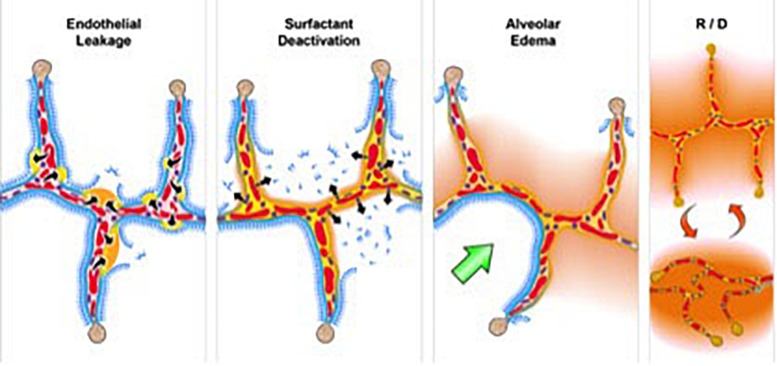
FIGURE 3.
The pathologic tetrad of acute respiratory distress syndrome (ARDS). Alveolar walls contain pulmonary capillaries (red circles) and are lined with a liquid hypophase (blue layer inside each alveolus), with an intact pulmonary surfactant layer (small blue ball with tail) layered on the hypophase. The systemic inflammatory response syndrome (SIRS) secondary to sepsis, trauma, burns, pneumonia, and so on increases pulmonary capillary permeability. Endothelial leakage: increased microvascular permeability allowing pulmonary edema to move into the alveolus (black arrows and tan edema blebs) (Martin and Brigham, 2012). Surfactant deactivation: the continuous layer of pulmonary surfactant molecules is disrupted as the edema blebs expand causing surfactant deactivation (surfactant sluffing off into the alveolar space). Edema usurping surfactant from the alveolar surface, the proteins in the edema fluid deactivating the surfactant (Taeusch et al., 2005), and improper mechanical ventilation (Albert, 2012) causing further surfactant disruption all combine to exacerbate surfactant loss. Alveolar edema: increased capillary permeability (Martin and Brigham, 2012) and high alveolar surface tension combine to flood alveoli with edema fluid (tan). Recruitment/derecruitment (R/D): loss of surfactant function results in increased alveolar surface tension causing loss of alveolar stability (i.e., causing alveolar R/D with each breath). Alveoli in the top frame of R/D are fully inflated but collapse during expiration in the bottom R/D frame. Alveolar R/D, known as atelectrauma, is another key VILI mechanism (Cressoni et al., 2017). Stress-focus: edema-filled or collapsed alveoli adjacent to air-filled alveoli create a stress-focus causing the alveolar wall to bend toward the fluid-filled alveolus (green arrow), which can cause stress failure at the alveolar wall (Perlman et al., 2011). Stress-focus is another key mechanism of VILI (Perlman et al., 2011; Chen et al., 2014; Makiyama et al., 2014; Retamal et al., 2014). Thus, the pathologic tetrad sets up a vicious cycle of high microvascular permeability → edema → surfactant deactivation → high alveolar surface tension → more edema → alveolar R/D → further increase in microvascular permeability → severe ARDS (Nieman and Bredenberg, 1985).