Abstract
Background
Total joint replacement (TJR) accounts for a substantial proportion of the total expenditures for health care. Efficient utilization of health resources requires information regarding the trends of TJR. This study investigated the association of TJR with the demographic characteristics in Taiwan from 1998 to 2009. It also estimated the demand for total knee replacement (TKR) and total hip replacement (THR) in the next two decades.
Methods
International Classification of Diseases-9 (ICD-9) procedure codes were used to identify the data for primary and revision TKRs and THRs between the years 1998 and 2009 from Taiwan's National Health Insurance Research Database. Age- and sex-specific rates of such procedures were calculated. The trend in TJR rate and its future estimation were studied with regression analyses.
Results
From 1998 to 2009, the number of primary TKRs increased by 99.1% and that of primary THRs increased by 11.3%. The number of revision TKRs increased by 3.1% and that of revision THRs decreased by 13.2%. Compared with their respective rates in 2005, the rates of primary TKR and primary THR were projected to increase by 508.2% and 69.7%, respectively, in 2030. The rate of revision TKR was predicted to increase by 75.3% and that of revision THR to decrease by 36.1%.
Conclusion
This study gives an insight into the current status burden of TJR in Taiwan. TJR rate projection would be useful for future planning of budget and resources for TJR in Taiwan.
Keywords: Taiwan, total hip arthroplasty, total joint arthroplasty, total joint replacement, total knee arthroplasty, trends in arthroplasty
1. Introduction
Total joint replacement (TJR) is one of the most clinically successful interventions for patients with debilitating hip and knee diseases.1, 2 In recent decades, the procedural rates of total knee replacement (TKR) and total hip replacement (THR) have increased worldwide,3 accounting for a large share of the total health care expenditure.4 Information regarding trends in TJR is required for optimal utilization of health resources and creation of an effective health care policy. Moreover, a large amount of the resources are being used for the training of surgeons and planning for hospital capacity; this creates the need for a reliable study for the estimation of TJR in future. Studies in Nordic countries,5 Australia,6 and the USA7 have reported trends in TJR using national registry data or health insurance databases. However, only a few of them have predicted the number of TJRs to be performed in the future.4, 8, 9 To our knowledge, no study of such prediction has been reported for Asian countries. Previous studies in Asian countries to understand the temporal trends of TJR did not estimate future TJR rates.10, 11, 12 Moreover, such studies did not consider revision TJR, and in those studies the time frame of analysis was limited to 4–9 years. Therefore, a study to understand the current and future trends in primary as well as revision TJR with data from recent years and longer periods would add to the useful information of health care planning. In this study, we investigated the trends in procedure frequency from 1998 to 2009 and estimated the requirements in the next two decades for THR and TKR in Taiwan.
2. Methods
2.1. Data sources and study population
Since 1995, the Bureau of National Health Insurance (BNHI) in Taiwan has maintained a clinical database that includes > 99.6% of the total population in Taiwan.13 The BNHI database is statistically valid and useful for a study of current and emerging health issues. A longitudinal analysis of such a database is useful for understanding the temporal patterns of TJR. Some of the previous studies of knee and hip replacement in Taiwan have used the NHI Research Database,10, 14 and detailed information about the NHI program in Taiwan is described in the agency's literature.13
In this study, BNHI data were used to calculate the procedural rates of primary and revision TJR for each year between 1998 and 2009. International Classification of Diseases-9 (ICD-9) procedure codes for THR (8.51, 8.53) and TKR (8.54, 8.55) were used to identify the procedures in the database. A 2.88-million-population database was decoded, representing 12.5% of the Taiwan population. All personal identification information of patients was deleted, and patients' personal information was protected while analyzing the data. The study was approved by the Research Ethics Committee of China Medical University and Hospital, Taichung, Taiwan.
