Abstract
Background:
Delay in seeking medical treatment for suspected acute coronary syndrome can lead to negative patient outcomes.
Objective:
Our aim was to evaluate the prevalence and predictors of delay in seeking care in high-risk chest pain patients with or without acute coronary syndrome (ACS).
Methods:
This was a secondary analysis of an observational cohort study of patients transported by Emergency Medical Services for a chief complaint of chest pain. Important demographic and clinical characteristics were extracted from electronic health records. Two independent reviewers adjudicated the presence of ACS. Logistic regression was used to model the predictors of delay in seeking care.
Results:
The final sample included 743 patients (99% non-Hispanic). Overall, 24% presented > 12 h from onset of symptoms. Among those with ACS (n = 115), 14% presented > 12 h after onset of symptoms. Race, smoking, diabetes, and related symptoms were associated with delayed seeking behavior. In multivariate analysis, non-Caucasian race (black or others) was the only independent predictor of > 12 h delay in seeking care (odds ratio 1.4; 95% confidence interval 1.0–1.9).
Conclusions:
One in four patients with chest pain, including 14% of those with ACS, wait more than 12 h before seeking care. Compared to non-blacks, black patients are 40% more likely to delay seeking care > 12 h.
Keywords: acute coronary syndrome, chest pain, emergency care, delay
INTRODUCTION
Heart disease continues to be the leading cause of death worldwide (1). Chest pain is a well-known symptom of a potential acute myocardial infarction. Many American Heart Association (AHA) campaigns (ie, Get with the Guidelines, Go Red) have been well established and publicized for several years and have targeted United States citizens to recognize the onset of chest pain as a potential life-threatening situation. Many studies have explored various interventions to change delayed seeking behavior, however, wait times from onset of symptoms continue to be greater than the gold standard of 2 h (1–4). In those with acute coronary syndrome (ACS), it is estimated that the risk of 1-year mortality is increased by 7.5% for each 30 min of delay, diminishing the potential benefit of revascularization with percutaneous coronary intervention (PCI) (5). As such, current AHA and European Society of Cardiology guidelines have advised to bypass general practitioners altogether and to refer all patients with new or recently changed chest complaints to the hospital to prevent delay in seeking immediate medical attention (5,6). Although this referral to the hospital may cause additional strain on the emergency department (ED), the benefits outweigh the potential risk of missing an ACS event.
Current practice guidelines recommend primary PCI or fibrinolytic therapy to patients with ST elevation ACS within 90 min of first medical contact; given that the onset of symptoms is ≤ 12 h (7). Although tremendous effort has been made nationwide to achieve this 90-min treatment window (ie, prehospital 12-lead electrocardiogram with expedited activation of catheterization laboratory), full understanding of the prevalence and predictors of delayed seeking behavior remains controversial (8–12). Literature over the last decade primarily suggests that women, young adults, and those with lower education and socioeconomic status tend to wait longer before seeking care for chest pain compared to their counterparts (13–17). However, most of these studies exclusively sampled patients hospitalized with ACS, making it difficult to compare the value of these predictors to patients with similar profiles but without ACS. Accordingly, we sought to define the prevalence and predictors of delay in seeking emergency care in patients complaining of chest pain with or without ACS.
METHODS
Design, Sample, and Setting
We conducted a secondary analysis of the EMPIRE (Electrocardiogram Methods for the Prompt Identification of Coronary Events) study (18). Our Institutional Review Board approved this prospective, observational cohort study of consecutive non-traumatic chest pain patients that call 9-1-1 for the chief complaint of chest pain. Enrolled patients were transported via ambulance by Emergency Medical Services (EMS) to one of three participating tertiary care centers with 24-h cardiac catheterization centers. This EMS agency is a municipal EMS agency that serves an urban city setting, with a mean transport time of 32 min (EMS arrival to scene to hospital arrival). The agency responded to 9-1-1 calls with a dual paramedic team during the study period.
EMPIRE prospectively enrolled patients that were transported to the hospital for the chief complaint of chest pain or equivalent. Inclusion criteria were as follows: 1) age ≥ 18 years old; 2) present with a chief complaint of non-traumatic chest pain or other atypical, suspicious symptoms (ie, shortness of breath); and 3) prehospital electrocardiogram (ECG) performed and transmitted to a medical command center. There were no restrictions to sex or race. For this secondary analysis, we enrolled all available patients from the first study cohort that enrolled patients transported between May 2013 and August 2014 (n = 750).
