Abstract
Background:
Current tools to predict the severity of respiratory syncytial virus (RSV) infection might be improved by including immunological parameters. We hypothesized that a combination of inflammatory markers would differentiate between severe and mild disease in RSV-infected children.
Methods:
Blood and nasopharyngeal samples from 52 RSV-infected children were collected during acute infection and after recovery. Retrospectively, patients were categorized into three groups based on disease severity: mild (no supportive treatment), moderate (supplemental oxygen and/or nasogastric feeding), and severe (mechanical ventilation). Clinical data, number of flow-defined leukocyte subsets, and cytokine concentrations were compared.
Results:
Children with severe RSV infection were characterized by young age; lymphocytopenia; increased interleukin (IL)-8, granulocyte colony-stimulating factor (G-CSF), and IL-6 concentrations; and decreased chemokine (C-C motif) ligand (CCL-5) concentrations in plasma. The combination of plasma levels of IL-8 and CCL-5, and CD4+ T-cell counts, with cutoff values of 67 pg/ml, 13 ng/ml, and 2.3 × 106/ml, respectively, discriminated severe from mild RSV infection with 82% sensitivity and 96% specificity.
Conclusion:
This study demonstrates that the combination of CD4+ T-cell counts and IL-8 and CCL-5 plasma concentrations correlates with disease severity in RSV-infected children. In addition to clinical features, these immunological markers may be used to assess severity of RSV infection and guide clinical management.
Supplementary information
The online version of this article (doi:10.1038/pr.2012.163) contains supplementary material, which is available to authorized users.
Subject terms: Diagnostic markers, Viral infection, Paediatrics
Main
Respiratory syncytial virus (RSV) is a common cause of bronchiolitis in young children (1,2). The clinical manifestations of RSV infection range from a common cold to severe lower respiratory tract infections requiring mechanical ventilation. About 1–2% of RSV-infected children are hospitalized (3,4,5), of which 6–11% require intensive care admission (3,6). Although young age, prematurity, congenital heart diseases, chronic lung diseases, and immune deficiencies are risk factors for severe RSV infection, more than half of the RSV-infected children requiring intensive care admission were otherwise healthy (3,7).
It has been reported that 35% of children hospitalized with bronchiolitis did not receive any supportive intervention (8). On the other hand, it is crucial that those children who may experience clinical deterioration are not discharged. Among those sent home with a diagnosis of bronchiolitis, 4.6–6.8% required hospitalization later on during infection (9,10). Clinical prediction models may help clinicians to distinguish RSV-infected children requiring hospitalization from those who can be safely sent home. To date, mainly clinical parameters have been used to predict the severity of disease in RSV infection (11,12). Several studies have associated severity of RSV disease with particular cytokines such as interleukin (IL)-8, IL-6, IL-4, and interferon (IFN)-γ (13,14,15,16). A change in plasma or nasopharyngeal levels of these cytokines early in the host response can be used as early markers for severity of disease. The addition of inflammatory parameters may improve the prediction of disease severity in children with RSV infections.
To examine whether a combination of these inflammatory mediators can differentiate between severe and mild RSV infection, we characterized immune cells (CD4+ and CD8+ T cells, natural killer (NK) cells, monocytes, and B cells) and measured concentrations of 16 cytokines and chemokines in young children with RSV bronchiolitis.
Results
Severity of RSV Infection Is Associated With Young Age
Demographics and clinical features of the 52 included infants are presented in Table 1. Children with severe disease were significantly younger than those with mild or moderate disease (1.0 vs. 2.0 and 5.3 mo; P < 0.01 and P = 0.04, respectively). No other significant differences in clinical parameters were observed.
Table 1.
Demographics of children diagnosed with an RSV infection and categorized by severity of disease
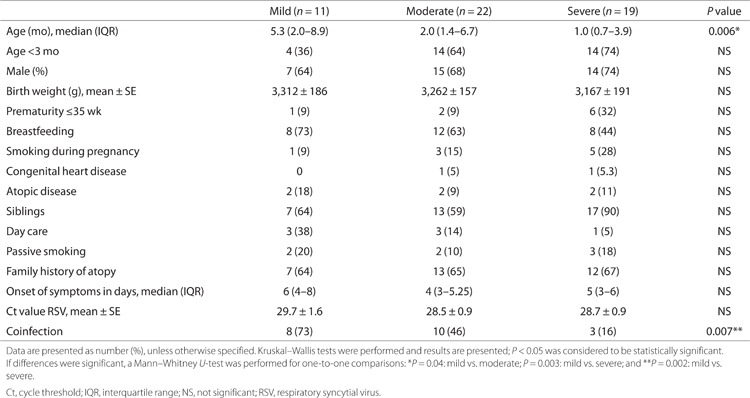
RSV Monoinfection Is Associated With Disease Severity, Irrespective of Viral Load
An examination of the nasopharyngeal samples detected RSV in all the samples. In 21 of 53 samples (40%), one or more other viruses than RSV were detected, of which rhinovirus was most frequently detected (n = 17). Viral coinfection occurred more often in children with mild RSV infection (73%) as compared with those with moderate (46%) and severe disease (16%; P < 0.01). No differences in RSV load were observed between the severity groups or between children with RSV monoinfections and those infected by multiple viruses.