2.2. Variable definition and statistical analysis
The age- and sex-specific rates of THR and TKR for a given year were expressed in terms of the number of procedures per 100,000 person-years. The rates were calculated by dividing the number of procedures by the corresponding resident population of Taiwan in that year. The primary and revision procedure rates were analyzed separately. Changes in the rates during the 12-year period (1998–2009) were evaluated. The frequency of the procedures was categorized by sex (male and female) and 10 age groups (<40 years, 40–44 years, 45–49 years, 50–54 years, 55–59 years, 60–64 years, 65–69 years, 70–74 years, 75–79 years, and ≥80 years). The number of THR and TKR procedures performed in a given year and for a particular age–sex group was assumed to follow a Poisson distribution, which is suitable for the distribution of such count data of TJR. A multivariate Poisson regression analysis with age, sex, calendar year, and their interactions as covariates was used to estimate the future procedure rate. For estimation of future rate, the future Taiwan population estimated by the Ministry of Interior was used. The estimation method used by the Ministry of Interior includes life expectancy and the current population growth rate. Moreover, a comparison of the rates in different age groups was performed using a univariate Poisson regression analysis, and temporal trend was examined using linear regression. The statistical analysis was performed with SAS statistical software (version 9.2 for Windows; SAS Institute, Inc., Cary, NC, USA).
3. Results
3.1. Overall trends
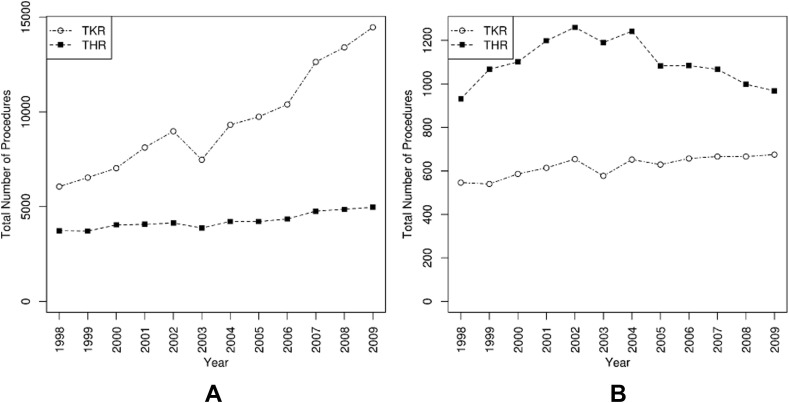
During the study period of 12 years from 1998 to 2009, a total of 114,185 primary TKRs, 50,949 primary THRs, 7462 revision TKRs, and 13,189 revision THRs were reported. The number of primary TKRs increased from 6062 in 1998 to 14,467 (an increase of 138%) in 2009. The number of primary THRs increased from 3726 to 4972 (an increase of 33%; Fig. 1 A). The number of revision TKRs increased from 546 to 675 (an increase of 23%). The number of revision THRs increased from 931 to 968 (an increase of 4%) during that period (Fig. 1B).
Fig. 1.
(A) Number of primary TKRs and THRs. (B) Number of revision TKRs and THRs. THR = total hip replacement; TKR = total knee replacement.
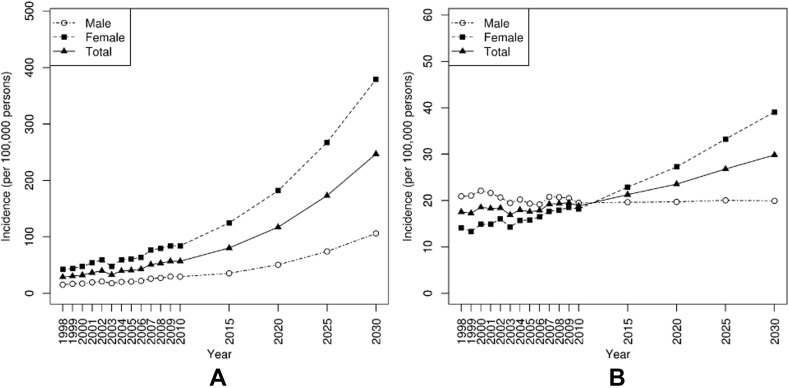
The multivariate Poisson regression model showed age, sex, and calendar year as significant factors for the year-to-year variation in all four types of TJRs. The primary TKR and THR rates showed an increasing trend with the progression of time. In 1998, the rate of primary TKR was 28.5 per 100,000 persons, which increased to 56.8 per 100,000 persons in 2009 (an increase of 99.1%; Fig. 2 A). The rate of primary THR was 17.5 per 100,000 persons in 1998, which increased to 19.5 per 100,000 persons in 2009 (an increase of 11.4%; Fig. 2B). There was a notable decrease in the rate of primary TJR in 2003, when the THR and TKR rates decreased by 8.1% and 18.2%, respectively, compared with those of the year 2002.