Data Collection
Prehospital and in-hospital electronic health records were manually examined by independent reviewers to extract pertinent clinical data. Baseline demographics and clinical characteristics for each patient (ie, age, sex, race, income, medical history, and medications) were collected from charts as per a predefined data coding scheme that has been described in detail previously (18). The patient incomes were obtained from public records of mean income according to the dispatch ZIP code location of the 9-1-1 call. Low income was defined as yearly salary < $44,999 and middle income was defined as $45,000–$139,999.
Onset of Symptoms
First medical contact time was recorded as scene arrival time for paramedics. ED arrival time was when the patient was entered into the electronic health record and the patient chart was activated. We used date and time stamps of 9-1-1 call and available EMS/physician narrative notes to determine the time from onset of symptoms to patient’s decision to seek care. If a discrepancy occurred, both the physician note and EMS charting was examined and compared, resulting in expert consensus of onset time. For example, if EMS documented on scene that chest pain started 2 h earlier, then delay in seeking care for that patient was coded as 2 h. However, if the physician note stated that chest pain started 2 h earlier, but the lag in time between ED arrival and 9-1-1 call was 45 min, then delay in seeking care for that patient was coded as1.25 h. Given that current guidelines recommend against reperfusion if there is 12 h delay from symptom onset, then delay ≤ 12 h vs. > 12 h was used as the primary dependent variable in logistic regression model (7).
Adjudication of ACS
ACS was defined per the AHA/American College of Cardiology Universal Definition criteria as: 1) elevated cardiac troponin (≥99th percentile of normal reference), 2) ECG indicative of ischemic changes, 3) echocardiographic images evident with new loss of viable myocardium or new regional wall motion abnormalities, or 4) coronary angiographic or nuclear imaging demonstrating > 70% stenosis of a major coronary artery with or without treatment (7,19). Two independent reviewers examined available electronic health and diagnostic records to adjudicate the presence of ACS. Disagreement was resolved by a third reviewer.
Statistical Analysis
All statistical analyses were performed on SPSS ®, version 25 (IBM, Armonk, NY). We presented continuous variables as mean ± standard deviation or as median (interquartile range) and tested with a Student’s t-test or the Mann-Whitney U test. We presented categorical variables as percentages and tested with χ 2. Predictors of delay significant at p < 0.10 in a univariable logistic regression were entered in a multivariable logistic regression model with backward selection. Significance level was set at 0.05 for two-sided hypothesis testing.
RESULTS
