASE, and we reviewed articles related to articular cartilage injury and repair among scientific meeting abstracts. All studies that included clinical results and concomitant information on articular cartilage repair were reviewed. Studies reviewed include those that described work- or activity-related functional outcomes; the ability to return to work after articular cartilage treatment received special attention. This systematic review of the literature was performed following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart outlining the systematic review algorithm. After application of all inclusion and exclusion parameters, 5 studies were identified for review.
Initially, only limited information was found in the medical databases, so all of the medical databases were analyzed further in a secondary review. Because cartilage injuries are often associated with other injuries, studies with concomitant operative procedures due to associated injuries were also accepted. Two studies that combined 2 procedures were included because these were the only allograft studies describing return to work.30,31 All studies included had at least 24 months of follow-up. Finally, 5 studies were found to be relevant to our research objectives.1,17,24,30,31
Data from each of the studies, including design, characteristics, level of evidence, and surgical information (eg, patient demographics, lesion characteristics, operation technique, concomitant procedures, and follow-up data), were systematically analyzed. Information describing levels of work activity (eg, activity scores such as time to return to work and level of work activity) was collected. Scores used in studies, such as the Tegner activity scale, Lysholm-Gillquist score, modified Cincinnati Knee Rating System, Knee injury and Osteoarthritis Outcome Score (KOOS), and International Knee Documentation Committee score, were included as measurements of outcomes.
Statistical analysis was performed through use of Stata Version 15 (Stata Corp). Data are presented as mean and standard error of the mean (SEM). Statistical significance was set at P ≤ .05.
Results
The analysis included 5 studies describing 283 patients (Table 1).1,17,24,30,31 All included studies were conducted after the year 2000. ACI and osteochondral allograft were the only 2 procedures that included reports of the return-to-work rate. Interestingly, we found no reports on microfracture even though it is one of the most common restorative procedures. The overall mean patient age in the studies was 33.78 ± 8.17 years, and the mean follow-up was 59.05 ± 23.91 months. Most studies included isolated defects with a mean defect size of 4.53 ± 0.43 cm2. Defect size was largest in patients undergoing cartilage repair with osteochondral allograft transplant (mean, 4.9 cm2) followed by ACI with high tibial osteotomy (HTO) (mean, 4.6 cm2) and ACI (mean, 4.4 cm2) (Table 2). Most lesions were located in the medial femoral condyle (Table 3).
Table 1.
Pooled Study Demographicsa
| Demographic Parameter | Value |
|---|---|
| No. of patients | 283 |
| Age, y, mean ± SEM | 33.78 ± 8.17 |
| Sex, % | |
| Male | 70.37 |
| Female | 29.63 |
| Follow-up, mo, mean ± SEM | 59.05 ± 23.91 |
| Lesion location, % | |
| Femoral condyle | 71.06 |
| Trochlear groove | 5.11 |
| Patella | 23.83 |
| Defect size, cm2, mean ± SEM | 4.53 ± 0.43 |
| Body mass index, mean ± SEM | 25.06 ± 2.69 |
aNo data were available on type of work or severity of lesions.
Table 2.
Patient Activity After Cartilage Repair Interventiona
| Lead Author (Year) | Intervention | No. of Patients | Follow-up, mob | Outcome Measure | Return to Work, moc | Type of Work | Results |
|---|---|---|---|---|---|---|---|
| Lindahl17 (2001) | ACI | 57 | 60 (24-120) | Modified Cincinnati | NRd | General | Mean days absent per year decreased from 155 to 1.5 after ACI. More than 80% of patients presented good/excellent clinical rating. |
| Bode1 (2015) | ACI + HTO | 40 | 60.5 ± 2.5 | Lysholm, VAS, KOOS | 3.15 ± 2.58 | General | Return to work depended on the workload. |
| Pestka24 (2016) | ACI | 130 | 63.6 ± 27.6 | Tegner | 3.4 ± 2.75 | General | Return to work did not appear to be influenced by patient age. Significant differences were found depending on work intensity according to the REFA score (grades 1-4). |
| Shaha31 (2013) | Osteochondral allograft | 38 | 49.2 (7.2-106.8) | KOOS, SANE | 12.1 ± 9 | General and military | Only 11 patients were able to return to full duty. |
| Scully30 (2011) | Osteochondral allograft | 18 | 40.8 ± 23.76 | Descriptive data | 23.2 | General and military | 7 of 18 patients returned to work. Only 1 patient returned to his or her previous job. The others returned to work, doing limited activity. |
aNo studies indicated the return to work outcome after other cartilage repair interventions (eg, microfracture, osteochondral autograft, stem cell therapy). ACI, autologous chondrocyte implantation; HTO, high tibial osteotomy; KOOS, Knee injury and Osteoarthritis Outcome Score; Lysholm, Lysholm-Gillquist score; NR, not reported; REFA, REFA Association; SANE, Single Assessment Numeric Evaluation; VAS, visual analog scale.
