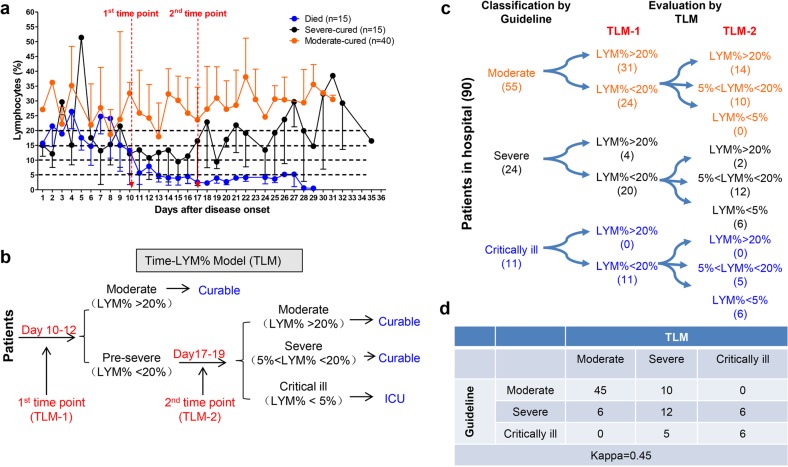
Fig. 1.
Establishment and validation of Time-LYM% model (TLM) in patients with COVID-19. a Dynamic changes of LYM% in the death cases (n = 15), severe-cured cases (n = 15), and moderate-cured cases (n = 40). Data are showen as means ± s.e.ms. Two cutoff time points of these three curves were set as 1st time point (day 10–12) and 2nd time point (day 17–19). b Description of TLM: 1st time point (TLM-1) and 2nd time point (TLM-2) are defined as day 10–12 and day 17–19 from symptom onset, respectively. The confirmed COVID-19 patients with LYM% > 20% at TLM-1 are classified as moderate type and the ones with LYM% < 20% at TLM-1 are suggested as pre-severe type, which need to be further distinguished at TLM-2. If LYM% > 20% at TLM-2, those pre-severe patients are reclassified as moderate. If 5% < LYM% < 20% at TLM-2, the pre-severe patients are indeed typed as severe. If LYM% < 5% at TLM-2, those patients are suggested as critically ill. The moderate and severe types are curable, while the critically ill types need intensive care has a poor prognosis. c Ninety COVID-19 patients were currently hospitalized in light of the classification criteria of the New Coronavirus Pneumonia Diagnosis Program (5th edition): 55 patients with moderate type, 24 patients with severe type and 11 patients with critically ill type. At TLM-1, LYM% in 24 out of 55 moderate cases was lower than 20%; At TLM-2, LYM% in all 24 patients was above 5%, indicating that these patients would be curable. Regarding other 24 patients with severe symptoms, LYM% at TLM-1 was lower than 20% in 20 out of 24 cases. LYM% at TLM-2 in 6 cases was <5%, indicating a poor prognosis. In 11 out of 11 critically ill patients, LYM% at TLM-1 was lower than 20%. LYM% at TLM-2 in six cases was lower than 5%, suggesting a poor prognosis. d The consistency between Guideline and TLM-based disease classification in c was tested using kappa statistic. Kappa = 0.48; P < 0.005