An uneven landscape: Geographic disparities in cancer burden and underlying factors
Studies have shown time after time that where people live can affect what diseases they get, how they die, and when they die (1–6). In 2017, about fifteen percent of the U.S. population—about 46 million people—lived in rural areas. While geography alone cannot predict cancer risk, it can impact prevention, screening, diagnosis, and treatment opportunities. The articles in this special CEBP Focus issue on rural cancer control explore geographic disparities across the cancer control continuum in several distinct rural communities and map out potential paths to reach geographic health equity (7–12).
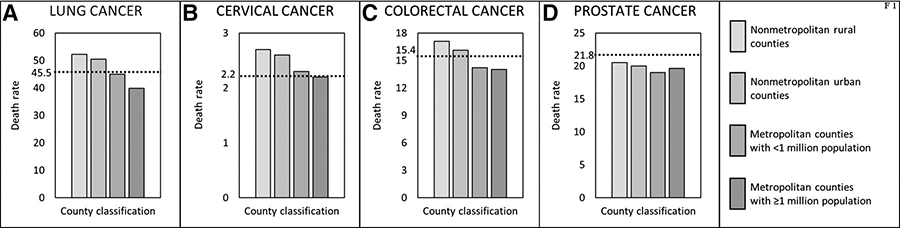
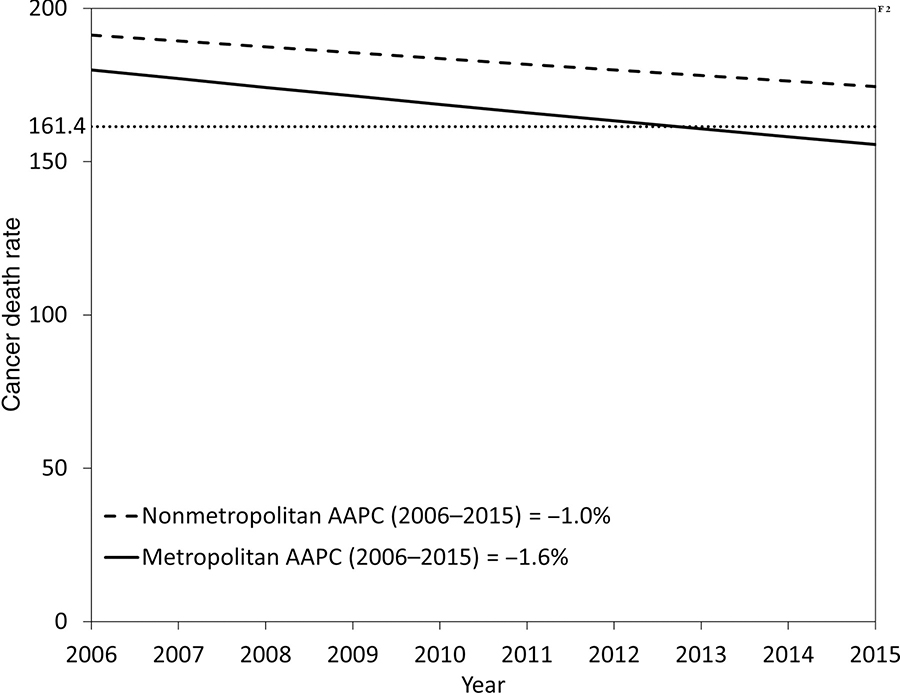
Cancers of the female breast, prostate, lung, and colorectal cancers are the most common cancers in the United States, in both rural and metropolitan areas (6). However, people who live in rural areas, compared with people who live in metropolitan areas, tend to have lower incidence rates for several cancer types that could be detected through screening and diagnostic imaging services (e.g., female breast, prostate, thyroid, and kidney cancers), but higher incidence rates for smoking-related cancers (e.g., lung and bladder cancer) and human papillomavirus (HPV)-related cancers (e.g., cervix cancer). Death rates are higher in persons residing in rural than metropolitan areas for many cancer types, particularly those amenable to primary prevention (e.g., lung cancer, Figure 1A and cervical cancer, Figure 1B), screening and early detection (e.g., colorectal cancer; Figure 1C), quality cancer treatment and cancer survivorship care (e.g., prostate cancer, Figure 1D). Moreover, progress in reducing cancer death rates for all cancers combined and for most common cancers has been slower in rural than in urban areas, further widening the disparity in mortality (Figure 2).
Figure 1.