Severity of RSV Infection Is Associated With Lymphocytopenia
No differences were found in the numbers of granulocytes, monocytes, or B cells between the severity groups (Figure 1). Severe RSV infection was associated with lower CD4+ T-cell, CD8+ T-cell, and NK-cell counts as compared with mild or moderate infection. During recovery, the number of NK cells, CD4+ T cells, and CD8+ T cells in children with severe RSV infection increased to normal values for age (Supplementary Figure S1 online). No differences were found in immunophenotyping of fresh or cryopreserved peripheral blood mononuclear cells (PBMCs) (data not shown).
Figure 1.
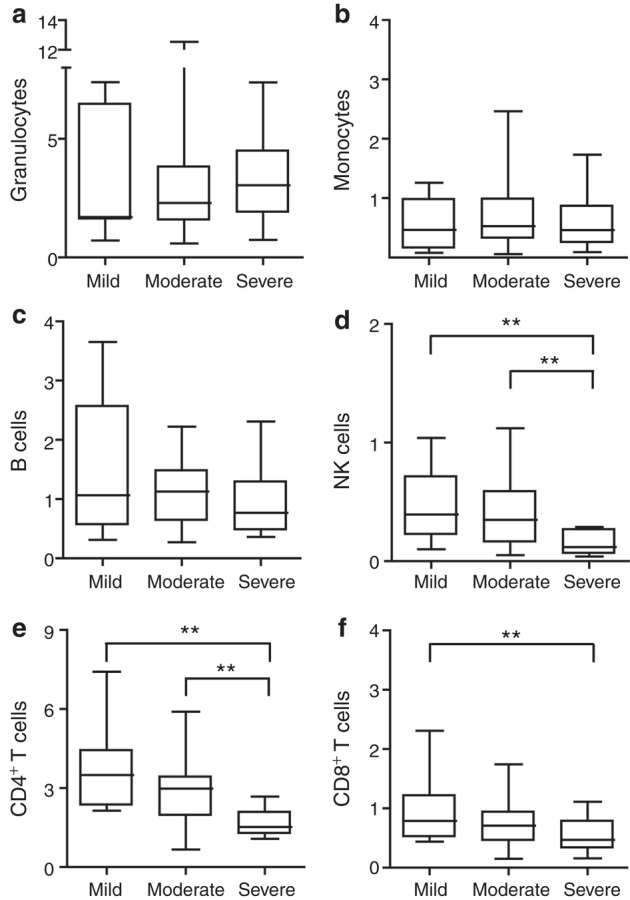
Absolute cell counts of leukocyte subsets in blood from children with an RSV infection categorized by disease severity. Cell counts of (a) granulocytes, (b) monocytes, (c) B cells, (d) NK cells, (e) CD4+ T cells, and (f) CD8+ T cells are expressed as 106 cells/ml. Data are plotted as medians with the 25th–75th percentile range. Mann–Whitney U-tests were performed, **P < 0.01. NK, natural killer; RSV, respiratory syncytial virus.
Severity of RSV Infection Is Associated With High IL-8, IL-6, and G-CSF, and Low CCL-5 Plasma Concentrations
Cytokine concentrations in plasma and nasopharyngeal aspirates in the three patient groups are summarized in Table 2 and Supplementary Table S1 online. Cytokines that were present in less than 30% of the acute blood and nasopharyngeal samples were excluded from further analyses (Supplementary Tables S2 and S3 online).
Table 2.
Cytokine and chemokine concentrations (pg/ml) in plasma of children with mild, moderate, or severe RSV infection
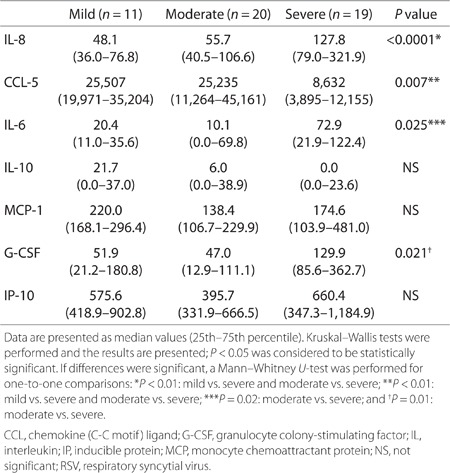
In children with severe disease, IL-8, IL-6, and granulocyte colony-stimulating factor (G-CSF) plasma concentrations were higher than in those with mild or moderate disease (Table 2). In contrast, severe disease was associated with lower chemokine (C-C motif) ligand (CCL-5) plasma concentrations as compared with mild or moderate disease (P < 0.01). Whereas CCL-5 concentrations were higher during acute infection as compared with those during recovery in the moderate group (P = 0.03), CCL-5 plasma levels were lower during acute infection as compared with those during recovery in the severe group (P = 0.01). In addition, CCL-5 plasma concentrations during recovery were significantly higher in the moderate group than in the severe group (P = 0.03).