Fig. 2.
(A) Incidence of primary total knee replacement. (B) Incidence of primary total hip replacement.
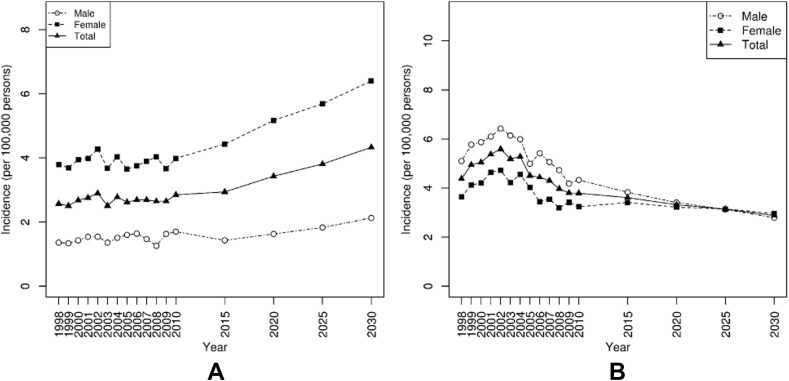
The revision TKR rate showed an increasing trend and the revision THR rate showed a decreasing trend with the progression of time. The revision TKR rate increased from 2.57 per 100,000 persons in 1998 to 2.65 per 100,000 persons (an increase of 3.1%) in 2009 (Fig. 3 A). The revision THR rate decreased from 4.38 per 100,000 persons in 1998 to 3.8 per 100,000 persons in 2009 (decrease of 13.2%) (Fig. 3B). Similar to the primary TJR rate, a notable decrease in the revision TJR rate was found in the year 2003, when the rate of revision THR decreased by 7.1% and that of revision TKR decreased by 13.4%, compared with those of the year 2002.
Fig. 3.
(A) Incidence of revision total knee replacement. (B) Incidence of revision total hip replacement.
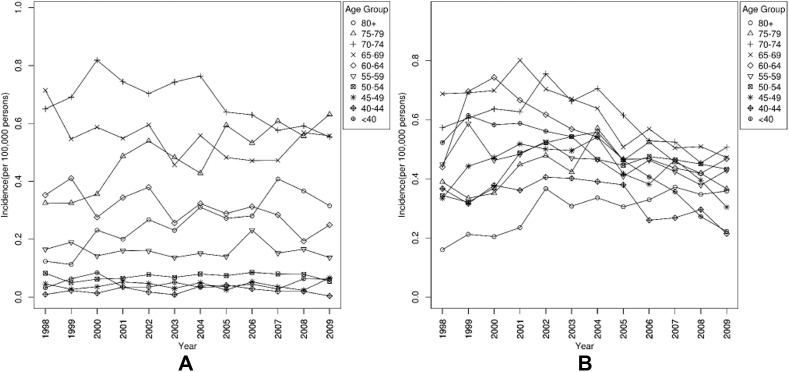
3.2. Trends by age
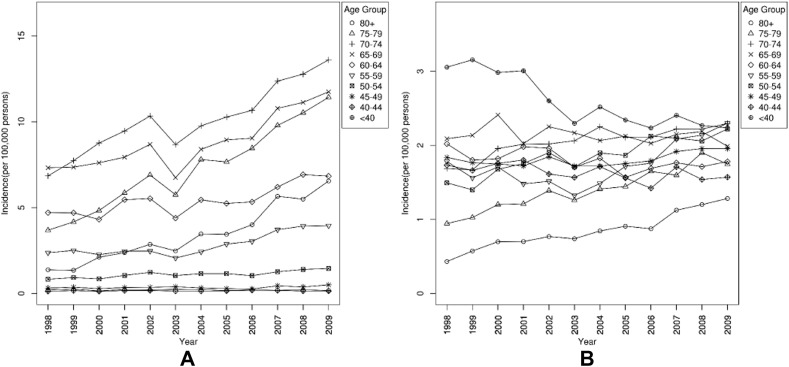
The average ages of patients who underwent primary TKR and primary THR were 69.3 ± 8.48 years and 56.9 ± 15 years, respectively. The average ages of primary TKR and primary THR patients gradually increased, by 2.5 years and 3.5 years, respectively, during the study period. Patient age was a significant factor (p < 0.05) influencing the variation of the rates of primary TKR and THR. Increasing patient age was associated with an increase in the primary TKR and THR rates. The age group of 70–74 years showed the highest rates of primary TKR and THR, compared with other age groups (p < 0.05). The age group of <40 years had the lowest rates of primary TKR and THR (p < 0.05).
The average ages of patients who underwent revision TKR and revision THR were 69.4 ± 10.37 years and 60.5 ± 14.4 years, respectively. The average ages of primary TKR and primary THR patients gradually increased by 2.0 years and 3.2 years, respectively, during the study period. Increasing patient age was associated with an increase in the revision TKR and THR rates. The age group of 70–74 years showed the highest rates for revision TKR and THR (p < 0.05). The age group of <40 years had the lowest rate of revision TKR and THR (p < 0.05; Fig. 4, Fig. 5 ).