bValues are expressed as mean ± SEM or mean (range).
cValues are expressed as mean or mean ± SEM.
dSee the Results section for more information.
Table 3.
Analysis of Return to Work Classified by Cartilage Repair Intervention (ACI vs Non-ACI)a
| Studies | No. of Patients | Intervention | Type of Work, % of Patients | Return to Work, mob | % of Return | Medial Femoral Condyle, % | Lateral Femoral Condyle, % |
|---|---|---|---|---|---|---|---|
| ACI studies | |||||||
| Lindahl17 (2001) | 57 | ACI | NR | NR | 100 | 66.67 (OCD 14.03, patella 19.3)c | |
| Bode1 (2015) | 40 | ACI + HTO | Mild-moderate: 64.2 | 2.27 ± 2.04 | 100 | 100 | 0 |
| Hard-heavy: 35.8 | 5.16 ± 3.7 | 100 | |||||
| Pestka24 (2016) | 130 | ACI | Mild-moderate: 76.9 | 2.61 ± 2.28 | 100 | 44.61 | 55.39 |
| Hard-heavy: 23.1 | 4.81 ± 3.26 | 96 | |||||
| Non-ACI studies | |||||||
| Shaha31 (2013) | 38 | Osteochondral allograft | Mild-moderate: 26.3 | 12.1 ± 9 | 67.8 | 65.78 | 34.22 |
| Hard-heavy: 73.7 | 30 | ||||||
| Scully30 (2011) | 18 | Osteochondral allograft | Mild-moderate: 33.3 | 23.2 | 100 | 83.33 | 16.67 |
| Hard-heavy: 66.7 | 8.3 | ||||||
aACI, autologous chondrocyte implantation; HTO, high tibial osteotomy; NR, not reported; OCD, osteochondritis dissecans.
bValues are expressed as mean or mean ± SEM.
cNo information provided regarding medial or lateral side; 8 (14.03%) lesions were OCD and 11 (19.3%) lesions were patellar.
The ACI procedure was the most common intervention (3 studies; 227 patients).1,17,24 We found that 2 studies used second-generation ACI with a collagen type I/III cover, whereas 1 study used first-generation ACI with periosteum cover. The 2 studies with osteochondral allograft reported the use of fresh-stored allograft. Concomitant procedures were performed in 4 studies with 63 patients including osteotomy,1,30,31 anterior cruciate ligament repair or reconstruction,17,31 meniscal debridement,30 meniscal allografts, or implant removal.31
Functional Outcomes
The overall mean time to return to work, calculated from data available in 4 studies, averaged 4.80 ± 3.02 months after a cartilage repair operation.1,24,30,31 Most of the patients were able to tolerate moderate to heavy physical strain, including military duties (Table 3).
The mean time to return to work after ACI was 3.34 months, whereas return to work after ACI with HTO at 3.15 months was slightly shorter than with ACI alone. The mean time to return to work for full duty after osteochondral allograft was 12.1 ± 6.9 months, significantly longer than for ACI and HTO (P < .05).