We included 743 (median age 58 years [interquartile range 24 years], 43% female, 99% non-Hispanic, and 40% black) in the final sample after excluding 7 patients with missing time metrics. Figure 1 shows the distribution of delay in seeking emergency care in this sample. Overall, 54% of patients sought emergent care within the 2-h window of onset of symptoms; 22% waited > 2 h, but sought emergent care within the 12-h window; and 24% sought care after 12 h of onset of symptoms. Among those with confirmed ACS (n = 115), 16 cases (14%) presented 12 h after the onset of symptoms.
Figure 1.
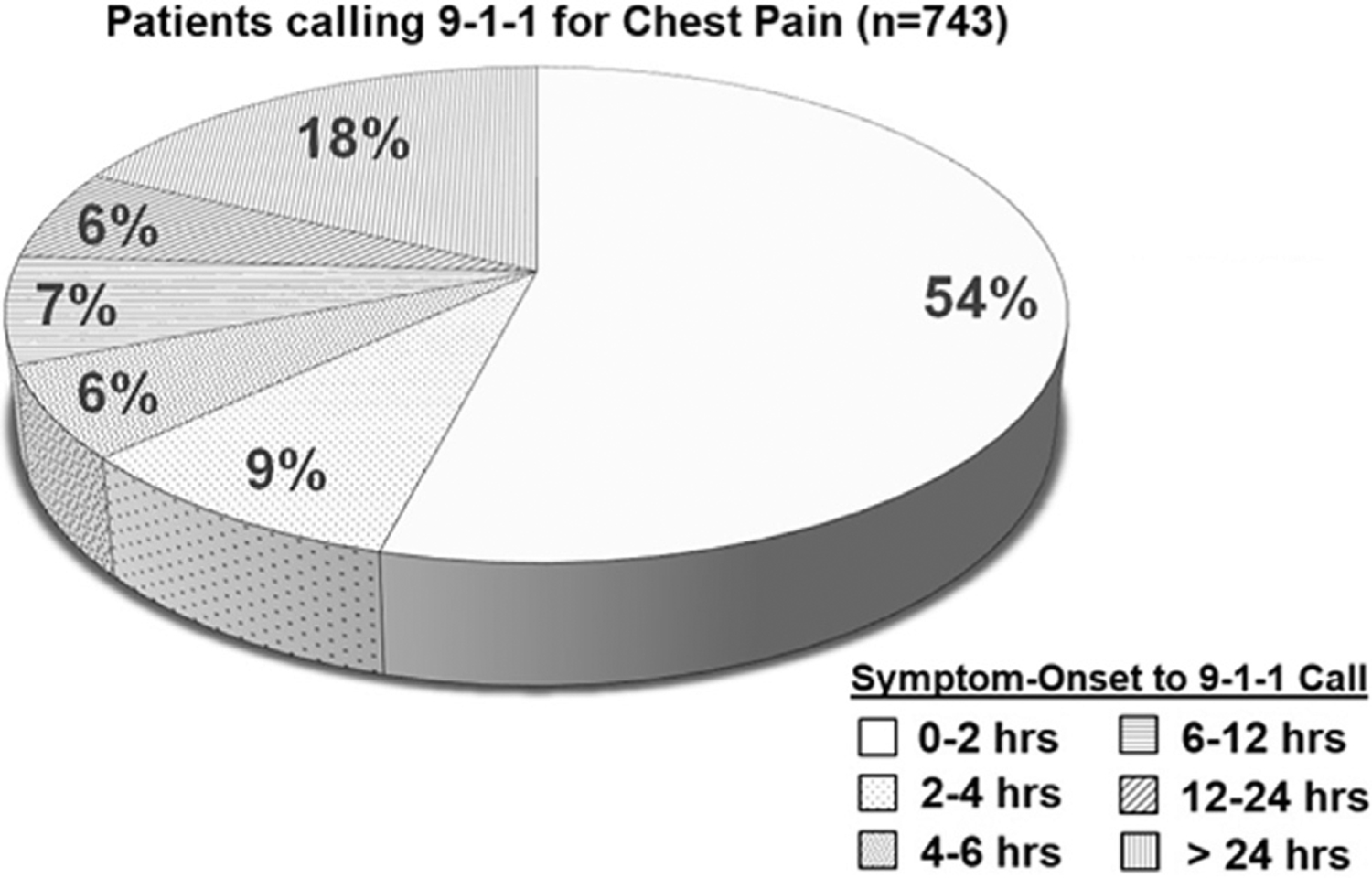
Patients calling 9-1-1 for chest pain (n = 743).
Table 1 compares the baseline demographic and clinical characteristics of patients who presented ≤ 12 h or > 12 h from onset of symptoms. Race categories were Caucasian, black, and other. Race analysis compared black and non-black race (ie, American Indian, Asian, and other) against Caucasian as the reference group. For average salary per year income categories, 3 patients had an income of < $20,000, and this sub-group was collapsed into one low-income category of < $44,999 group. There were 154 patients in the middle-income category (ie, $45,000–$139,999). No patients had an income > $139,999 per year. None of the EMS factors (ie, day of event, time of day of event) were significantly different between symptom-onset groups.
Table 1.
Demographic and Clinical Characteristics of Study Sample
| Symptom Onset to 9-1-1 Call | |||
|---|---|---|---|
| Characteristic | All Patients (n = 743) | 0–12 h (n = 565 [76%]) | > 12 h (n = 178 [24%]) |
| Sociodemographic characteristics | |||
| Age, years, median (IQR) | 72 (23) | 58 (24) | 56 (23) |
| Sex (male), n (%) | 427 (57) | 325 (58) | 102 (57) |
| Income class, n (%) | |||
| Low | 583 (79) | 441 (78) | 136 (76) |
| Middle | 154 (21) | 115 (20) | 38 (21) |
| Race, n (%) | |||
| Caucasian | 434 (58) | 338 (60) | 90 (51) |
| Black | 301 (40) | 219 (39) | 81 (45) |
| Other | 15 (2) | 8 (1) | 7 (4) |
| EMS factors | |||
| Day of event, n (%) | |||
| Weekday | 508 (68) | 382 (68) | 126 (71) |
| Weekend | 235 (32) | 183 (32) | 52 (29) |
| Time of event, n (%) | |||
| 12:00 am–6:00 am | 123 (17) | 96 (17) | 27 (15) |
| 6:00 am–12:00 pm | 210 (28) | 158 (28) | 52 (29) |
| 12:00 pm–6:00 pm | 224 (30) | 164 (29) | 60 (34) |
| 6:00 pm–12:00 am | 186 (25) | 147 (26) | 39 (22) |
| Speed of EMS response (9-1-1 call to EMS arrival to scene), min, median (IQR) | 12.1 (11.6–12.5) | 11.8 (11.3–12.0) | 12.9 (11.9–14.0) |
| Duration of transport (EMS arrival to scene to hospital arrival), min, median (IQR) | 33.7 (32.6–34.9) | 33.9 (32.6–35.2) | 32.9 (31.4–34.5) |
| ACS risk factors, n (%) | |||
| Obesity (body mass index > 30) | 285 (38) | 211 (38) | 74 (42) |
| Ever smoked | 434 (58) | 324 (57) | 110 (62) |
| Hypertension | 519 (70) | 398 (71) | 119 (68) |
| Diabetes mellitus | 196 (26) | 142 (25) | 54 (31) |
| Hyperlipidemia | 258 (35) | 196 (35) | 62 (35) |
| Coronary artery disease | 248 (33) | 190 (34) | 58 (33) |
| History of myocardial infarction | 205 (28) | 156 (28) | 49 (28) |
| Known heart failure | 130 (18) | 95 (17) | 35 (20) |
| Prior PCI or CABG | 207 (28) | 159 (28) | 48 (27) |
| Chief complaint, n (%) | |||
| Chest pressure | 642 (87) | 492 (87) | 150 (85) |