Fig. 4.
(A) Incidence of primary total knee replacement for age groups. (B) Incidence of primary total hip replacement for age groups.
Fig. 5.
(A) Incidence of revision total knee replacement for age groups. (B) Incidence of revision total hip replacement for age groups.
3.3. Trends by sex
A significant association was found between patients' sex and the rates of all four kinds of TJRs (p < 0.05). Both sexes showed an increasing trend of the rate of primary TKR. Females accounted for 74.7% of the total number of primary TKRs and had a higher primary TKR rate than males (p < 0.05; Fig. 2A). The TKR rate in females was 42.2 per 100,000 persons in the year 1998, which increased by 99% in 2009, compared with 15.0 per 100,000 persons in males, an increase of 96.5% since 1998.
An increasing trend was found in both sexes for the primary THR rate. Males accounted for 57.8% of the total number of primary THRs and had a higher primary THR rate than females (p < 0.05). The primary THR rate in females was 14.1 per 100,000 persons in 1998, which increased by 31.4% in 2009, while it was 20.9 per 100,000 persons in males in 1998, a decrease of 1.9% in 2009 (Fig. 3A).
An increasing trend for the revision TKR rate was found in both sexes. Females accounted for 72.2% of the total number of revision TKRs and had a higher revision TKR rate (p < 0.05) than males. The revision TKR rate in females was 3.79 per 100,000 persons in 1998, which decreased by 3.4% in 2009. The revision TKR rate was 1.36 per 100,000 persons in 1998 in males, which increased by 19.9% in the year 2009 (Fig. 3B).
A decreasing trend was found in the revision THR rates for both sexes. Females constituted 41.8% of the total number of revision THRs. However, the revision THR rate was higher in males (p < 0.05) than in females. The rate of revision THR in females was 3.64 per 100,000 persons in 1998, which decreased by 6.0% in 2009. The revision THR rate was 5.1 per 100,000 persons in males in 1998, which decreased by 18.0% in 2009 (Fig. 3B).
