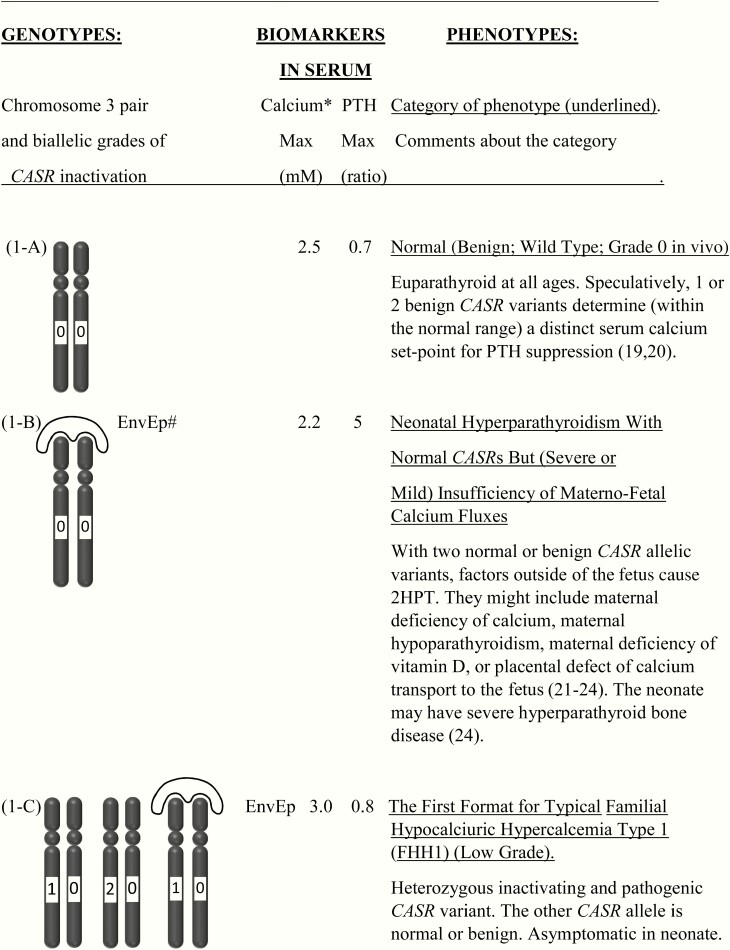
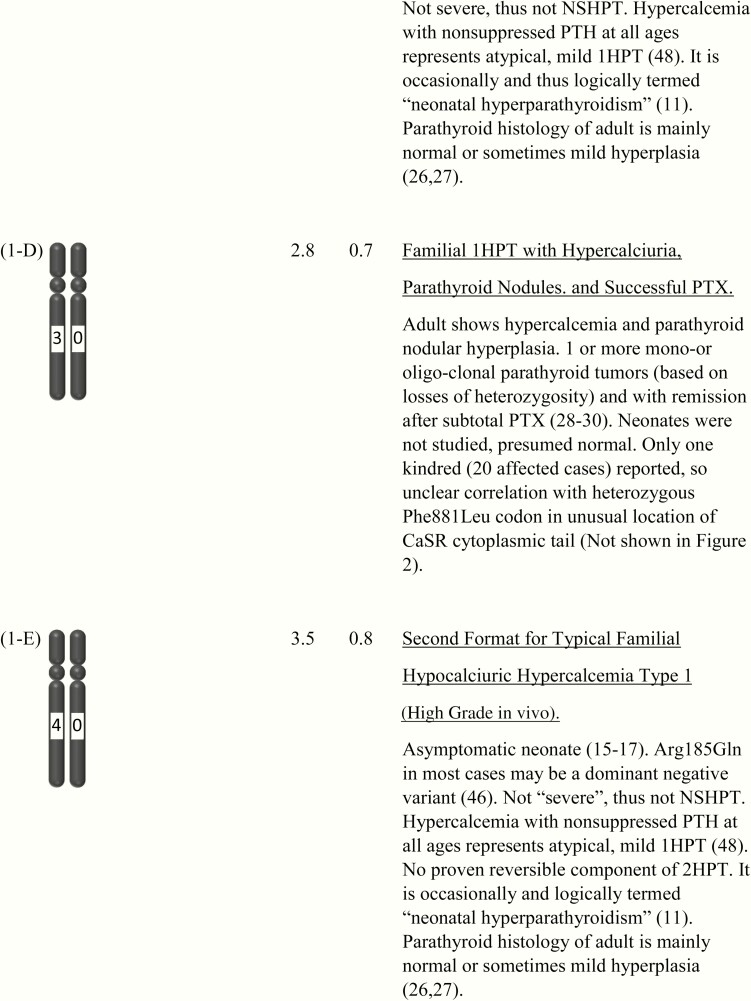
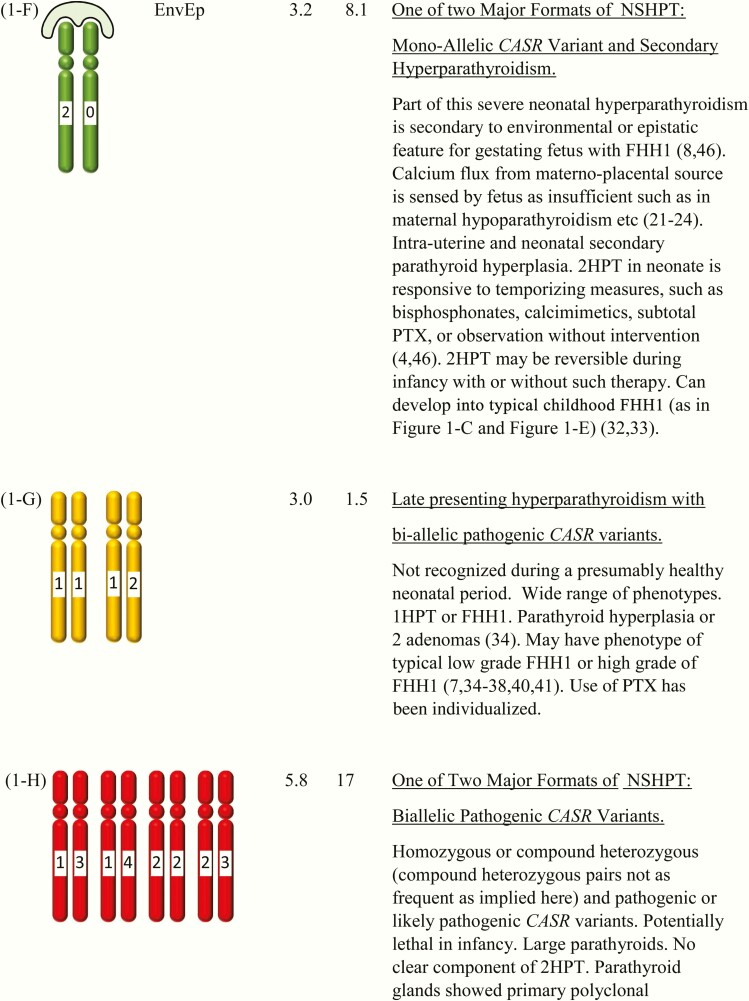
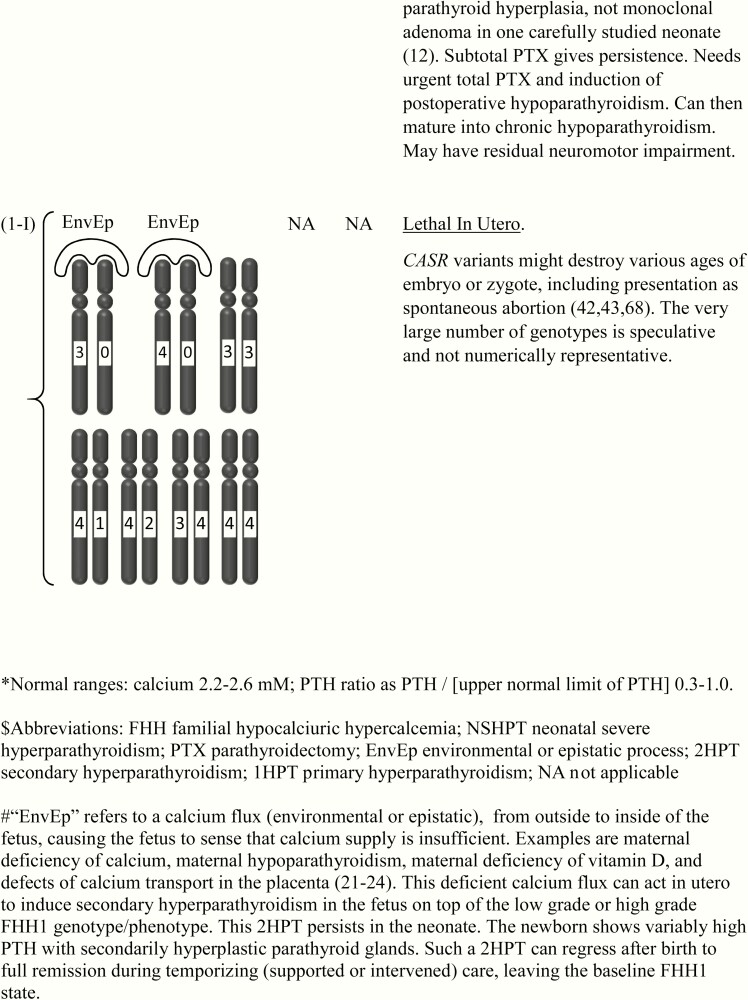
Figure 1.
This shows the category related to neonatal severe hyperparathyroidism (NSHPT), dependent on secondary hyperparathyroidism and/or upon the dosage and stages of inactivation of CASR alleles at chromosome 3q13.3-q21.1. This is a speculative synthesis of data from human and animal species, intended to give a logical background for a spectrum of phenotypes and genotypes. The number of chromosomal pairs in a subpanel is somewhat arbitrary and intended to accommodate overall most of the many possibilities considering 5 grades of severity for each allele. The CASR also causes monogenic phenotypes by activating variants such as in autosomal dominant hypoparathyroidism, autosomal resistant hypoparathyroidism, or type V Bartter syndrome (2, 3); these activating variants are not shown here. Degree of inactivation varies from 0 to 4 or from benign (no inactivation) to pathogenic (maximal inactivation). Degree of inactivation of the calcium-sensing receptor in vitro correlates with serum calcium in vivo (11). The GNA11 and AP2S1 genes can be incorporated into this speculative scheme in similar but more complicated ways (not shown). Red is NSHPT with biallelic-inactivating and pathogenic variant of the CASR (Fig. 1-H). Green is NSHPT with monoallelic-inactivating and pathogenic or likely pathogenic CASR variant and secondary hyperparathyroidism (Fig. 1-F). Yellow is late-onset biallelic-inactivating and pathogenic or likely pathogenic variant of the CASR (Fig. 1-G).