| Shortness of breathing | 215 (29) | 165 (29) | 50 (28) |
| Heart rhythm abnormality | 124 (17) | 101 (18) | 23 (13) |
| Atypical symptoms | 53 (7) | 44 (8) | 9 (5) |
| Prehospital vital signs, mean ± SD | |||
| Heart rate (beats/min) | 91 ± 30 | 91 ± 31 | 89 ± 26 |
| Respiratory rate (breaths/min) | 18±4 | 18 ± 3 | 19 ± 7 |
| Systolic blood pressure (mm Hg) | 147 ± 31 | 146 ± 32 | 148 ± 29 |
| Diastolic blood pressure (mm Hg) | 87 ± 19 | 87 ± 19 | 86 ± 19 |
| Oxygen saturation (%) | 97 ± 7 | 98 ± 66 | 97 ± 8 |
ACS = acute coronary syndrome; CABG = coronary artery bypass grafting; EMS = emergency medical services; IQR = interquartile range; PCI = percutaneous coronary intervention.
In univariate analysis, black race (odds ratio [OR] 1.3; 95% confidence interval [CI] 1.0–1.9), other race (OR 3.3; 95% CI 1.2–9.3), smoking history (OR 1.6; 95% CI 1.0–2.5), diabetes mellitus (OR 1.3; 95% CI 0.9–1.9), shortness of breath (OR 1.5; 95% CI 0.9–2.7), atypical symptoms (OR 1.6; 95% CI 0.8–3.3), and heart rhythm abnormalities (OR 0.7; 95% CI 0.4–1.1) were associated (p < 0.10) with more than a 12-h delay in seeking emergent care (see Table 2). However, in multi variable analysis, non-Caucasian race was the only independent predictor of more than a 12-h delay in seeking emergent care for chest pain (OR 1.4; 95% CI 1.0–1.9 for blacks and 2.7; 95% CI 1.2–9.4 for others).
Table 2.
Univariate and Multivariate Predictors of Delay in Seeking Care
| Symptom Onset to 9-1-1 Call > 12 h | ||
|---|---|---|
| Variables | Univariate, OR (95% CI) | Multivariate, OR (95% CI) |
| Sociodemographic characteristics | ||
| Age (per 10-year increment) | NS | — |
| Male sex | NS | — |
| Race | ||
| Caucasian | ref | ref |
| Black | 1.3 (1.0–1.9) | 1.4 (1.0–1.9) |
| Other | 3.3 (1.2–9.3) | 2.7 (1.1–9.4) |
| Income class (low vs. middle) | NS | — |
| EMS factors | ||
| Day of event (weekday vs. weekend) | NS | — |
| Time of day of event | NS | — |
| Speed of EMS response (9-1-1 call to EMS arrival to scene) | NS | — |
| EMS transport duration (EMS arrival to scene to hospital arrival) | NS | — |
| ACS risk factors | ||
| Obesity (body mass index > 30) | NS | — |
| Ever smoked | 1.6 (1.0–2.5) | NS |
| Hypertension | NS | — |
| Diabetes mellitus | 1.3 (0.9–1.9) | NS |
| Hyperlipidemia | NS | — |
| Coronary artery disease | NS | — |
| History of myocardial infarction | NS | — |
| Diagnosed heart failure | NS | — |
| Prior PCI or CABG | NS | — |
| Chief complaint | ||
| Chest pressure | NS | — |
| Shortness of breath | 1.5 (0.9–2.7) | NS |
| Heart rhythm abnormality | 0.7 (0.4–1.1) | NS |
| Atypical symptoms | 1.6 (0.8–3.3) | NS |
| Prehospital vital signs | ||
| Heart rate (beats/min) | NS | — |
| Respiratory rate (breaths/min) | NS | — |
| Systolic blood pressure (mm Hg) | NS | — |
| Diastolic blood pressure (mm Hg) | NS | — |
| Oxygen saturation (%) | NS | — |
ACS = acute coronary syndrome; CABG = coronary artery bypass grafting; CI = confidence interval; EMS = Emergency Medical Services; NS = not significant; OR = odds ratio; PCI = percutaneous cardiac intervention.