3.4. Projection of procedure rates
The projected rates for the different TJRs, compared with their respective rates, in 2005 were estimated. A comparison of the rates between the years 2005 and 2030 was made, to compare with the results of the previous studies conducted by Kurtz et al4, 9 in the USA.
The rate of primary TKR was projected to increase by 508.2% by 2030 (Fig. 2A). It would increase by 523.2% in females and by 415.8% in males. The rate of primary THR was estimated to increase by 69.7% (Fig. 2B). It would increase in females by 147.3% and in males by 3.1%.
The rate of revision TKR was estimated to increase by 75.3%. It would increase in females by 75.3% and in males by 33.1%. The rate of revision THR was estimated to decrease by 36.1% (Fig. 3). It would decrease in females by 26.4% and in males by 44.1%.
4. Discussion
This study investigated the temporal trends of TKR and THR in Taiwan during a period of 12 years, from 1998 to 2009. This is the trend analysis of TJR in Taiwan, which includes revision TJR in the study and estimates the rate of TJR in the future. The study was conducted using the NHI Research Database for patients who underwent TJR of the knee or hip. This study indicated that the number and procedural rates of primary TKRs and THRs have increased in Taiwan. The increasing trend was more pronounced for TKR. The rate of primary TKR increased by around 99% between 1998 and 2009. The THR rate increased by only 11% during that period. The rate of revision TKR has increased by only 3% and that of the revision THR decreased by 13%.
The overall increase in the trends of the primary TKR and THR may be explained, at least in part, by the growing population of elderly patients, improved surgical techniques, implant materials and designs, and expanding indications for joint replacement.15, 16 Such an increase in the rate is consistent with the result of a previous study conducted by Tien et al.10 The increase of primary TKR reported in Tien et al's10 study was 140% in 9 years (1996–2004), while our study showed an increase of 99% in 12 years. The smaller increase in the procedural rate shown in our study may suggest improved medical management of clinical conditions such as osteoarthritis. Similar studies in the USA,4, 9 Nordic countries,5 Australia,6 and South Korea12 showed a higher rate of primary TKR than that in Taiwan, in the respective study periods in those studies. Such differences in the procedural rate of TJR from Western countries may be due to differences in the incidence of obesity, sociocultural beliefs about surgery, work and exercise habits, hereditary characteristics, and socioeconomic status between Taiwan and the Western populations. Taiwan's population has an obesity rate of 17–18%; in Western countries it is 24–34%,17, 18 which may be a significant factor for differences in TJR rates between Taiwan and the Western population. Moreover, Taiwan NHI criteria for coverage of sponsored arthroplasty may also add to the difference in procedural rate.
The increase in the primary THR rate in Taiwan from 1998 to 2009 was only 11%, which was much smaller than that of the primary TKR rate. The lower incidence of hip osteoarthritis, as compared with knee, may explain this difference.19 The increase in the primary THR rate was smaller than those reported in previous studies.10, 14 The smaller increase may be due to a decreased incidence of avascular necrosis of the femoral head in patients receiving THR in Taiwan. Avascular necrosis of the femoral head is among the major causes of THR in Taiwan.10 Similar to primary TKR, primary THR showed a lower rate compared with those in the USA, Nordic countries, and Australia, but higher than that in South Korea. Despite a similar prevalence of osteoarthritis20 among these countries, the lower rate of THR in Taiwan compared with that in the Western countries may be attributed to the same factors mentioned above for primary TKR. The reasons for the higher rate compared with that of South Korea need to be explored.
The primary TKR and THR rates showed an increasing trend with an increase in patient age. Similar to the results of studies from the Western countries and South Korea, the TKR rates were high in the age group of 65–75years. The increase in the incidence of symptomatic osteoarthritis with the increase in age21, 22 explains this trend. The average age of patients has increased for both primary TKR and THR. Advancements in the medical management of clinical conditions such as osteoarthritis may help patients delay joint replacement surgeries, resulting in an increase in the average age of patients undergoing primary TJR.
