INTRODUCTION
The rate of diabetes-related complications among Americans with diabetes has declined significantly over the past two decades.1 However, it remains unclear how complication rates have changed across different racial/ethnic groups, as past studies on diabetes complication disparities are either outdated, restricted to limited populations, did not examine trends, or included only limited race/ethnicity categories.1–4 Therefore, we used nationally representative data to examine prevalence trends in several diabetes complications from 1997 to 2017 among Whites, Blacks, and Hispanics in the USA.
METHODS
The National Health Interview Survey (NHIS) from 1997 to 2017 was used to identify non-Hispanic White, non-Hispanic Black, and Hispanic adults aged 20 years or older with self-reported diagnoses of diabetes mellitus (type 1 or 2). The two outcomes of interest were (1) a cardiovascular complication composite defined as patients experiencing either coronary heart disease, acute myocardial infarction, or angina and (2) chronic kidney disease, defined as having “weak or failing kidneys in the past 12 months,” excluding kidney stones, bladder infections, or incontinence.
Prevalence estimates were adjusted using NHIS weights and standardized to the 2000 US Census Population using four age categories: 20–44, 45–64, 65–74, and 75+.1 Significance of time trends and racial/ethnic disparities was assessed via logistic regressions involving year, race, year-race interactions, and age group dummies. All analyses were conducted using Stata version 14.1. This study was approved by an institutional review board at University of Southern California.
RESULTS
The final analytic sample included 31,722 Whites, 11,020 Blacks, and 9389 Hispanics. For cardiovascular complications, although White patients experienced higher rates of complications than Black or Hispanic patients in 1997, the difference became narrower by 2017 (Fig. 1). A significant decline in the rate of cardiovascular complications was observed only among White patients (a decline of 4.28 percentage points; p < 0.001). This improvement was marginally statistically distinguishable from trends for Black and Hispanic patients (p = 0.048 and p = 0.056, respectively).
Figure 1.
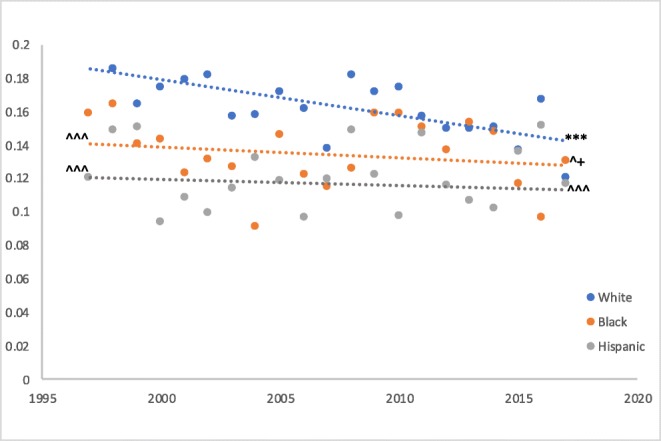
Age-adjusted prevalence of cardiovascular complications, 1997–2017. Trendline was created from logit predictions of the age-adjusted prevalence rates. Significance testing was done using the logit-predicted prevalence rates. Asterisk symbols indicate a statistically significant time trend (*p< 0.05; **p< 0.01; ***p< 0.001). A plus sign indicates statistically significant difference in time trends between White/Black and White/Hispanic patients. Upward-pointing arrowheads indicate statistically significant difference in predicted prevalence between White/Black and White/Hispanic patients in a given year (either 1997 or 2017).
For renal complications, prevalence was lower among White patients than Black or Hispanic patients at baseline (Fig. 2). Significant changes in prevalence between 1997 and 2017 were observed only among White patients (an increase of 2.04 percentage points; p < 0.001). Renal complication trends converged between White and Hispanic patients (p = 0.03), and no significant White-Hispanic difference in prevalence was observed by 2017.
Figure 2.