DISCUSSION
In this study, we sought to evaluate the prevalence and predictors of delay in seeking emergent care in chest pain patients with or without ACS. We found that 1 in 4 patients, including 14% of those with confirmed ACS, waited > 12 h before seeking emergency care. Race was the only independent predictor of this behavior. Even after adjusting for all factors, compared to non-Caucasians, black patients were 40% more likely to delay seeking care > 12 h. This is one of a few studies focusing on high-risk chest pain patients transported by EMS, which included a representative sample of both ACS cases and non-ACS controls.
Prevalence of Delay in Seeking Care
Our findings indicate that approximately 25% of overall chest pain patients and 14% of ACS cases present 12 h after the onset of symptoms. Previous studies reported similar prevalence rates (ie, 18–33%) (13,20). However, it is worth noting that delay has been defined differently throughout literature. For instance, a recent prospective study by Zègre-Hemsey et al. examined delay > 3 h in a cohort of 590 non-ACS controls and 474 ACS cases (21). They found that 63% of non-ACS patients and 49% of ACS patients had a delayed presentation > 3 h(21). When compared to our study, we found an overall prevalence of > 2 h delay in 46% of patients in our cohort (Figure 1). Some studies have reported even larger prevalence rates.
Studies that investigate delay time in ST-elevated myocardial infarction (STEMI) patients only focus on different delay durations. The prevalence of delay varied in these patients according to time. For instance, it has been reported that the majority of STEMI patients (59%) presented within 6 h of symptom onset and only 25% of patients waited > 60 min (22,23). In another study, it has been shown that up to 33% of STEMI patients would wait > 12 h to seek medical care (20). Many other studies just simply reported the average time of delay (in minutes) (24–26). Compared to our data, we found that only 14% of ACS patients waited for > 12 h. It is worth noting that we did not stratify this group based on acute MI subtype due to sample size issues. In fact, previous studies suggest no difference among non-STEMI, unstable angina, and non-ACS patients in terms of prehospital delay in seeking care (21,27,28). It is important that the prevalent delay in presentation in ACS patients raises significant concerns; time from symptom onset to reperfusion therapy has been associated with increased infarct size and mortality (5,13). Improving patient education and knowledge of what constitutes a cardiac event is an ongoing educational target to address this important concern.
Predictors of Delay in Seeking Care
Prehospital barriers to delay continue to be a problem, despite many public campaigns and initiatives to impact patients’ ability to understand the signs and symptoms of an ACS event. Our findings indicate that race was the only independent predictor of delay; black individuals were 40% more likely to delay seeking medical care > 12 h when compared to Caucasian and other race. This finding is congruent with current literature and continues to be a concern for optimizing medical care to impact morbidity and mortality in the treatment of ACS (29–32). A particular strength of our analysis was that we had a racially diverse and well-represented cohort, which is representative of an urban city.
Prehospital EMS factors have the potential to add to the perceived acuity of patients upon arrival to the scene. Our EMS system’s mean transport time was only 42 min. This transportation time includes at-home medical treatment, loading the patient in the ambulance, and traveling to the hospital. Our EMS agency’s average response time during the study period was 12 min compared to the national average of 7 min (33). None of the EMS factors were different between no delay and delay > 12 h (see Table 2).