Almost 100% of patients returned to work after ACI or ACI with HTO; however, only 51.78% of those who underwent osteochondral allograft returned to their former work activity (P < .01). It is important to note that those studies included active duty military personnel with very high–demand activity. No statistically significant difference was found in time to return to work between ACI alone and ACI with HTO (P > .05). We found that 2 studies included information on work intensity after return to work.1,24 The rate of return to preinjury work level was 90.8% in patients who had undergone ACI, significantly higher than the 21.42% for those with a high-demand military work receiving an osteochondral allograft (P < .05).
Outcome Scoring
Regarding evaluation of knee function in daily life after ACI, alternative scoring systems have provided differing clinical outcomes. Measurements using the modified Cincinnati Knee Rating System have shown good to excellent outcomes in 85.96% of patients. However, evaluations using the Tegner activity level scale have shown a significant decrease after ACI (3.4 ± 1.8 postoperatively vs 4.3 ± 2.7 1 year before surgery). Visual analog scale (VAS) pain scores were significantly improved after ACI with HTO, increasing from 6.7 ± 1.9 before surgery to 2.2 ± 1.4 after surgery (P = .00). Mean Lysholm scores increased by 22 points from 54.4 ± 18.9 to 76.2 ± 19.8 points after ACI with HTO. The postoperative KOOS subscale score for activities of daily living was 87.6 ± 16.2, and that for knee-related quality of living was 55.5 ± 22.0. The calculated total KOOS score was 71.2 ± 16.1 points. KOOS and Single Assessment Numeric Evaluation scores were significantly higher in patients with full return to work (340.88 ± 64.03 and 79.38 ± 10.50, respectively) after osteochondral allograft intervention compared with patients unable to return to full duty (192.00 ± 49.93 and 41.25 ± 20.31, respectively; P < .05).
Patient-Specific Factors
Work Intensity
Time to return to work was strongly associated with the physical workload in each occupation. In 1 study, patients performing job-related activities involving small to moderate physical strain returned to work significantly sooner after ACI surgery than did patients whose jobs involved the greatest physical strain (2.8 ± 2.45 vs 5.15 ± 3.5 months, respectively; P = .0038).24 In another study, patients with jobs that involved low physical strain who underwent ACI and HTO returned to work significantly sooner than patients whose jobs involved heavy physical strain (2.27 ± 2.04 vs 5.16 ± 3.7 months, respectively; P = .023).1 The mean duration of sick leave after ACI was approximately 1.5 days per year (range, 0-58 days) compared with 155 days per year before surgery.17,24 A study of osteochondral allograft transplant among military personnel reported that time to return to work was associated with the specific branch of service. The time to return to work was longer for individuals in the Marines and Navy than for those in other branches (P < .05) of the armed forces.31
Age
The mean time to return to work after ACI was not significantly correlated with patient age. In 1 study, patients younger than 30 years of age took 2.7 ± 1.17 months to return to work, whereas patients aged 30 to 45 years and those older than 45 years of age returned to work after 3.72 ± 2.975 and 3.5 months, respectively.24 Similarly, no significant association was found between age and time to return to work after osteochondral allograft. None of the reports included in this review provided age data for both ACI and HTO patients.
Other Factors
In 1 study, no significant differences were found in time to return to work after ACI related to the area of lesion, the defect size, or the sex of the patient.24 No data were available to compare return-to-work rates between first- and second-generation ACI; however, both first- and second-generation ACI studies showed good clinical outcomes. Concomitant HTO and ACI procedures did not alter time to return to work. Another study reported that there was no difference in return-to-work outcome after osteochondral allograft related to the area of the lesion, the size of the lesion (552.3 mm2 for return to full duty vs 472.6 mm2 for return to limited duty and 488.9 mm2 for no return to duty), number of osteochondral plugs, concomitant procedures, or prior surgical interventions.31 However, an association was found between a patient’s weight and his or her return-to-work status. The mean body mass index (BMI) for return to full duty was 26.0, compared with 27.9 for return to limited duty and 28.7 for no return to duty, but the difference was not statistically significant.31 No other related factors were mentioned in the studies of ACI with HTO, and there was no mention of prior procedures in relation to the return-to-work outcome.