Differences in the primary TKR and THR rates were associated with sex. The primary TKR rate was higher in females. Similar results for the primary TKR with respect to sex were reported in studies from other countries. However, in our study, the primary THR rate was higher in males in contrast to the results from studies in other countries.5, 6, 7, 12 Such a difference may be due to the higher prevalence of avascular necrosis of the femoral head in males in Taiwan population.10 Similar to primary TKR, revision TKR showed an increasing trend with the progression of time and a higher rate in females. However, revision THR showed a decreasing trend with the progression of time, and the rate was higher in males. The revision THR rate did not increase with the increase of the primary THR rate, which may be explained as follows: (1) advancements in prosthesis design, such as wear-resistant polymer-lined implants23, 24; (2) improvement in surgical techniques25 for THR to ensure alignment of the implant with the joint; and (3) sociocultural factors such as patients' preference to avoid the pain and discomfort of revision surgery and receive the care offered by their family members.
The average patient age for both revision TKR and THR has increased. The increase may be attributed to the increase in the average patient age for the primary TKR and THR.
In 2007, Kurtz et al4 predicted that in the USA in 2030, the rates of primary TKR, primary THR, revision TKR, and revision THR would increase by 673%, 174%, 600%, and 137%, respectively, compared with those in 2005. The estimation in their study was higher than those in ours (1.3 times for primary TKR, 2.5 times for THR, 8.0 times for revision TKR, and 4.8 times for revision THR). In 2014, in another study by Kurtz et al,9 the increase in the primary THR rate was estimated to be higher than that in their earlier prediction. The lower estimated increase of rates in our study may be due to the same factors mentioned above as the reasons for lower primary TKR and THR, and also due to the difference in the statistical model used in our studies. However, in Taiwan, the projected rate of primary TKR is high, having a significant impact on health budgets and service provisions.
A notable decrease in the THR and TKR rates in 200326 was due to the severe acute respiratory syndrome outbreak during that year. In that year, for several months only a limited number of the facilities were available for TJR in Taiwan.
The limitations inherent to a large administrative database are applicable to our study. First, the current study used ICD-9 codes, which may lead to under-reporting of comorbidities. Second, since this was an observational study, the associations observed are not necessarily causal relationships. Third, a limited number of variables are available in the BNHI database, which makes it impossible to control other important confounders such as clinical and genetic factors.
In conclusion, this study offers an insight into the current status of TJR in Taiwan, and its projection results can be useful for future planning of budget and resources for TJR in Taiwan. The current study can be further extended to observe changes in the pattern of hospital stay, economic burden to the patient and country, and the effect of different treatment modalities on the trends.
Footnotes
Conflicts of interest: The authors declare that there are no conflicts of interest related to the subject matter or materials discussed in this article.
References
- 1.Jones C.A., Beaupre L.A., Johnston D.W.C., Suarez-Almazor M.E. Total joint arthroplasties: current concepts of patient outcomes after surgery. Clin Geriatr Med. 2005;21:527–541. doi: 10.1016/j.cger.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D.J. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh J.A. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J. 2011;5:80–85. doi: 10.2174/1874325001105010080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Robertsson O., Bizjajeva S., Fenstad A.M., Furnes O., Lidgren L., Mehnert F. Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop. 2010;81:82–89. doi: 10.3109/17453671003685442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wells V.M., Hearn T.C., McCaul K.A., Anderton S.M., Wigg A.E.R., Graves S.E. Changing incidence of primary total hip arthroplasty and total knee arthroplasty for primary osteoarthritis. J Arthroplasty. 2002;17:267–273. doi: 10.1054/arth.2002.30414. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S., Mowat F., Ong K., Chan N., Lau E., Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S.M., Lau E., Ong K., Zhao K., Kelly M., Bozic K.J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurtz S.M., Ong K.L., Lau E., Bozic K.J. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–630. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 10.Tien W.C., Kao H.Y., Tu Y.K., Chiu H.C., Lee K.T., Shi H.Y. A population-based study of prevalence and hospital charges in total hip and knee replacement. Int Orthop. 2009;33:949–954. doi: 10.1007/s00264-008-0612-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi H.Y., Chiu H.C., Chang J.K., Wang J.W., Culbertson R., Khan M.M. Evaluation and prediction of health-related quality of life for total hip replacement among Chinese in Taiwan. Int Orthop. 2008;32:27–32. doi: 10.1007/s00264-006-0268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim H.A., Kim S., Seo Y.I., Choi H.J., Seong S.C., Song Y.W. The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology. 2008;47:88–91. doi: 10.1093/rheumatology/kem308. [DOI] [PubMed] [Google Scholar]
- 13.National health insurance health statistics annual report. Available at: http://www.mohw.gov.tw/cht/DOS/Statistic.aspx?f_list_no=312&fod_list_no=2680. [accessed 13.08.13].