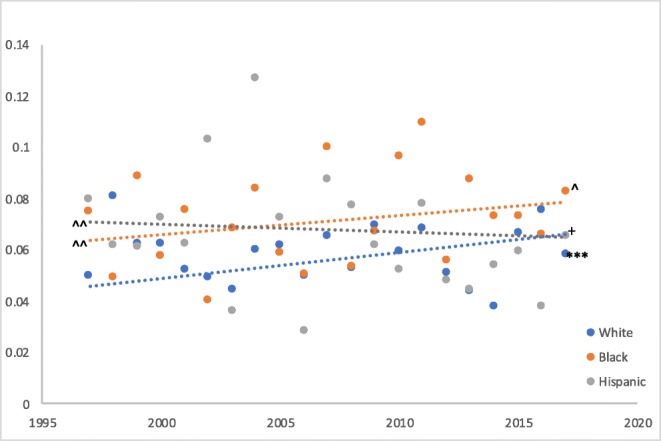
Age-adjusted prevalence of chronic kidney disease, 1997–2017. Trendline was created from logit predictions of the age-adjusted prevalence rates. Significance testing was done using the logit-predicted prevalence rates. Asterisk symbols indicate a statistically significant time trend (*p< 0.05; **p< 0.01; ***p< 0.001). A plus sign indicates statistically significant difference in time trends between White/Black and White/Hispanic patients. Upward-pointing arrowheads indicate statistically significant difference in predicted prevalence between White/Black and White/Hispanic patients in a given year (either 1997 or 2017).
DISCUSSION
Using a nationally representative sample of non-institutionalized individuals in the USA, we found significant differences in the trends of diabetes complications among different races/ethnicities over the last two decades. Specifically, the rate of cardiovascular complications declined among White patients, while trends for Blacks and Hispanics were insignificant. We also found that the rates of renal complications have increased among White patients, resulting in convergence in prevalence among White and Hispanic patients.
Our findings are consistent with past studies focused on specific patient cohorts from 1995 to 2010, which have generally found Blacks and Hispanics to experience higher rates of renal complications but lower rates of cardiovascular complications compared to Whites.2–4 However, higher rates of cardiovascular complications among Whites contradict the broader literature that has found minority patients with worse intermediate outcomes and cardiovascular risk factors.3, 5, 6 One potential explanation is that patients from different racial/ethnic groups have had different probabilities of receiving a complication diagnosis, arising from changes in provider behavior or healthcare access.3, 5
A recent study observed significant changes in the rates of diabetes-related complications among US patients over the past two decades.1 Our findings highlight the importance of examining these trends by racial/ethnic groups to discern the extent to which the documented improvements have been distributed equitably, as well as identify opportunities to improve care for specific diabetes patient populations. Further research is needed to characterize the drivers of racial/ethnic differences in diabetes complications.
Author Contribution
Chiou contributed to the design of the study, conducted the data analyses, led the interpretation of the data and drafting and revisions of the article, and takes full responsibility for the contents of the article. Tsugawa contributed to the design of the study, interpretation of the data, and the revisions of the article for important intellectual content. Goldman, Myerson, and Kahn contributed to the conceptualization and design of the study, as well as the interpretation of the data. Romley led the conceptualization and design of the study, and contributed to the interpretation of the data and revisions of the article for important intellectual content.
Compliance with Ethical Standards
This study was approved by an institutional review board at University of Southern California.
Conflict of Interest
Goldman is a consultant to Precision Health Economics, a healthcare consultancy providing services to the life sciences industry, and owns equity (< 1%) in its parent company, Precision Medicine Group. Myerson reports grant funding from Bristol-Myers Squibb for investigator-initiated research. Romley is a consultant to Precision Health Economics. Chiou, Tsugawa, and Kahn report nothing to disclose. These relationships did not impact the design, execution, or interpretation of this study.
Footnotes
Prior Presentations
None
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990–2010. New Engl J Med. 2014;370(16):1514–1523. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Katzmarzyk PT, Horswell R, et al. Racial disparities in diabetic complications in an underinsured population. J Clin Endocrinol Metab. 2012;97(12):4446–4453. doi: 10.1210/jc.2012-2378. [DOI] [PubMed] [Google Scholar]
- 3.Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diab Rep. 2013;13(6):814–823. doi: 10.1007/s11892-013-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osborn CY, De Groot M, Wagner JA. Racial and ethnic disparities in diabetes complications in the northeastern United States: the role of socioeconomic status. J Natl Med Assoc. 2013;105(1):51–58. doi: 10.1016/S0027-9684(15)30085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi Q, Zhao Y, Fonseca V, Krousel-Wood M, Shi L. Racial disparity of eye examinations among the US working-age population with diabetes: 2002–2009. Diabetes Care. 2014;37(5):1321–1328. doi: 10.2337/dc13-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36(8):2271–2279. doi: 10.2337/dc12-2258. [DOI] [PMC free article] [PubMed] [Google Scholar]


