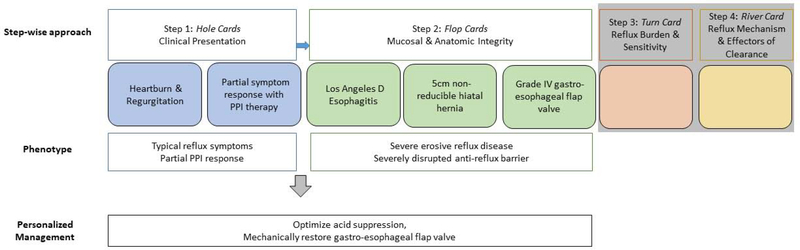
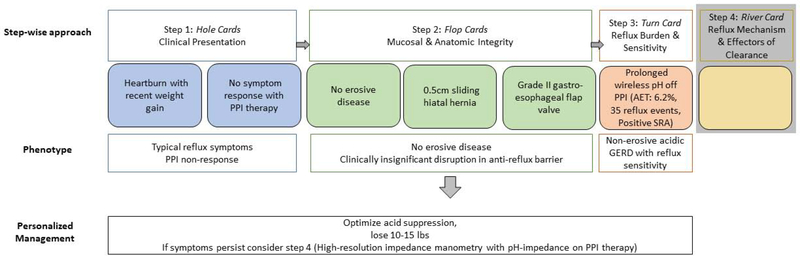
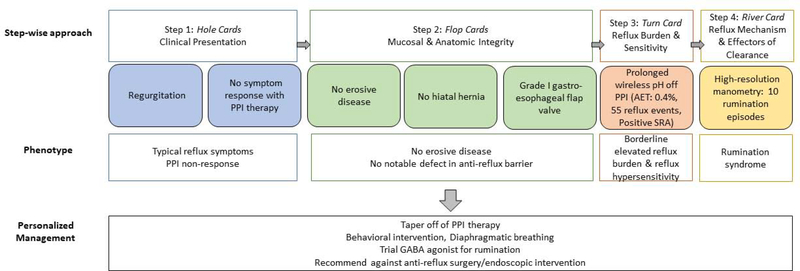
Figure 5. Step-wise phenotype approach for three patient examples (A, B, C).
Example 5A: A 65 year old man is referred for heartburn and regurgitation partially responsive to PPI (hole cards) and undergoes upper GI endoscopy which reveals a 5cm non-reducible hiatal hernia with grade IV gastroesophageal flap valve and LA D esophagitis (flop cards). This patient’s phenotype is clear at this point (typical reflux symptoms with partial PPI response, erosive reflux disease and a severely disrupted anti-reflux barrier), and thus phenotype guided management can proceed without further evaluation. Management in this case will hinge on optimizing acid suppression and mechanical restoration of the gastro-esophageal flap valve.
Example 5B: A 65-year old man with recent weight gain, heartburn, and no response to PPI therapy (hole cards) undergoes upper GI endoscopy which reveals normal esophageal mucosa, a 0.5cm sliding hiatal hernia and grade II gastroesophageal flap valve (flop cards). The GERD phenotype is not clear at this point, and the next step is ambulatory reflux monitoring. Since the patient has a low pre-test probability of GERD, the patient undergoes prolonged wireless pH monitoring off PPI therapy. The acid exposure time (AET) is elevated. Thus, this patient’s phenotype is: heartburn symptoms with recent weight gain, PPI non-responder with non-erosive acidic reflux disease. At this point you can attempt management without further diagnostic evaluation focused on weight loss and optimizing acid suppression. However, if symptoms persist further evaluation with esophageal manometry and impedance-pH monitoring on PPI (river card) would be warranted.
Example 5C: A 65-year old man is referred to clinic for regurgitation and no response to PPI therapy (hole cards) and undergoes upper GI endoscopy which reveals normal esophageal mucosa, no hiatal hernia, and grade I gastroesophageal flap valve (flop cards). The GERD phenotype is unclear and so the next step is ambulatory reflux monitoring, which demonstrates an inconclusive number of reflux events, normal acid exposure, and positive symptom-reflux association for regurgitation (SI 100%, SAP 99%). (turn card) Given inconclusive findings and suspicion for rumination the next step is esophageal physiologic testing with manometry and pH impedance on PPI therapy which uncovers rumination syndrome. At this point the phenotype is clear (PPI non-responder with rumination) and management will focus on behavioral intervention, diaphragmatic breathing and trial of GABA agonist. In this case you will refrain from referring for anti-reflux surgery.