No significant differences in the percentage or absolute numbers of IL-4– and IFN-γ–producing CD4+ and CD8+ T cells were observed in children with severe RSV infection as compared with those with mild or moderate RSV infection (Supplementary Table S4 online).
Severity of RSV Infection Is Associated With High IL-6 Nasopharyngeal Concentrations
Overall, nasopharyngeal cytokine concentrations were higher during acute infection than after recovery (Supplementary Table S3 online). Higher IL-6 concentrations were found in nasopharyngeal samples from children with moderate or severe disease as compared with those with mild disease (P < 0.05). No other significant differences in nasopharyngeal cytokine levels were found between the patient groups (Supplementary Table S1 online).
Inflammatory Parameters Distinguish Disease Severity in RSV-Infected Infants Younger Than 3 mo and in Children With Single RSV Infection
Given that severe disease was associated with younger age, we also performed analyses in infants within 3 mo of birth. Because of the small numbers, we categorized these infants into two groups: ventilated (15) and nonventilated (18). In this young age group, higher IL-8, IL-6, and G-CSF plasma concentrations, lower CCL-5 plasma concentrations, and lower NK cell and CD4 T-cell counts were observed in ventilated as compared with nonventilated RSV-infected infants (Table 3).
Table 3.
Significant differences in clinical and inflammatory parameters between ventilated and nonventilated RSV-infected infants within 3 mo of birth
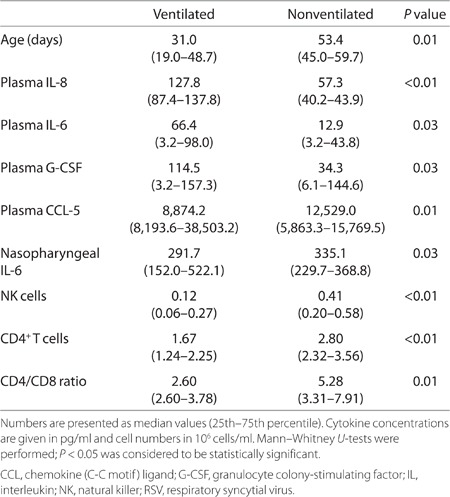
As infection by multiple viruses may have influenced our results, we analyzed inflammatory parameters in 16 ventilated and 15 nonventilated children with RSV single infections. No significant differences in age and clinical parameters were found. Significantly higher IL-8, IL-6, and G-CSF and, although not significant, lower CCL-5 plasma concentrations (P = 0.06) were observed in ventilated children as compared with nonventilated children. In addition, CD4+ T-cell and NK cell but not CD8+ T-cell counts were lower in ventilated children than in nonventilated children.
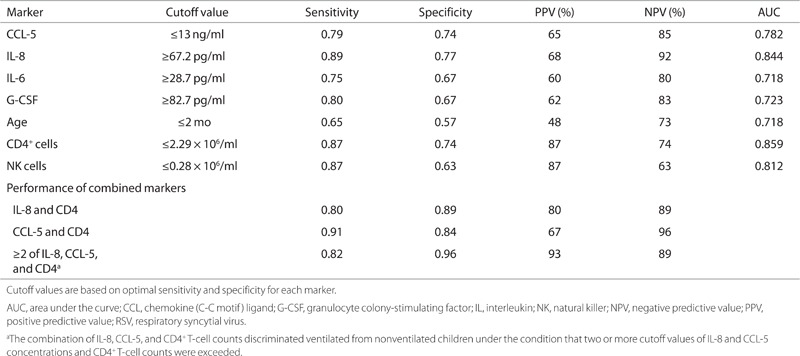
Combination of IL-8, CCL-5, and CD4+ T-cell Count Discriminates Severe RSV Infection From Mild RSV Infection
Clinical and inflammatory parameters that were significantly different between the patient groups (Table 4) were selected for further analyses. On the basis of the receiver operating characteristic curves, cutoff values were calculated (67 pg/ml, 13 ng/ml, and 2.3 × 106 cells/ml for IL-8 and CCL-5 plasma levels and CD4 T-cell counts, respectively). IL-8 plasma levels and CD+ T-cell counts showed high sensitivity (89% and 87%, respectively) and specificity (77% and 74%, respectively), followed by CCL-5 with a sensitivity of 79% and specificity of 74%. We explored the possibility of using a combination of markers to predict disease severity. The combination of IL-8 and CCL-5 levels and CD4+ T-cell counts predicted disease severity with a sensitivity of 82% and specificity of 96%, if two of three cutoff values within a patient were above or below the threshold. Positive and negative predictive values were 93% and 89%, respectively, for this combination of markers.