Discussion
Returning to work is a crucial step in recovering from injury, and it means that individuals can return to a normal life, often reducing the injury’s social, financial, and emotional impact on both the patient and their families. Returning to work may mean that individuals have gone back to their previous post, have taken another position, or are working reduced hours or modified duties.
Articular cartilage injuries occur frequently and can have a significant impact on not only the individual but also society. Several surgical methods are available to treat these injuries, all of which result in satisfactory outcomes. It appears that reporting the return-to-work capacity may lead to great benefits for a large segment of the general population, for example, by helping both surgeons and patients understand realistic effects of the planned procedure, suggesting pre- and postoperative rehabilitation processes, and indicating when to operate and which actions should be taken before and after surgery. To that end, it is crucial that surgical outcomes be assessed to optimize the patient’s capacity to return to activity.
Several clinical outcome studies on return to previous activities have been conducted, mostly regarding return to sports. The mean reported time to return to sports varies from 7.1 months to 16 months depending on the procedure as well as the severity of the injury.6 Studies of return to sports in athletes usually present data uniquely related to competitions and challenges. These data are specific to the greater biomechanics and excessive movement demands seen in athletes and may differ from those in the general nonsporting population. However, data are lacking regarding time to return to work in the general population; in particular, there are no randomized studies examining return-to-work rates, an area that could be considered to have wide importance. Despite our exhaustive literature search, we found only 5 studies that addressed return to work after articular cartilage surgery.
The primary approach in this study was to review the literature to evaluate the relationship between surgical intervention in cartilage treatment and return to work after articular cartilage injury. Surprisingly, although microfracture is one of the most frequently used interventions for articular cartilage treatment of knees, no studies were available showing return to work after this surgery in the general population. However, we found many studies of microfracture that reported on return to sports, including clinical score, failure rate, and osteoarthritis progression. No definitive conclusions can be made given the few studies available and the heterogeneity of these studies.
Some studies indicated that patients who undergo microfracture are less likely to return to sport than athletes who undergo ACI or OAT.6,10,15 The rate of return to sports for athletes was reported to be 66%, with a mean time to return after microfracture of 8 months,20 which is much higher than the mean time to return to work found in the current review. Several studies found various factors to be involved in return to sports after microfracture. One factor is age, which can affect metabolic activity, repair, and synthesis in cartilage. Other factors include the duration of symptoms, lesion characteristics, overall recovery period, delay before surgery, and socioeconomic lifestyle adaptation.20,21 These factors could be more closely examined in future studies of return to work after microfracture surgery in the general population.
Only 3 studies reported data on return to work after ACI1,17,24 in the general population in contrast to the relatively large number of studies on return to sports after ACI.19,28 The present review found that the surgical techniques of first- and second-generation ACI provide similar results in return to work. Return to work after surgical intervention with ACI is faster than return to sport (3.34 ± 2.75 vs 18 ± 4 months, respectively).19 The mean return to work period in this review appeared closely correlated with age and work intensity; that is, younger patients (<30 years) returned to work sooner than older patients (≥30 years). The good recovery in the younger age group in the general population is in agreement with findings on return to sports.19 The difference between age groups may possibly be explained by the number of comorbidities, which tend to increase with age. In addition, patients undergoing ACI tend to have a more active lifestyle,12 so their expectations may be a factor in their more rapid recovery. The ability to return to work is also associated with clinical function scoring. A significantly high percentage of good and excellent scores on the modified Cincinnati Knee Rating System is an indication of good long-term functional improvement in the general population,25,26 similar to the results for return to sports.22
HTO is used to correct concomitant malalignment to optimize the biomechanical environment for the healing site in cartilage repair intervention, including in ACI.2,11 This review found that the return-to-work rate after ACI with HTO was not significantly different compared with the rate for ACI alone. The approximate time to return to work was also similar to the 2.9 months with HTO alone.29 Functional outcomes show that patients experience good recovery as evidenced by improvement of VAS scores, significant increase of knee function as measured by the Lysholm score, and good to excellent results on the KOOS. These outcomes may indicate that the combination of alignment correction and cartilage repair neither increases nor reduces the capacity to return to work. However, future research should ascertain whether different HTO techniques result in different return-to-work outcomes.