Prehospital symptoms reported to EMS play a key role in wait time associated with seeking emergent care. In the literature, atypical symptoms such as shortness of breath or fatigue are associated with increased delay time and are well documented. These findings are also supported in our findings. This increase in wait time has been associated with a lack of knowledge of symptoms of a heart attack. Symptoms of heart rhythm abnormalities, such as palpitations, were found to decrease wait times in our cohort and may suggest recognition of urgency. On the contrary, age, sex, income category (ie, low and middle) and medical history did not predict delay in our cohort. Diabetes and smoking were associated with delay at the univariate level. There have been conflicting findings in literature regarding these variables over the last decade (13–17). For instance, many studies suggested female sex as a predictor of delay, which is frequently attributed to a lack of understanding of the severity of their symptoms (13,16,17,34). Other studies, however, have found no difference between sex and delayed presentation (35–38). Such discrepancy may be due to regional improved awareness of heart health for women in various clinical populations.
Strengths and Limitations
Our sample included a cohort of consecutive chest pain cases, giving a distribution of ACS and non-ACS events similar to that observed in real-world practice. Our data were demographically representative of the region with regard to sex and race. The single EMS agency allowed for a universal standardized electronic prehospital charting system. Additionally, there was universal electronic health record charting at all hospital destinations.
This study has few limitations. First, we used electronic health records to extract patients’ self-report for onset of symptoms, which might add inaccuracies due to patient recall bias. We used multiple sources to make sure we have the correct approximate time of onset of symptoms. The EMS dispatch location was used for patient income. There is a chance that this location may not have been the primary residence for the patient calling 9-1-1. Also, we were unable to examine education level in our sample. Lower education and socioeconomic status have been reported as significant predictors of delay in many populations.
CONCLUSIONS
In this urban, predominantly non-Hispanic sample, which represents racial diversity, 1 in 4 patients with chest pain, including 14% of those with ACS, waited > 12 h before seeking care. Race was the only independent predictor of this behavior. Compared to non-Caucasians, black patients were 40% more likely to delay seeking care that long. These findings have important clinical implications. We need to investigate and understand why this vulnerable patient population has delays in seeking emergency care. The patient’s perspective of seeking emergent care for chest pain could help decrease or eliminate barriers to timely medical care. These barriers to prehospital delay continue to be a problem and need to be addressed. The patient’s perspective to seeking care is complex and involves many variables. We need to continue education from various sources, such as public health campaigns and outpatient and in-hospital settings to emphasize urgency of chest pain symptoms. Additionally, educational interventions should potentially be designed to target underserved populations in urban settings. This vulnerable population may need specialized dedicated education, which may reduce the racial disparities observed in the care of chest pain patients.
Practice Implications
One in four patients in our study had prehospital delay. Patients who wait to seek medical treatment for ACS are at increased risk for another cardiac event, including death and readmission of heart failure up to 12 months after the initial presentation (25). With research supporting early recognition of ACS symptoms, prehospital delay continues to be the major contributor to increased morbidity and mortality in acute MI (39). Every 30-min delay increases the 1-year mortality risk by 7.5% (4). In cases of STEMI patients, patients with increased prehospital delay time may be ineligible for thrombolysis/PCI, which can potentially reduce mortality by up to 25–30% (7). Striving for improved patient outcomes, patient education must emphasize the potential consequences of prehospital delay of an ACS event. This is an important teaching opportunity of an urban community where 1 in 4 patients are not seeking medical care within the guideline recommended treatment window.
Unfortunately, patients of black race are 40% more likely to delay care. Future work needs to investigate why this group of patients tend to delay seeking care for acute chest pain, which can serve as an important opportunity to improve outcomes and reduce disparity in the care of the racial group. These research findings need to be validated in the future and a collaborative effort involving public health programs in the region need to be informed to target underserved minorities in urban communities to inform them of signs and symptoms of an ACS event.
ARTICLE SUMMARY.
-
Why is this topic important?
Delay in seeking medical treatment for suspected acute coronary syndrome can lead to negative patient outcomes, including increased morbidity and mortality.
-
What does this study attempt to show?
Delay in seeking emergent care continues to be a problem among chest pain patients in our cohort. Vulnerable populations in an urban setting continue to have barriers that increase delay in seeking emergency treatment for chest pain.
-
What are the key findings?
Race was the only independent predictor of delay in seeking emergent care for chest pain patients in this cohort. Blacks were 40% more likely to delay in seeking treatment for > 12 h compared to non-blacks. Age, sex, income, and medical history did not predict delay in seeking medical care.
-
How is patient care impacted?
One in four patients continues to have delay in seeking emergent care in our cohort. Delay in seeking medical care is associated with increased mortality. Potential acute myocardial infarction patients with increased delay may be ineligible for life-saving treatments. Future patient education needs to continue to emphasize the importance of seeking emergent care immediately for chest pain to reduce patient delay and potentially improve patient outcomes.