Table 4.
Comparison of sensitivity, specificity, PPVs, NPVs, and AUC for different inflammatory markers in ventilated vs. nonventilated children with RSV bronchiolitis
Discussion
This study demonstrates that CD4+ T-cell counts and IL-8 and CCL-5 plasma concentrations may be a useful set of markers for distinguishing disease severity in young children with RSV bronchiolitis. Therefore, by including immunological inflammatory parameters, current clinical prediction models for severity of RSV infection may be improved.
In our study, young age, lymphocytopenia, and IL-8, IL-6, G-CSF, and CCL-5 plasma levels were associated with severe RSV infection. Young age is a known risk factor for severe RSV infection. An immature immune system, in combination with the lack of in utero sensitization to RSV and small airways, indicates that severe RSV infections are predominantly observed in young infants (17). However, age alone cannot explain the observed differences in inflammatory parameters because our analyses in infants within 3 mo of birth still showed significant differences in inflammatory parameters between the severity groups.
In line with previous studies (18,19,20), lower T-cell and NK-cell counts were observed during severe RSV infection as compared with milder infections. Given that young infants have normally higher T-cell and NK-cell counts than older children (21,22), the degree of lymphocytopenia may even have been underestimated in this patient group. This lymphocytopenia can be explained by either migration of lymphocytes into the airways or apoptosis (13,18,19,23). Another hypothesis may be that infection-induced immune suppression results in lower lymphocyte counts.
As previously described (15), our results show that RSV infections induce a systemic response reflected by changes in cytokine plasma concentrations. Despite the significantly higher IL-8, IL-6, and G-CSF and lower CCL-5 concentrations in plasma during severe RSV infection as compared with milder infection, in nasopharyngeal aspirates, only IL-6 was significantly higher during severe RSV infection. Given that nasopharyngeal samples do not necessarily reflect local inflammation in the lower airways (24), and sampling methods and correction for dilutional effects differ between studies, the use of cytokines in nasopharyngeal samples as biomarkers is complicated. Because blood samples are relatively easy to obtain in a uniformly established manner, and cytokine plasma levels were all normalized at the time of recovery, cytokine levels in plasma are potential biomarker candidates for diagnostic use.
In contrast to increased IL-8, IL-6, and G-CSF levels, CCL-5 plasma concentrations were decreased during severe RSV infection as compared with those after recovery and milder manifestations of RSV infection. Although our results differ from some studies that observed increased CCL-5 concentrations in respiratory samples (24,25) and blood (26) during acute RSV infection as compared with healthy controls, they are consistent with others showing lower CCL-5 concentrations in blood during acute infection as compared with recovery samples (27,28). The fact that not all studies examined recovery samples or evaluated disease severity may explain these differences.
Although CCL-5 is initially produced by local innate immune cells to attract T cells and monocytes to the site of infection, CD4+ and CD8+ T cells have been described as the main source of the second peak of CCL-5, which occurs 5–7 d after infection (29). A decrease in T cells may therefore result in lower CCL-5 levels. However, the discrepancy between T-cell counts and CCL-5 levels during recovery in the moderate and severe groups suggests that the lower T-cell counts cannot completely explain the lower CCL-5 levels during severe RSV infection. Other mechanisms such as an inadequate or suppressed T-cell response may play a role. Infection-induced immune suppression is a well-established phenomenon and has been described in sepsis, measles, and chronic viral infections (30,31,32). The immature immune system of infants can also result in a reduced immune response. Controversial results have been published on changes in CCL-5 levels during the first months of life, and we cannot exclude that higher CCL-5 levels reflect functional maturation of the immune system (33,34). However, in infants within 3 mo of birth, we still observed significantly lower CCL-5 concentrations in ventilated infants than in nonventilated infants.
The inflammatory response during severe RSV infection has been associated with atopy and asthma, although the precise mechanism behind this relation is still unclear (35). It has been suggested that an IL-4–induced Th2 response during primary RSV infection might play a role in the development of atopic disease, although this could also be due to a shared etiology of bronchiolitis and asthma (36). If this had played a role in our study, one would expect differences in IL-4–producing T-cell subsets or differences in the prevalence of atopic disease. However, no differences between severe and nonsevere patients were found. Therefore, it is unlikely that the inflammatory markers found to be associated with disease severity can be explained by the existing atopy or the development of atopic disease.
Some limitations of our study need to be considered. Multiple viruses were detected in 40% of the samples, and these coinfections were associated with less severe RSV infection. Although comparing single RSV infections between ventilated and nonventilated children gave results similar to those of the analyses in which multiple infections were included, the possibility that the presence of other viruses induced a different inflammatory response cannot be entirely excluded. Another important consideration regarding markers for disease severity is that they do not have clinical implications at this moment, because currently no antiviral treatment is available. However, newly developed antiviral treatment of patients will be based most likely on diagnostics predicting disease severity and susceptibility (37,38). For the evaluation of intervention studies, such as vaccination and antiviral treatment, markers for disease severity will be valuable. Furthermore, given that we focused on the discrimination between ventilated and nonventilated children, studies need to be undertaken to determine whether this set of biomarkers could also discriminate between children requiring hospitalization and those who can be discharged.
