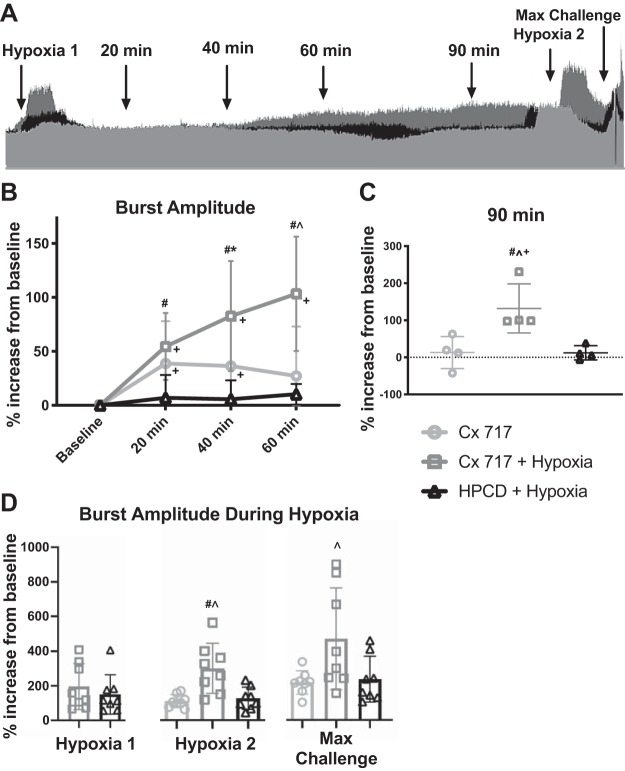
Fig. 4.
Pretreating with ampakine enables a single episode of hypoxia to trigger sustained facilitation of phrenic inspiratory burst amplitude. A: superimposed phrenic neurograms from each treatment group highlight the effect of CX717+ hypoxia (dark gray) on the amplitude of phrenic motor output compared with CX717alone (light gray) and 2-hydroxypropyl-β-cyclodextrin (HPCD) + hypoxia (black). Dotted line represents baseline amplitude. Arrows indicate points used for data analysis. B: average change in phrenic burst amplitude in the 3 experimental groups. Data from 90 min posttreatment, which were collected in a separate cohort, are shown in C. CX717 + hypoxia resulted in sustained increases in phrenic bursting that were 100% greater than baseline by 60 min. At the 90-min time point, average amplitude was significantly different in the CX717 + hypoxia group compared with the other groups and was significantly different from baseline. D: average change in burst amplitude from baseline during chemoreceptor challenge. Pretreatment with CX717 did not alter the amplitude of phrenic bursts during subsequent hypoxia (hypoxia 1) compared with the HPCD + hypoxia treatment group. After 60 min, the increase in burst amplitude during a second hypoxia challenge (hypoxia 2) as well as the maximal chemoreceptor challenge (max challenge) were elevated in the CX717+ hypoxia group. Individual data points are shown, and horizontal lines indicate means ± SD. #P < 0.05, significant difference between CX717 + hypoxia and HPCD + hypoxia. *P < 0.05, significant difference between CX717 and HPCD + hypoxia. ^P < 0.05, significant difference between CX717 and CX717 + hypoxia. +P < 0.05, significant difference compared with 0 (baseline).