Healthy People 2020 objectives for cancer and average annual death rates (per 100,000 persons, age-adjusted to the 2000 U.S. standard population) from selected cancers (A. Lung Cancer, B. Cervical Cancer, C. Colorectal Cancer, D. Prostate Cancer) by county classification—United States, 2011–2015. Healthy People 2020 objectives for cancer death rates are indicated with a dotted line (Reference 13). Counties were identified using the United States Department of Agriculture Economic Research Service 2013 vintage rural-urban continuum code, which categorizes nonmetropolitan counties by degree of urbanization and adjacency to a metro area, and metropolitan counties by the population size of their metro area (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/). (Adapted from Reference 6).
Figure 2.
Trends in cancer death rates (per 100,000 persons, age-adjusted to the 2000 U.S. standard population) from 2006 to 2015 in U.S. rural (nonmetropolitan) and metropolitan counties. The Healthy People 2020 objective for cancer death rate is indicated with a dotted line (Reference 13). Average annual percent change (AAPC) in rates calculated using joinpoint regression was used to describe trends. (Adapted from Reference 6)
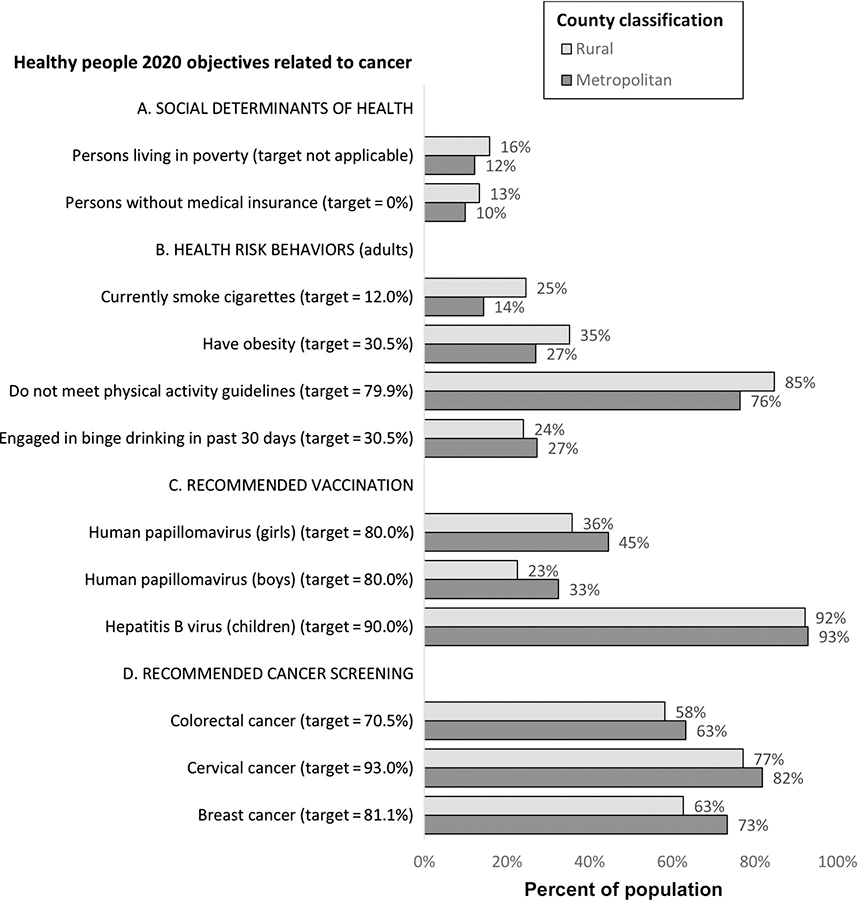
Factors contributing to slower progress and higher burden of cancer in rural areas are multi-factorial and include economic, social, and structural barriers. Persons residing in rural areas were more likely to live below the Federal poverty level (16%) than those residing in metropolitan areas (12%) and less likely to have medical insurance (13% vs 10%; Figure 3A) (13), potentially limiting access to recommended preventive, early detection, and treatment services (14–16). Prevalence of cigarette smoking, obesity, and physical inactivity, common risk factors for many cancer types (17), were higher among residents of rural areas than among residents of metropolitan areas (Figure 3B) (13, 18). Comprehensive tobacco prevention and control programs are proven to reduce smoking prevalence (19, 20); however; tobacco control efforts such as smokefree policies, excise taxes on tobacco products, and accessibility to smoking cessation resources tend to be lower in rural areas compared with metropolitan areas (13). Vaccination uptake rates for human papillomavirus (HPV) among adolescent boys and girls were lower in rural areas than in metropolitan areas, potentially impacting future cancer burden, (Figure 3C) (21) despite the availability of the vaccine to children to low-income families at no cost through a Federal program, Vaccines for Children (22). However, vaccination rates for hepatitis B virus among children were high (>90%) in both rural and metropolitan areas (Figure 3C), suggesting that barriers other than cost may impact low HPV vaccination rates. According to data from the 2015 National Health Interview Survey the prevalence of receiving recommended screening tests for female breast, colon and rectum, and cervical cancers (Figure 3D) were lower in persons residing in rural areas than among residents of metropolitan areas (13). Lower adherence to screening could be due to factors such as barriers to transportation to screening facilities, unaffordable screening tests, insufficient number of local screening facilities, or shortage of trained personnel, such as radiologists (6, 23). Persons residing in rural areas may be less likely to receive guideline concordant treatments. For example, receipt of radiation therapy for breast cancer patients residing in the National Cancer Institute’s Surveillance, Epidemiology and End Results program was lower for rural (62.1%) than urban (69.1%) patients (24). There are fewer primary healthcare providers and specialists in rural areas which may limit access to timely and high-quality prevention, early detection, treatment, and survivorship care services.