- 14.Lai Y.S., Wei H.W., Cheng C.K. Incidence of hip replacement among national health insurance enrollees in Taiwan. J Orthop Surg Res. 2008;3:42. doi: 10.1186/1749-799X-3-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deaton A., Paxson C. Growth, demographic structure, and national saving in Taiwan. Popul Dev Rev. 2000;26:141–173. [Google Scholar]
- 16.Ritter M.A. The anatomical graduated component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Jt Surgery Br. 2009;91:745–749. doi: 10.1302/0301-620X.91B6.21854. [DOI] [PubMed] [Google Scholar]
- 17.James P.T., Leach R., Kalamara E., Shayeghi M. The worldwide obesity epidemic. Obes Res. 2012;9:228S–233S. doi: 10.1038/oby.2001.123. [DOI] [PubMed] [Google Scholar]
- 18.Yeh C.J., Chang H.Y., Pan W.H. Time trend of obesity, the metabolic syndrome and related dietary pattern in Taiwan: from NAHSIT 1993–1996 to NAHSIT 2005–2008. Asia Pac J Clin Nutr. 2011;20:292–300. [PubMed] [Google Scholar]
- 19.Cushnaghan J., Dieppe P. Study of 500 patients with limb joint osteoarthritis. I. Analysis by age, sex, and distribution of symptomatic joint sites. Ann Rheum Dis. 1991;50:8–13. doi: 10.1136/ard.50.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arden N., Nevitt M.C. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20:3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 21.Jordan J.M., Helmick C.G., Renner J.B., Luta G., Dragomir A., Woodard J. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–180. [PubMed] [Google Scholar]
- 22.Fransen M., Bridgett L., March L., Hoy D., Penserga E., Brooks P. The epidemiology of osteoarthritis in Asia. Int J Rheum Dis. 2011;14:113–121. doi: 10.1111/j.1756-185X.2011.01608.x. [DOI] [PubMed] [Google Scholar]
- 23.Engh C.A., Jr., Stepniewski A.S., Ginn S.D., Beykirch S.E., Sychterz-Terefenko C.J., Hopper R.H. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non-cross-linked Enduron polyethylene liners. J Arthroplasty. 2006;21:17–25. doi: 10.1016/j.arth.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Dorr L.D., Wan Z., Shahrdar C., Sirianni L., Boutary M., Yun A. Clinical performance of a Durasul highly cross-linked polyethylene acetabular liner for total hip arthroplasty at five years. J Bone Joint Surg Am. 2005;87:1816–1821. doi: 10.2106/JBJS.D.01915. [DOI] [PubMed] [Google Scholar]
- 25.Mont M.A., Seyler T.M., Ulrich S.D., Beaule P., Boyd H., Grecula M. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh Y.H., Chen C.W.S., Hsu S.B. SARS outbreak, Taiwan, 2003. Emerg Infect Dis. 2004;10:201–206. doi: 10.3201/eid1002.030515. [DOI] [PMC free article] [PubMed] [Google Scholar]