In summary, we demonstrate the usefulness of a combination of immunological markers to distinguish disease severity in young RSV-infected children. We conclude that prediction models of RSV infection in young children may be improved by including immunological parameters, such as IL-8 and CCL-5 concentrations and CD4+ T-cell counts. Future studies have to be performed to validate our findings to see whether the use of these parameters may contribute to early recognition of children developing severe RSV infection. This may guide clinicians to decide whether a child needs to be hospitalized and to initiate symptomatic therapy in an early phase of disease.
Methods
Study Design
Children below 2 y of age with RSV bronchiolitis were prospectively included during three consecutive winter seasons (from November to April 2006–2009). Bronchiolitis was defined as an acute infection of the lower airways, characterized by increased respiratory effort and expiratory wheezing and/or crackles and/or apnea. The study was approved by the Committee on Research Involving Human Subjects of the University Nijmegen Medical Center, and written informed consent was obtained from all parents. Within 24 h after presentation, blood and nasopharyngeal samples were collected; and from hospitalized children, permission was asked of the parent or guardian for a recovery sample 4–6 wk later. Clinical data were collected from questionnaires and medical records. Retrospectively, based on the clinical course, patients were classified into three different groups: children without supportive interventions were allocated to the mild group; those requiring hospitalization for supplemental oxygen (oxygen saturations below 93%) and/or nasogastric feeding were allocated to the moderate group; and children requiring mechanical ventilation were allocated to the severe group.
Sample Collection
Nasopharyngeal aspirates were collected by introducing a catheter into the nasopharynx. Then, 1.5 ml saline was instilled into the nose and, while slowly retracting the catheter, the nasopharyngeal fluid was aspirated in a collection tube. Subsequently, the catheter was flushed with 1 ml saline, which was added to the collection tube. The samples were cooled and immediately transported to the laboratory. The nasopharyngeal aspirate was centrifuged and the supernatant was frozen at −80 °C.
A total of 5 ml of blood was collected into sodium heparin tubes and processed within 2 h. Blood smears were stained with May-Grunwald-Giemsa to determine the percentages of granulocytes. PBMCs were obtained by density gradient centrifugation (Lymphoprep, Axis Shield, Oslo, Norway) and stored in liquid nitrogen after cryopreservation. Immunophenotyping was performed on either fresh blood cells or on viably frozen PBMCs to determine the leukocyte subsets. Plasma samples, diluted 1:1 with phosphate-buffered saline, were stored at −80 °C for cytokine analyses.
Virus Detection
Multiplex real-time reverse transcription PCR was performed on nasopharyngeal aspirates as previously described (39). The multiplex real-time PCR assay detects 15 different viral pathogens: influenza virus type A and B, coronavirus 229E and OC43, human bocavirus, enterovirus, adenovirus, parechovirus, parainfluenza virus types 1–4, human metapneumovirus, rhinovirus, and RSV. The amount of virus was recorded semiquantitatively based on the cycle threshold value.
Immunophenotyping
Erythrocytes were eliminated from heparinized blood by using ammonium chloride lysis; the remaining leukocytes were washed with phosphate-buffered saline and resuspended in phosphate-buffered saline with 0.5% bovine serum albumin. Leukocyte subsets were analyzed using immunofluorescence-labeled monoclonal antibodies determined in multicolor flow cytometry. Depending on the number of cells, 50 µl of cell suspension containing maximally 1 × 106 nucleated cells was incubated with 50 µl fluorochrome-labeled monoclonal antibodies (final dilution 1:20) for 15 min in the dark at room temperature. Combinations of mAb conjugates were used for CD3, CD4, CD8, CD56, CD45, CD14, and CD19 (Beckman Coulter, Miami, FL). Cells were enumerated by using flow-count counting beads (Beckman Coulter). Staining of cells was determined by using a Fc500 flow cytometer (Beckman Coulter). Data were analyzed using the CXP software (Beckman Coulter).
Immunophenotyping of cryopreserved PBMCs and intracellular cytokine staining were performed after thawing. The following combinations of markers and fluorescent antibodies were used: CD14–FITC, CD16.56–phycoerythrin, IL-4–PE, CD3–peridinin chlorophyll protein, CD19–allophycocyanin, IFN-γ–allophycocyanin, CD4–phycoerythrin–Cy7, and CD8–allophycocyanin–Cy7. Extracellular staining of surface markers CD14, CD16.56, CD3, CD4, and CD8 was performed in 96-well microtiter plates. For intracellular cytokine staining (IL-4 and IFN-γ), PBMCs were stimulated with β-mercapto-ethanol, phorbol myristate acetate (10 ng/ml), golgistop, and ionomycin at 37 °C for 4 h. Then, staining of surface markers CD3, CD4, and CD8 was performed. Thereafter, cells were fixed, permeabilized with 0.5% saponin and 0.5% bovine serum albumin in phosphate-buffered saline, and stained for intracellular IL-4 and IFN-γ. Samples were acquired immediately after staining on a BD FACSCanto (Becton Dickinson, Heidelberg, Germany) and analyzed using flow cytometry analysis software (FlowJo analyses 7.6, Three Star, Ashland, OR).