Acknowledgments
This study is supported by a grant from the National Institutes of Health, United States grant R01 HL 137761. SOF received support from the National Institute of Nursing Research of the National Institutes of Health, United States under award number T32NR008857 and the Robet Wood Johnson Foundation Future of Nursing Scholars program. The funding bodies played no part in the conception, design, analysis, or preparation of research outputs.
REFERENCES
- 1.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: a report from the American Heart Association. Circulation 2018;137(12):e67–492. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg RJ, Mooradd M, Gurwitz JH, et al. Impact of time to treatment with tissue plasminogen activator on morbidity and mortality following acute myocardial infarction (The second National Registry of Myocardial Infarction). Am J Cardiol 1998;82:259–64. [DOI] [PubMed] [Google Scholar]
- 3.Chareothatawee P, Gibbons RJ, Roberts RS, Christian TF, Burns R, Yusuf S. The impact of time to thrombolytic treatment on outcome in patients with acute myocardial infarction. For the CORE investigators (Collaborative Organization for RheothRx Evaluation). Heart 2000;84:142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004;109:1223–5. [DOI] [PubMed] [Google Scholar]
- 5.Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-Elevation Myocardial Infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2016;133:1135–47. [DOI] [PubMed] [Google Scholar]
- 6.Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119–77. [DOI] [PubMed] [Google Scholar]
- 7.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362–425. [DOI] [PubMed] [Google Scholar]
- 8.Morrison LJ, Brooks S, Sawadsky B, McDonald A, Verbeek PR. Prehospital 12-lead electrocardiography impact on acute myocardial infarction treatment times and mortality: a systematic review. Acad Emerg Med 2006;13:84–9. [DOI] [PubMed] [Google Scholar]
- 9.Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol 2009;53:161–6. [DOI] [PubMed] [Google Scholar]
- 10.Adams GL, Campbell PT, Adams JM, et al. Effectiveness of prehospital wireless transmission of electrocardiograms to a cardiologist via hand-held device for patients with acute myocardial infarction (from the Timely Intervention in Myocardial Emergency, NorthEast Experience [TIME-NE]). Am J Cardiol 2006;98:1160–4. [DOI] [PubMed] [Google Scholar]
- 11.Brainard AH, Raynovich W, Tandberg D, Bedrick EJ. The prehospital 12-lead electrocardiogram’s effect on time to initiation of reperfusion therapy: a systematic review and meta-analysis of existing literature. Am J Emerg Med 2005;23:351–6. [DOI] [PubMed] [Google Scholar]
- 12.Nam J, Caners K, Bowen JM, Welsford M, O’Reilly D. Systematic review and meta-analysis of the benefits of out-of-hospital 12-lead ECG and advance notification in ST-segment elevation myocardial infarction patients. Ann Emerg Med 2014;64:176–86. e1–e9. [DOI] [PubMed] [Google Scholar]
- 13.Ladwig KH, Meisinger C, Hymer H, et al. Sex and age specific time patterns and long term time trends of pre-hospital delay of patients presenting with acute ST-segment elevation myocardial infarction. Int J Cardiol 2011;152:350–5. [DOI] [PubMed] [Google Scholar]
- 14.Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention of a patient delay and emergency medical service use in acute coronary heart disease. JAMA 2000;284:60–7. [DOI] [PubMed] [Google Scholar]
- 15.Xie L, Huang S-F, Hu Y-Z. Factors influencing pre-hospital patient delay in patients with acute myocardial infarction. Chin Nursing Res 2015;2(2–3):75–9. [Google Scholar]
- 16.Roswell RO, Kunkes J, Chen AY, et al. Impact of sex and contact-to-device time on clinical outcomes in acute ST-segment elevation myocardial infarction-findings from the National Cardiovascular Data Registry. J Am Heart Assoc 2017;6(1). 10.1161/JAHA.116.004521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Albarqouni L, Smenes K, Meinertz T, et al. Patients’ knowledge about symptoms and adequate behaviour during acute myocardial infarction and its impact on delay time: findings from the multi-centre MEDEA Study. Patient Educ Couns 2016;99:1845–51. [DOI] [PubMed] [Google Scholar]
- 18.Al-Zaiti SS, Martin-Gill C, Sejdić E, Alrawashdeh M, Callaway C. Rationale, development, and implementation of the Electrocardiographic Methods for the Prehospital Identification of Non-ST Elevation Myocardial Infarction Events (EMPIRE). J Electrocardiol 2015;48:921–6. [DOI] [PubMed] [Google Scholar]