Figure 3.
Healthy People 2020 objectives related to cancer, including social determinants of health, health risk behaviors, recommended vaccination against cancer-causing viruses, and recommended cancer screening. Data for most indicators are from the 2015 or 2016 National Health Interview Surveys reported in the Healthy People 2020 database (Reference 13); data for poverty are from the 2016 Current Population Survey (Reference 13); data for obesity prevalence are from the 2016 Behavioral Risk Factor Surveillance System (Reference 18) and data for vaccination rates are from the 2015 National Immunization Survey (Reference 21).
Bridging the gap: Stories from the field
In this special CEBP Focus issue, six papers share new insights into cancer disparities in rural communities. A paper by Zahnd et al. examines cancer incidence rates and trends by demographic, geographic, and socioeconomic characteristics based on a multistate database, covering 93% of the US population, and confirms that cancer rates associated with modifiable risks, such as tobacco use and HPV infection, and some preventive screening modalities were higher in rural areas compared with urban areas (7). Zahnd and colleagues underscore the utility of such large and generalizable databases for monitoring the cancer burden in rural communities and other under-served populations to inform further research and public health efforts. Ross and colleagues examined progress in reducing lung cancer death rates among women from 1990 to 2015 by county, and found that while lung cancer death rates steadily decreased in most counties, they increased until the late 2000s in several rural counties in Appalachia and the Midwest, widening geographic inequities in lung cancer mortality (8). The authors noted that these geographic areas are characterized by weak tobacco control policies such as low excise tax on cigarettes and lack of comprehensive smoke-free policies banning smoking in all workplaces, restaurants and bars, and called for intensifying local tobacco control policies.
Paskett et al conducted a-year long church-based diet and exercise intervention trial with input from the community to reduce obesity in Appalachia (9). The authors found that participants who actively participated and attended more education sessions about physical activity and healthy diet were more likely to lose weight. However, the authors reported that only a third of participants regularly attended educational sessions and noted the need for more in-person contact to increase the impact of the intervention. Nevertheless, this trial demonstrates the importance of social gatherings such as churches as a vehicle to motivate healthy behaviors in rural and other underserved communities. Briant and colleagues showcased the benefits of using culturally tailored interventions to improve health awareness, knowledge, and behavior; their study showed that promotor(a)-led “home health parties” increased the use of fecal occult blood test screening from 51% to 80% among Hispanic men and women living in rural Washington State (10). McDougall et al studied colorectal cancer survivors in New Mexico and found that those who lived in rural areas were more likely to experience financial hardship and less likely to adhere to recommended follow-up care, highlighting the importance that place plays in affordable, accessible survivorship care (11). To examine the associations of neighborhood characteristics in Missouri with treatment and outcomes of ductal carcinoma in situ, Zhang, Liu and colleagues used census tract level socioeconomic deprivation and rural-urban commuting area codes to define rurality; while differences in treatment, but not outcome, were found, the authors suggest that larger studies using nuanced definitions of rurality are needed to refine our understanding the contribution of place to outcome (12). It is noteworthy that the definition, location, and composition of “rural” differ across the United States and these may affect the interpretation of the study findings included in this special issue.
Conclusion
The papers in this special issue describe disparities in cancer risk, screening, treatment, and outcome that exist in several different rural populations, confirming that not all communities in the United States have benefitted from advances in cancer prevention and control. These papers also describe novel approaches to promote physical activity, healthy eating habits, and CRC screening in rural areas through community participation, which could inform future studies and public health efforts to promote healthy behaviors and environments. Bridging the chasm in geographic health inequity requires such targeted, culturally appropriate, and sustainable interventions to improve access to primary prevention, early detection, and treatment services (23).
Footnotes
Conflicts of interest: We have no conflict of interest to declare.
Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94(10):1682–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomarkers Prev 2013;22(10):1657–67 doi 10.1158/1055-9965.epi-13-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh GK, Williams SD, Siahpush M, Mulhollen A. Socioeconomic, rural-urban, and racial inequalities in US cancer mortality: Part I-all cancers and lung cancer and Part II-colorectal, prostate, breast, and cervical cancers. J Cancer Epidemiol 2011:107497 doi 10.1155/2011/107497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blake KD Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiol Biomarkers Prev. 2017. June 9. doi: 10.1158/1055-9965.EPI-17-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moy E, Garcia MC, Bastian B, et al. Leading causes of death in nonmetropolitan and metropolitan areas—United States, 1999–2014. MMWR Surveill Summ 2017;66(No. SS-1):1–8. 10.15585/mmwr.ss6601a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henley SJ, Anderson R, Thomas CC, Massetti GM, Peaker B, Richardson LC. Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties — United States. MMWR Surveill Summ 2017;66(14):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, et al. Rural-urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Biomarkers Prev 2018; 27:1265–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross K, Kramer MR, Jemal A. Geographic inequalities in progress against lung cancer among women in the United States, 1990–2015. Cancer Epidemiol Biomarkers Prev 2018;27:1261–4. [DOI] [PubMed] [Google Scholar]
- 9.Paskett ED, Baltic RD, Young GS, Katz ML, Lesko SM, Webber KH, et al. A group randomized trial to reduce obesity among Appalachian church members: the walk by faith study. Cancer Epidemiol Biomarkers Prev 2018;27:1289–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briant KJ, Sanchez JI, Ibarra G, Escareño M,Gonzalez NE, Gonzalez VJ, et al. Using a culturally tailored intervention to increase colorectal cancer knowledge and screening among Hispanics in a rural community. Cancer Epidemiol Biomarkers Prev 2018;27:1283–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDougall JA, Banegas MP, Wiggins CL, Chiu VK, Rajput A, Kinney AY. Rural disparities in treatment-related financial hardship and adherence to surveillance colonoscopy in diverse colorectal cancer survivors. Cancer Epidemiol Biomarkers Prev 2018;27:1275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang S, Liu Y, Yun S, Lian M, Komaie G, Colditz GA. Impacts of neighborhood characteristics on treatment and outcomes in women with ductal carcinoma in situ of the breast. Cancer Epidemiol Biomarkers Prev 2018;27:1298–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Health and Human Services. Cancer. Healthy people 2020 Washington, DC: US Department of Health and Human Services; 2017. https://www.healthypeople.gov/2020/topics-objectives/topic/cancer [Google Scholar]
- 14.U.S. Preventive Services Task Force. Recommendations for primary care practice. 2017. https://www.uspreventiveservicestaskforce.org/Page/Name/recommendations
- 15.Schillie S, Vellozzi C, Reingold A, et al. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm Rep 2018;67(No. RR-1):1–31. DOI: 10.15585/mmwr.rr6701a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meites E, Kempe A, Markowitz LE. Use of a 2-Dose schedule for human papillomavirus vaccination — updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016;65;1405–8. DOI: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- 17.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31–54. [DOI] [PubMed] [Google Scholar]
- 18.Lundeen EA, Park S, Pan L, O’Toole T, Matthews K, Blanck HM. Obesity prevalence among adults living in metropolitan and nonmetropolitan counties — United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:653–658. DOI: 10.15585/mmwr.mm6723a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frieden TR, Myers JE, Krauskopf MS, Farley TA. A public health approach to winning the war against cancer. Oncologist 2008;13:1306–13. 10.1634/theoncologist.2008-0157 [DOI] [PubMed] [Google Scholar]
- 20.Community Preventive Services Task Force. 2014–2015 Annual report to Congress, Federal agencies and prevention stakeholders, including a special update on recommendations to prevent cancers. 2015. https://www.thecommunityguide.org/sites/default/files/assets/2015-congress-report-full_0.pdf.
- 21.National Center for Health Statistics. Health, United States, 2016: With chartbook on long-term trends in health. Hyattsville, MD: 2017. https://www.cdc.gov/nchs/data/hus/hus16.pdf [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Vaccines for Children Program. https://www.cdc.gov/vaccines/programs/vfc/index.html.
- 23.Wheeler SB, Basch E. Translating cancer surveillance data into effective public health interventions. JAMA. 2017;317(4):365–367. [DOI] [PubMed] [Google Scholar]
- 24.Baldwin LM, Patel S, Andrilla CH, Rosenblatt RA, Doescher MP. Receipt of recommended radiation therapy among rural and urban cancer patients. Cancer. 2012. October 15;118(20):5100–9. doi: 10.1002/cncr.27488. [DOI] [PubMed] [Google Scholar]