Cytokine Concentrations
Concentrations of the cytokines IL-1β, IL-2, IL-4, IL-6, IL-10, IL-12p70, IL-13, IL-17, G-CSF, granulocyte-macrophage colony-stimulating factor, IFN-γ, and tumor necrosis factor and the chemokines IL-8 (chemokine CXC ligand 8), IFN-γ–inducible protein-10, monocyte chemoattractant protein-1, and CCL-5 were measured by flow cytometry using the BD CBA Human Soluble Flex Set system (Becton Dickinson) according to the manufacturer’s instructions. Briefly, cytokine-specific antibody–coated beads were incubated for 1 h with 25 µl plasma, supernatant of nasopharyngeal aspirates, or standard solution. Thereafter, samples were incubated with the corresponding phycoerythrin-labeled detection antibodies for 2 h. After washing, samples were measured by flow cytometry. Analysis of data and quantification of cytokines were performed using FCAP Array software (Becton Dickinson).
The detection limits were 2.3 pg/ml for IL-1β, 11.2 pg/ml for IL-2, 1.4 pg/ml for IL-4, 1.6 pg/ml for IL-6, 0.13 pg/ml for IL-10, 0.6 pg/ml for IL-12p70, 0.6 pg/ml for IL-13, 0.3 pg/ml for IL-17a, 1.6 pg/ml for G-CSF, 0.2 pg/ml for granulocyte-macrophage colony-stimulating factor, 0.8 pg/ml for IFN-γ, 1.2 pg/ml for tumor necrosis factor, 1.2 pg/ml for IL-8, 0.002 pg/ml for CCL-5, 1.3 pg/ml for monocyte chemoattractant protein -1, and 0.5 pg/ml for inducible protein-10.
Statistics
Values are expressed as percentages for categorical variables and as mean and SE or median and interquartile range for continuous variables. For variables that were not normally distributed, the Kruskal–Wallis test was performed to compare continuous variables, followed by Mann–Whitney U-tests for individual comparisons. χ2 tests were performed to compare categorical data. A two-sided value of P < 0.05 was considered statistically significant.
A receiver operating characteristic curve was plotted for those markers that were statistically different between severe and mild RSV infection. An optimal cutoff value for individual markers was then determined with a sensitivity approaching 100% and specificity >85%. If the diagnostic marker was unable to meet the above-mentioned criteria, the optimal cutoff value was adjusted so that both sensitivity and specificity approached 75%. With these optimal cutoff values, the sensitivity, specificity, and positive and negative predictive values of these markers or combination of markers were calculated. All statistical tests were performed by SPSS (Release 16; SPSS, Chicago, IL).
Statement of Financial Support
The study was financially supported by the VIRGO consortium, an Innovative Cluster approved by the Netherlands Genomics Initiative and partially funded by the Dutch Government (BSIK 03012), The Netherlands.
Disclosure
The authors declared no conflict of interest.
Supplementary information
Acknowledgements
The authors thank the children and their parents for participating in this study, and the nurses and medical staff of the Department of Pediatrics at the Radboud University Medical Center and Canisius Wilhelmina Hospital for assistance in obtaining clinical samples. The authors are grateful to Elles Simonetti and Kim van der Weerd for their contribution in the laboratory. In addition, the authors thank Eva Voorbrood and Paul Ruijs from the Laboratory of Hematology at the Radboud University Medical Center for counting the blood smears.
