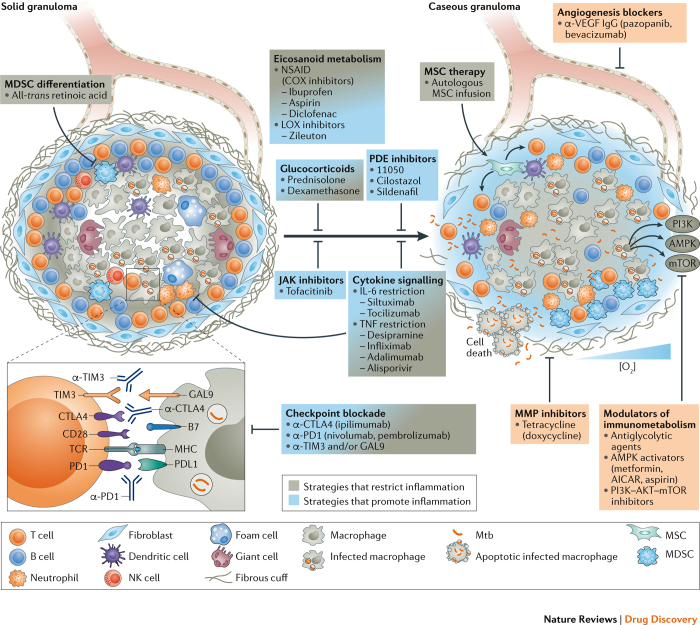
Figure 3. HDTs that target inflammatory responses and granulomas in TB.
During latent tuberculosis (TB), lung lesions may be absent or may present as solid, eventually fibrotic and mineralized granulomas. During active TB, granulomas progress towards necrosis and caseation, leading to cavitation and bacterial expectoration. Such lesions contain Mycobacterium tuberculosis (Mtb) in distinct metabolic and replicative stages: replicating and metabolically active bacilli in caseous granulomas; and non-replicative, dormant bacteria in the hypoxic environment of solid granulomas. In a single patient, different granuloma types coexist that harbour Mtb with an active or a dormant phenotype. Hence, strategies to restrict or to promote inflammation are envisaged as potential host-directed therapy (HDT) for TB. The selection of a particular HDT depends on the rationale for applying it as stand-alone treatment, for example, to limit exacerbated tissue damage, or as an adjunct to canonical TB therapy to promote inflammation and facilitate killing of actively replicating Mtb. Interference with arachidonic acid (AA) metabolism, which generates both pro- and anti-inflammatory metabolites and which also modulates patterns of cell death in infected cells, and interference with cytokine signalling and selected cellular therapies, such as the maturation of myeloid-derived suppressor cells (MDSCs) and the infusion of mesenchymal stem cells (MSCs), can correct exacerbated inflammation. The amendment of immune suppression by checkpoint blockade can restrict inflammation by correcting levels of protective interferon-γ (IFNγ); however, this may facilitate hyper-inflammation once pathological levels of the cytokine are achieved. Drugs interfering with such mechanisms limit immunopathology and help to preserve tissue functionality. Immune-suppressive drugs, notably glucocorticoids and biologics, besides limiting life-threatening inflammation, reduce the local abundance of host-protective cytokines and thereby facilitate lesion caseation and promote the resuscitation of dormant Mtb. Metabolically active bacteria can be targeted by canonical TB chemotherapy. Limiting vasculogenesis restricts nutrient supply and access of Mtb-permissive cells to granulomas. Metformin, glycolytic agents and kinase inhibitors interfere with metabolic pathways activated under hypoxic conditions that support bacillary replication, and inhibition of matrix metalloproteinases (MMPs) limits collateral damage and Mtb spread. Boxes indicate drugs that interfere with angiogenesis, metabolic pathways and factors that promote tissue damage. AICAR, 5-aminoimidazole-4- carboxamide ribonucleotide; AMPK, 5′ adenosine monophosphate- activated protein kinase; COX, cyclooxygenase; CTLA4, cytotoxic T lymphocyte associated protein 4; GAL9, galectin 9; LOX, lipoxygenase; MHC, major histocompatibility complex; mTOR, mammalian target of rapamycin; NK, natural killer; NSAID, non-steroidal anti-inflammatory drug; PDE, phosphodiesterase; PD1, programmed cell death protein 1; PDL1, PD1 ligand 1; PI3K, phosphatidylinositol-4,5-bisphosphate 3-kinase; TCR, T cell receptor; TIM3, T cell immunoglobulin mucin receptor 3; TNF, tumour necrosis factor; VEGF, vascular endothelial growth factor.