- 19.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581–98. [DOI] [PubMed] [Google Scholar]
- 20.Choudhary R, Sharma SM, Kumar V, Gautam DK. An observational study of prehospital and hospital delay in reperfusion for acute myocardial infarction at a university hospital in India. J Pract Cardiovasc Sci 2016;2(3):163–8. [Google Scholar]
- 21.Zègre-Hemsey JK, Burke LA, De Von HA. Patient-reported symptoms improve prediction of acute coronary syndrome in the emergency department. Res Nurs Health 2018;41:459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George L, Ramamoorthy L, Satheesh S, Saya RP, Subrahmanyam DK. Prehospital delay and time to reperfusion therapy in ST elevation myocardial infarction. J Emerg Trauma Shock 2017;10:64–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim HS, Eun SJ, Hwang JY, Lee KS, Cho SI. Symptom clusters and treatment time delay in Korean patients with ST-elevation myocardial infarction on admission. Medicine (Baltimore) 2018;97(19): e0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaul P, Armstrong PW, Sookram S, Leung BK, Brass N, Welsh RC. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. Am J Heart 2011;161:91–7. [DOI] [PubMed] [Google Scholar]
- 25.Cullen L, Greenslade JH, Menzies L, et al. Time to presentation and 12-month health outcomes in patients presenting to the emergency department with symptoms of possible acute coronary syndrome. Emerg Med J 2016;33:390–5. [DOI] [PubMed] [Google Scholar]
- 26.Elbarouni B, Goodman SG, Yan RT, et al. Impact of delayed presentation on management and outcome of non-ST-elevation acute coronary syndromes. Am Heart J 2008;156:262–8. [DOI] [PubMed] [Google Scholar]
- 27.De Von HA, Ryan CJ, Rankin SH, Cooper BA. Classifying subgroups of patients with symptoms of acute coronary syndromes: a cluster analysis. Res Nurs Health 2010;33:386–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Donnell S, McKee G, Mooney M, O’Brien F, Moser DK. Slow-onset and fast-onset symptom presentations in acute coronary syndrome (ACS): new perspectives on prehospital delay in patients with ACS. J Emerg Med 2014;46:507–15. [DOI] [PubMed] [Google Scholar]
- 29.Miller AL, Simon D, Roe MT, et al. Comparison of delay times from symptom onset to medical contact in blacks versus whites with acute myocardial infarction. Am J Cardiol 2017;119:1127–34. [DOI] [PubMed] [Google Scholar]
- 30.Goldberg R, Goff D, Cooper L, et al. Age and sex differences in presentation of symptoms among patients with acute coronary disease: the REACT trial. Rapid early action for coronary treatment. Coron Artery Dis 2000;11:399–407. [DOI] [PubMed] [Google Scholar]
- 31.Banks A, Dracup K. Factors associated with prolonged prehospital delay of African Amercians with acute myocardial infarction. Am J Crit Care 2006;15:149–57. [PubMed] [Google Scholar]
- 32.Sheifer SE, Rathore SS, Gersh BJ, et al. Time to presentation with myocardial infarction in the elderly: associations with race, sex, and socioeconmic characteristics. Circulation 2000;102:1651–6. [DOI] [PubMed] [Google Scholar]
- 33.Mell HK, Mumma SN, Hiestand B, Carr BG, Holland T, Stopyra J. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg 2017;152:983–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dracup K, McKinley S, Doering LV, et al. Acute coronary syndrome: what do patients know? Arch Intern Med 2008;168:1049–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Isaksson RM, Holmgren L, Lundblad D, Brulin C, Eliasson M. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. The Northern Sweden MONICA Study. Eur J Cardiovasc Nurs 2008; 7:152–8. [DOI] [PubMed] [Google Scholar]
- 36.Lesneski L Factors influencing treatment delay for patients with acute myocardial infarction. Appl Nurs Res 2010;23:185–90. [DOI] [PubMed] [Google Scholar]
- 37.Noureddine S, Adra M, Arevian M, et al. Delay in seeking health care for acute coronary syndromes in a Lebanese sample. J Transcult Nurs 2006;17:341–8. [DOI] [PubMed] [Google Scholar]
- 38.Lovlien M, Schei B, Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs 2007;6:308–13. [DOI] [PubMed] [Google Scholar]
- 39.Wu JR, Moser DK, Riegel B, McKinley S, Doering LV. Impact of prehospital delay in treatment seeking on in-hospital complications after acute myocardial infarction. J Cardiovasc Nurs 2011; 26:184–93. [DOI] [PubMed] [Google Scholar]