References
- 1.Black CP. Systematic review of the biology and medical management of respiratory syncytial virus infection. Respir Care. 2003;48:209–31; discussion 231–3. [PubMed] [Google Scholar]
- 2.Boyce TG, Mellen BG, Mitchel EF, Jr, Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in medicaid. J Pediatr. 2000;137:865–70. doi: 10.1067/mpd.2000.110531. [DOI] [PubMed] [Google Scholar]
- 3.Berger TM, Aebi C, Duppenthaler A, Stocker M. Prospective population-based study of RSV-related intermediate care and intensive care unit admissions in Switzerland over a 4-year period (2001-2005) Infection. 2009;37:109–16. doi: 10.1007/s15010-008-8130-z. [DOI] [PubMed] [Google Scholar]
- 4.Henderson J, Hilliard TN, Sherriff A, Stalker D, Al Shammari N, Thomas HM. Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol. 2005;16:386–92. doi: 10.1111/j.1399-3038.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 5.Nicholson KG, McNally T, Silverman M, Simons P, Stockton JD, Zambon MC. Rates of hospitalisation for influenza, respiratory syncytial virus and human metapneumovirus among infants and young children. Vaccine. 2006;24:102–8. doi: 10.1016/j.vaccine.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Purcell K, Fergie J. Driscoll Children’s Hospital respiratory syncytial virus database: risk factors, treatment and hospital course in 3308 infants and young children, 1991 to 2002. Pediatr Infect Dis J. 2004;23:418–23. doi: 10.1097/01.inf.0000126273.27123.33. [DOI] [PubMed] [Google Scholar]
- 7.Prais D, Danino D, Schonfeld T, Amir J. Impact of palivizumab on admission to the ICU for respiratory syncytial virus bronchiolitis: a national survey. Chest. 2005;128:2765–71. doi: 10.1378/chest.128.4.2765. [DOI] [PubMed] [Google Scholar]
- 8.Mansbach JM, Clark S, Christopher NC. Prospective multicenter study of bronchiolitis: predicting safe discharges from the emergency department. Pediatrics. 2008;121:680–8. doi: 10.1542/peds.2007-1418. [DOI] [PubMed] [Google Scholar]
- 9.Roback MG, Baskin MN. Failure of oxygen saturation and clinical assessment to predict which patients with bronchiolitis discharged from the emergency department will return requiring admission. Pediatr Emerg Care. 1997;13:9–11. doi: 10.1097/00006565-199702000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Norwood A, Mansbach JM, Clark S, Waseem M, Camargo CA., Jr Prospective multicenter study of bronchiolitis: predictors of an unscheduled visit after discharge from the emergency department. Acad Emerg Med. 2010;17:376–82. doi: 10.1111/j.1553-2712.2010.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parker MJ, Allen U, Stephens D, Lalani A, Schuh S. Predictors of major intervention in infants with bronchiolitis. Pediatr Pulmonol. 2009;44:358–63. doi: 10.1002/ppul.21010. [DOI] [PubMed] [Google Scholar]
- 12.Walsh P, Rothenberg SJ, O’Doherty S, Hoey H, Healy R. A validated clinical model to predict the need for admission and length of stay in children with acute bronchiolitis. Eur J Emerg Med. 2004;11:265–72. doi: 10.1097/00063110-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Larrañaga CL, Ampuero SL, Luchsinger VF. Impaired immune response in severe human lower tract respiratory infection by respiratory syncytial virus. Pediatr Infect Dis J. 2009;28:867–73. doi: 10.1097/INF.0b013e3181a3ea71. [DOI] [PubMed] [Google Scholar]
- 14.Brandenburg AH, Kleinjan A, van Het Land B. Type 1-like immune response is found in children with respiratory syncytial virus infection regardless of clinical severity. J Med Virol. 2000;62:267–77. doi: 10.1002/1096-9071(200010)62:2<267::AID-JMV20>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 15.Bont L, Heijnen CJ, Kavelaars A. Peripheral blood cytokine responses and disease severity in respiratory syncytial virus bronchiolitis. Eur Respir J. 1999;14:144–9. doi: 10.1034/j.1399-3003.1999.14a24.x. [DOI] [PubMed] [Google Scholar]
- 16.Hassan MA, Eldin AM, Ahmed MM. T – helper2 /T – helper1 imbalance in respiratory syncytial virus bronchiolitis in relation to disease severity and outcome. Egypt J Immunol. 2008;15:153–60. [PubMed] [Google Scholar]
- 17.Maródi L. Neonatal innate immunity to infectious agents. Infect Immun. 2006;74:1999–2006. doi: 10.1128/IAI.74.4.1999-2006.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinto RA, Arredondo SM, Bono MR, Gaggero AA, Díaz PV. T helper 1/T helper 2 cytokine imbalance in respiratory syncytial virus infection is associated with increased endogenous plasma cortisol. Pediatrics. 2006;117:e878–86. doi: 10.1542/peds.2005-2119. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell DR, Carrington D. Peripheral blood lymphopenia and neutrophilia in children with severe respiratory syncytial virus disease. Pediatr Pulmonol. 2002;34:128–30. doi: 10.1002/ppul.10140. [DOI] [PubMed] [Google Scholar]
