Figure 4. Viruses and bacteria induce airway inflammation.
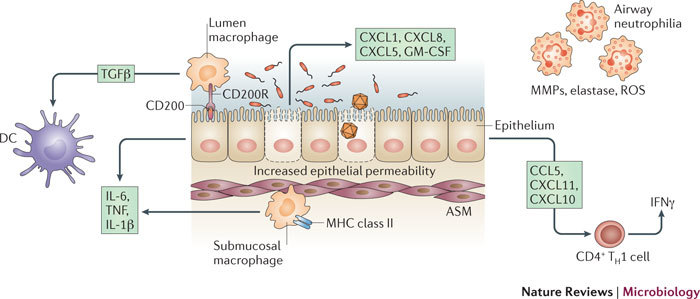
Bacterial and viral infections of the airways activate immune and structural cells, promoting inflammation and influencing responses to other pathogens, allergens and pollution. Infection of airway epithelium by both viruses and bacteria induces neutrophil chemokines (CXC-chemokine ligand 1 (CXCL1; also known as GROα), CXCL5 (also known as ENA78) and CXCL8 (also known as IL-8)), and T helper 1 (TH1) type chemokines (CC-chemokine ligand 5 (CCL5; also known as RANTES), CXCL10 (also known as IP10) and CXCL11 (also known as ITAC)), and increases epithelial permeability. Neutrophils secrete several mediators that can contribute to inflammation and the integrity of the airway, including matrix metalloproteinases (MMPs), elastase and reactive oxygen species (ROS). Epithelial cells normally express luminal CD200, which, when bound to its receptor, CD200R, on lumen macrophages, prevents the macrophage response to inflammatory stimuli. Lumen macrophages are normally inhibitory, as they produce transforming growth factor-β (TGFβ), which inhibits inflammatory airway dendritic cells (DCs). A higher epithelial permeability or epithelial damage as a result of infection allows the unrestrained submucosal macrophages access to the allergen and to other stimuli, and this can promote overzealous inflammation. Submucosal macrophages and epithelial cells are triggered by exposure to bacteria or viruses (and their products) to produce interleukin-1β (IL-1β), IL-6 and tumour necrosis factor (TNF), which promote inflammation. ASM, airway smooth muscle; GM-CSF, granulocyte–macrophage colony-stimulating factor; IFNγ, interferon-γ; MHC, major histocompatibility complex; TH1, T helper 1.