Data on osteochondral allografts showed a significantly longer time to return to work compared with the mean for all cartilage repair interventions. The time to return to work after allograft was also longer than that for return to sports (12.1 ± 6.9 vs 9.6 ± 3 months, respectively).16,31 However, it is important to note that the original study of osteochondral allografts was conducted in a military population.30,31 The greater intensity of effort and more extreme physical activity among members of the military may contribute to the longer recovery period. The outcomes reported in studies of military servicemembers also showed a great variation in ability to return to work; rates of return to preinjury work were between 5.56% and 29%.30,31 This implies that outcomes may be different for patients who perform dissimilar military duties or in studies of less physically demanding occupations. No studies were available on return to work after OAT in the general population; however, studies of return to sports showed that the mean recovery period with OAT is shorter than with other surgical interventions, including osteochondral allograft transplant.6 It might be interesting to investigate the relation between OAT and return to work.
The secondary approach in this study was to review the literature to evaluate the relationship between work intensity and return to work. Work intensity is negatively correlated with return to work. A high physical workload is assumed to be a detrimental factor for recovery. This is in line with the results of studies on return to sports where high-level competitive athletes have a lower return rate compared with recreational athletes.6 Studies on return to sport mostly present the relationship between outcomes for different levels of competition or for a specific type of sport. Future studies could expand on this and develop a system for making prognostic judgments regarding return to work after cartilage repair by relatively predicting the outcome based on physical work intensity, somatic status, and lesion type. Some return-to-work studies report on the relationship of outcomes to specific work intensity categories. For example, the REFA classification (from the REFA Association in Germany) categorizes outcomes in relation to work intensity.24 Several classification systems have been adapted for use in prediction of return to work after other orthopaedic procedures, for example, the DOT classification system (from the Dictionary of Occupational Titles), which is used in arthroplasty studies.18 However, those classifications focus primarily on weight-carrying or exertion and movement in the vertical plane, but they include only minimal objective definitions. As a result, the use of these classifications may be limited to only some subpopulations. A more generally applicable classification system, which includes categories for horizontal plane movement, frequency of work activity, and objective parameters, is needed for use with the general population.
Time to return to work may not rely solely on the patient’s physical factors but may entail multiple other confounding factors. Outcomes are believed to depend on several specific factors including patient compliance with rehabilitation protocols, where strict compliance is one of the keys to successful recovery. The level of patient compliance is individual and may be affected by several factors including concomitant injuries as well as psychological and social factors. Several studies have shown that the expense of cartilage treatment to the patient involves not only the direct cost of the operation but also indirect costs such as expenses related to visiting the patient and purchase of medication.17,32 A quicker return to work can minimize those indirect costs. Additionally, there are several areas in which the general population and athletes may differ after surgery. Follow-up in the general population may be less frequent than with athletes, the latter normally having a special medical team to closely monitor their progress. In addition, athletes’ contracts can include clauses that link remuneration to participation, which would tend to motivate faster return to active play. These sport-related factors contrast with the standard provisions in employment contracts regarding paid sick leave and absenteeism after surgery in the general population. An extended paid sick leave period may actually increase the time to recovery, especially if the sick leave compensation is generous. All these factors should be taken into consideration when researching time to return to work.