- 20.Roe MF, Bloxham DM, White DK, Ross-Russell RI, Tasker RT, O’Donnell DR. Lymphocyte apoptosis in acute respiratory syncytial virus bronchiolitis. Clin Exp Immunol. 2004;137:139–45. doi: 10.1111/j.1365-2249.2004.02512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Vries E, de Bruin-Versteeg S, Comans-Bitter WM. Longitudinal survey of lymphocyte subpopulations in the first year of life. Pediatr Res. 2000;47(4 Pt 1):528–37. doi: 10.1203/00006450-200004000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Comans-Bitter WM, de Groot R, van den Beemd R. Immunophenotyping of blood lymphocytes in childhood. Reference values for lymphocyte subpopulations. J Pediatr. 1997;130:388–93. doi: 10.1016/S0022-3476(97)70200-2. [DOI] [PubMed] [Google Scholar]
- 23.De Weerd W, Twilhaar WN, Kimpen JL. T cell subset analysis in peripheral blood of children with RSV bronchiolitis. Scand J Infect Dis. 1998;30:77–80. doi: 10.1080/003655498750002349. [DOI] [PubMed] [Google Scholar]
- 24.Sheeran P, Jafri H, Carubelli C. Elevated cytokine concentrations in the nasopharyngeal and tracheal secretions of children with respiratory syncytial virus disease. Pediatr Infect Dis J. 1999;18:115–22. doi: 10.1097/00006454-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Bonville CA, Rosenberg HF, Domachowske JB. Macrophage inflammatory protein-1alpha and RANTES are present in nasal secretions during ongoing upper respiratory tract infection. Pediatr Allergy Immunol. 1999;10:39–44. doi: 10.1034/j.1399-3038.1999.101005.x. [DOI] [PubMed] [Google Scholar]
- 26.Tian M, Liu F, Wen GY, Shi SY, Chen RH, Zhao DY. Effect of variation in RANTES promoter on serum RANTES levels and risk of recurrent wheezing after RSV bronchiolitis in children from Han, Southern China. Eur J Pediatr. 2009;168:963–7. doi: 10.1007/s00431-008-0870-3. [DOI] [PubMed] [Google Scholar]
- 27.Huang JL, Huang J, Duan ZH. Th2 predominance and CD8+ memory T cell depletion in patients with severe acute respiratory syndrome. Microbes Infect. 2005;7:427–36. doi: 10.1016/j.micinf.2004.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawasaki Y, Hosoya M, Kanno H, Suzuki H. Serum regulated upon activation, normal T cell expressed and presumably secreted concentrations and eosinophils in respiratory syncytial virus infection. Pediatr Int. 2006;48:257–60. doi: 10.1111/j.1442-200X.2006.02199.x. [DOI] [PubMed] [Google Scholar]
- 29.Culley FJ, Pennycook AM, Tregoning JS. Role of CCL5 (RANTES) in viral lung disease. J Virol. 2006;80:8151–7. doi: 10.1128/JVI.00496-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hotchkiss RS, Opal S. Immunotherapy for sepsis–a new approach against an ancient foe. N Engl J Med. 2010;363:87–9. doi: 10.1056/NEJMcibr1004371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Said EA, Dupuy FP, Trautmann L. Programmed death-1-induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection. Nat Med. 2010;16:452–9. doi: 10.1038/nm.2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Avota E, Gassert E, Schneider-Schaulies S. Measles virus-induced immunosuppression: from effectors to mechanisms. Med Microbiol Immunol. 2010;199:227–37. doi: 10.1007/s00430-010-0152-3. [DOI] [PubMed] [Google Scholar]
- 33.Malamitsi-Puchner A, Sarandakou A, Tziotis J, Economou E, Protonotariou E, Rigopoulou O. Chemokines Rantes and interleukin-8 in the perinatal period: changes in serum concentrations. Am J Perinatol. 2004;21:235–40. doi: 10.1055/s-2004-828611. [DOI] [PubMed] [Google Scholar]
- 34.Sarafidis K, Diamanti E, Taparkou A, Tzimouli V, Drossou-Agakidou V, Kanakoudi-Tsakalidou F. Plasma RANTES increase during the first month of life independently of the feeding mode. Eur J Pediatr. 2007;166:819–23. doi: 10.1007/s00431-006-0329-3. [DOI] [PubMed] [Google Scholar]
- 35.Carroll KN, Wu P, Gebretsadik T. The severity-dependent relationship of infant bronchiolitis on the risk and morbidity of early childhood asthma. J Allergy Clin Immunol. 2009;123:1055–61, 1061.e1. doi: 10.1016/j.jaci.2009.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smyth RL, Openshaw PJ . Bronchiolitis. Lancet 2006;368:312–22. [DOI] [PubMed]
- 37.Hogatt J . Personalized medicine—trends in molecular diagnostics: exponential growth expected in the next ten years. Mol Diagn Ther 2011;15:53–5. [DOI] [PubMed]
- 38.Quinn B. Payers and the assessment of clinical utility for companion diagnostics. Clin Pharmacol Ther. 2010;88:751–4. doi: 10.1038/clpt.2010.234. [DOI] [PubMed] [Google Scholar]
- 39.Templeton KE, Scheltinga SA, Beersma MF, Kroes AC, Claas EC. Rapid and sensitive method using multiplex real-time PCR for diagnosis of infections by influenza a and influenza B viruses, respiratory syncytial virus, and parainfluenza viruses 1, 2, 3, and 4. J Clin Microbiol. 2004;42:1564–9. doi: 10.1128/JCM.42.4.1564-1569.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