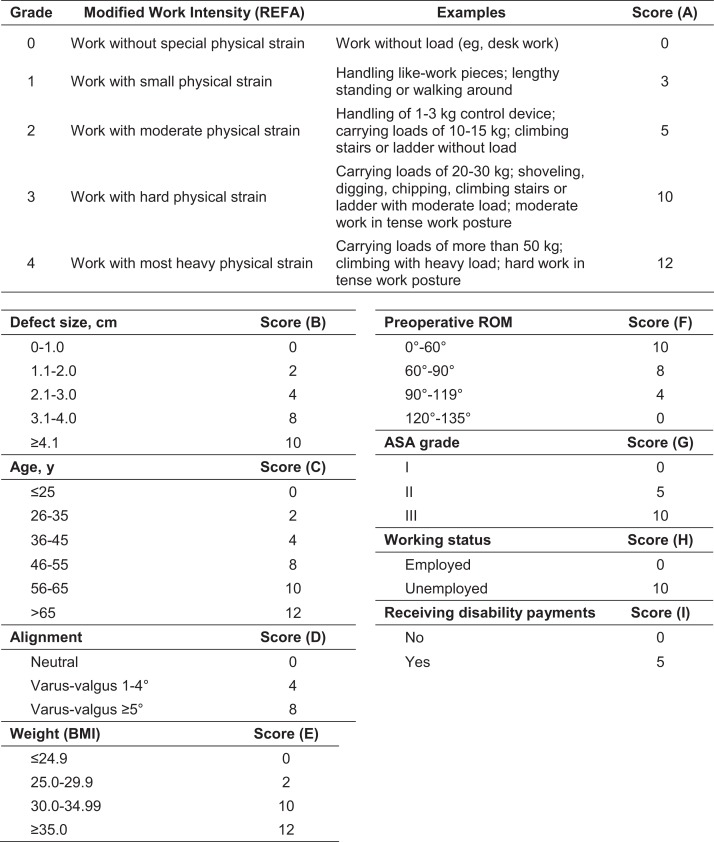
One area in particular, research on outcomes of cartilage repair, would benefit from attention to time to return to work. To predict the time to recovery after cartilage repair, a scoring system should be adopted that includes several critical items of information, for example, details of work intensity related to job-specific classifications, lesion characteristics, and patient demographics (eg, age, BMI, alignment of the knee, and preoperative range of motion). In addition, whether the patient is authorized to receive sick leave compensation needs to be included as one of the factors. To that end, we have prepared a return-to-work prognostic scoring system, the Prognostic Cartilage Repair Return to Work (PROCART-RTW) score (Figure 2). This scoring system is intended to be a first draft that includes a summary score of somatic, psychological, and work type–related factors that could potentially affect time to return to work. The draft scoring system also includes factors known to be related to healing potential after surgery, including obesity (BMI),13 level of physical effort or intensity of work,33 and initial defect size.27
Figure 2.
Prognostic Cartilage Repair Return to Work (PROCART-RTW) score. Total prognostic score = A + B + C + D + E + F + G + H + I; 0 = the best prognosis, 89 = the worst prognosis. ASA, American Society of Anesthesiologists classification; BMI, body mass index; REFA, REFA Association (Reichsausschuβ für Arbeitszeitermittlung [Reich Committee for Working Time Determination]); ROM, range of motion.
This proposed scoring system is based on work intensity grading as delineated by REFA scores20 and includes additional patient demographics. The scoring ranges from 0 to 89; the minimum score of 0 indicates the highest chance of returning to work whereas the maximum score of 89 indicates the lowest chance of returning to work after cartilage repair. This scoring system is suggested as a tool for clinicians to use in patient selection, choice of intervention, and prediction of postoperative recovery. The scoring system could also provide patients with additional information regarding what to expect after a cartilage repair.
This review has several limitations. The first is the limited number of studies on return to work and hence the relatively small number of patients for whom information is available. Second, there are no studies of return to work after alternative interventions (eg, microfracture), where outcomes could be quite different. Third, insufficient information is available to adequately assess some specific aspects (eg, postoperative complications after return to work), which could be important for treatment planning. Fourth, the populations in some of the studies included in this review are unique, such as the study of military personnel, whose activity profile could be quite different from that of the general population. Fifth, no randomized studies have examined return to sport or return to work. Cultural differences influence return to work, and the amount of workers’ compensation varies among countries. Subsequently, it is important that all future cartilage repair studies report on the return to work. Randomization might be more difficult to perform, but today’s registries could document work disability and return to work.
Our proposed return-to-work score, which needs to be validated, is a suggestion to help both surgeons and patients understand realistic effects of the planned procedure. The score can be used to start preoperative rehabilitation processes, determine when to operate, and identify actions that should be taken before and after surgery.
Conclusion
The vast majority of published results on cartilage repair do not include data on return to work; the few studies that do include such data do not stratify the patients by type or demand of work. Available studies show that individuals are often able to work at their preinjury level after ACI and ACI with HTO, but they are less likely to be able to do so after treatment of large lesions with osteochondral allografts. Because few comparative studies are available, further randomized studies are needed to improve our understanding of time to return to work and capacity to work after various surgical procedures, such as microfracture and OAT. A scoring system such as the PROCART-RTW that can predict probable surgical outcomes could potentially assist both clinicians and patients in the evaluation of treatment options.
Acknowledgment
We are most grateful for Chaisiri Angurawaranon, MD, PhD, and Areerak Phanphaisarn, RN, for statistical support and G. Lamar Robert, PhD, for manuscript editing support.
Footnotes
Final revision submitted November 8, 2019; accepted November 25, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand, and the University of Gothenburg, Gothenburg, Sweden. M.B. has served on the Medical Advisory Board for Episurf Medical and has received speaking fees from Anika, research support from Vericel, and publishing royalties from Elsevier and Studentlitteratur. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Bode G, Ogon P, Pestka J, et al. Clinical outcome and return to work following single-stage combined autologous chondrocyte implantation and high tibial osteotomy. Int Orthop. 2015;39(4):689–696. [DOI] [PubMed] [Google Scholar]
- 2. Bode G, Schmal H, Pestka JM, Ogon P, Sudkamp NP, Niemeyer P. A non-randomized controlled clinical trial on autologous chondrocyte implantation (ACI) in cartilage defects of the medial femoral condyle with or without high tibial osteotomy in patients with varus deformity of less than 5 degrees. Arch Orthop Trauma Surg. 2013;133(1):43–49. [DOI] [PubMed] [Google Scholar]
- 3. Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(suppl 2):58–69. [DOI] [PubMed] [Google Scholar]
- 4. Buckwalter JA. Articular cartilage: injuries and potential for healing. J Orthop Sports Phys Ther. 1998;28(4):192–202. [DOI] [PubMed] [Google Scholar]
- 5. Buckwalter JA, Lane NE. Athletics and osteoarthritis. Am J Sports Med. 1997;25(6):873–881. [DOI] [PubMed] [Google Scholar]
- 6. Campbell AB, Pineda M, Harris JD, Flanigan DC. Return to sport after articular cartilage repair in athletes’ knees: a systematic review. Arthroscopy. 2016;32(4):651–668.e651. [DOI] [PubMed] [Google Scholar]
- 7. Cole BJ. A randomized trial comparing autologous chondrocyte implantation with microfracture. J Bone Joint Surg Am. 2008;90(5):1165. [PubMed] [Google Scholar]
- 8. Drawer S, Fuller CW. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br J Sports Med. 2001;35(6):402–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gobbi A, Nunag P, Malinowski K. Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2005;13(3):213–221. [DOI] [PubMed] [Google Scholar]
- 10. Gudas R, Gudaite A, Pocius A, et al. Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med. 2012;40(11):2499–2508. [DOI] [PubMed] [Google Scholar]
- 11. Hangody L, Fules P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85-A(suppl 2):25–32. [DOI] [PubMed] [Google Scholar]
- 12. Harris JD, Brophy RH, Siston RA, Flanigan DC. Treatment of chondral defects in the athlete’s knee. Arthroscopy. 2010;26(6):841–852. [DOI] [PubMed] [Google Scholar]
- 13. Keng A, Sayre EC, Guermazi A, et al. Association of body mass index with knee cartilage damage in an asymptomatic population-based study. BMC Musculoskelet Disord. 2017;18(1):517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Knutsen G, Drogset JO, Engebretsen L, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture: findings at five years. J Bone Joint Surg Am. 2007;89(10):2105–2112. [DOI] [PubMed] [Google Scholar]
- 15. Kon E, Filardo G, Berruto M, et al. Articular cartilage treatment in high-level male soccer players: a prospective comparative study of arthroscopic second-generation autologous chondrocyte implantation versus microfracture. Am J Sports Med. 2011;39(12):2549–2557. [DOI] [PubMed] [Google Scholar]
- 16. Krych AJ, Robertson CM, Williams RJ, III; Cartilage Study Group. Return to athletic activity after osteochondral allograft transplantation in the knee. Am J Sports Med. 2012;40(5):1053–1059. [DOI] [PubMed] [Google Scholar]
- 17. Lindahl A, Brittberg M, Peterson L. Health economics benefits following autologous chondrocyte transplantation for patients with focal chondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(6):358–363. [DOI] [PubMed] [Google Scholar]
- 18. Lombardi AV, Jr, Nunley RM, Berend KR, et al. Do patients return to work after total knee arthroplasty? Clin Orthop Relat Res. 2014;472(1):138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR. Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med. 2009;37(suppl 1):167S–176S. [DOI] [PubMed] [Google Scholar]
- 20. Mithoefer K, Steadman RJ. Microfracture in football (soccer) players: a case series of professional athletes and systematic review. Cartilage. 2012;3(1)(suppl):18S–24S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mithoefer K, Williams RJ III, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34(9):1413–1418. [DOI] [PubMed] [Google Scholar]
- 22. Mithöfer K, Minas T, Peterson L, Yeon H, Micheli LJ. Functional outcome of knee articular cartilage repair in adolescent athletes. Am J Sports Med. 2005;33(8):1147–1153. [DOI] [PubMed] [Google Scholar]
- 23. O’Donoghue DH. Chondral and osteochondral fractures. J Trauma. 1966;6(4):469–481. [PubMed] [Google Scholar]
- 24. Pestka JM, Feucht MJ, Porichis S, Bode G, Sudkamp NP, Niemeyer P. Return to sports activity and work after autologous chondrocyte implantation of the knee: which factors influence outcomes? Am J Sports Med. 2016;44(2):370–377. [DOI] [PubMed] [Google Scholar]
- 25. Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A. Autologous chondrocyte transplantation: biomechanics and long-term durability. Am J Sports Med. 2002;30(1):2–12. [DOI] [PubMed] [Google Scholar]
- 26. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38(6):1117–1124. [DOI] [PubMed] [Google Scholar]
- 27. Richter DL, Schenck RC, Jr, Wascher DC, Treme G. Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health. 2016;8(2):153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Santos-Magalhaes AF, Hambly K. Measuring physical activity and sports participation after autologous cartilage implantation: a systematic review. J Sport Rehabil. 2014;23(3):171–181. [DOI] [PubMed] [Google Scholar]
- 29. Schroter S, Mueller J, van Heerwaarden R, Lobenhoffer P, Stockle U, Albrecht D. Return to work and clinical outcome after open wedge HTO. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):213–219. [DOI] [PubMed] [Google Scholar]
- 30. Scully WF, Parada SA, Arrington ED. Allograft osteochondral transplantation in the knee in the active duty population. Mil Med. 2011;176(10):1196–1201. [DOI] [PubMed] [Google Scholar]
- 31. Shaha JS, Cook JB, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Return to an athletic lifestyle after osteochondral allograft transplantation of the knee. Am J Sports Med. 2013;41(9):2083–2089. [DOI] [PubMed] [Google Scholar]
- 32. Upmeier H, Bruggenjurgen B, Weiler A, Flamme C, Laprell H, Willich SN. Follow-up costs up to 5 years after conventional treatments in patients with cartilage lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2007;15(3):249–257. [DOI] [PubMed] [Google Scholar]
- 33. Zarkadis NJ, Kusnezov NA, Garcia EJ, Pallis MP, Waterman BR. Return to preoperative function after autologous cartilage implantation of the knee in active military servicemembers. Orthop J Sports Med. 2017;5(5):2325967117706057. [DOI] [PMC free article] [PubMed] [Google Scholar]