Abstract
Coronaviruses as well as influenza A viruses are widely spread in pig fattening and can cause high economical loss. Here we infected porcine precision-cut lung slices with porcine respiratory coronavirus and two Influenza A viruses to analyze if co-infection with these viruses may enhance disease outcome in swine. Ciliary activity of the epithelial cells in the bronchus of precision-cut lung slices was measured. Co-infection of PCLS reduced virulence of both virus species compared to mono-infection. Similar results were obtained by mono- and co-infection experiments on a porcine respiratory cell line. Again lower titers in co-infection groups indicated an interference of the two RNA viruses. This is in accordance with in vivo experiments, revealing cell innate immune answers to both PRCoV and SIV that are able to restrict the virulence and pathogenicity of the viruses.
Keywords: Coronavirus, Influenza A virus, Porcine lung, Co-infection, Porcine respiratory disease complex
Highlights
-
•
PCLS can be used to analyze porcine respiratory coronavirus infection.
-
•
Co-infection of PCLS with PRCoV and SIV reduces viral replication efficiency.
-
•
SIV replication is reduced after co-infection of NPTr cells with PRCoV.
-
•
Porcine influenza and coronaviruses interfere during infection.
1. Introduction
Swine in pig fattening are ubiquitously prone to different kinds of pathogens that can be fatal or even beneficial when combined. Porcine respiratory coronavirus (PRCoV) with a high sequence homology to transmissible gastroenteritis virus (TGEV) is considered to protect swine from the fatal intestinal infection due to cross-protection between these two coronaviruses (Bernard et al., 1989). PRCoV belongs to the family Coronaviridae within the genus α-Coronavirus (Thiel, 2007). These single stranded RNA viruses of positive genome orientation use their spike protein for receptor binding (Delmas et al., 1992, Siddell et al., 1983). Like TGEV, PRCoV uses aminopeptidase N for virus entry but replicates solely in the respiratory tract of swine (Rasschaert et al., 1990, Rasschaert et al., 1987). Infection by PRCoV causes mild clinical symptoms in swine like sneezing, coughing, mild fever, polypnea and anorexia (Bourgueil et al., 1992, Cox et al., 1990, Jung et al., 2007). However, this coronavirus can be part of the porcine respiratory disease complex, like the swine influenza A viruses (SIV) subtype H3N2 or H1N1. Influenza A viruses belong to the family Orthomyxoviridae and are viruses with single stranded RNA of negative polarity (Kuntz-Simon and Madec, 2009). They co-evolved in Europe and are typed by their glycoproteins hemagglutinin (H) and neuraminidase (N) (Marozin et al., 2002). Genetic drift and reassortment of the influenza subtypes cause different disease outcome in the same host, e.g. H3N2 is a reassorted SIV from the avian originated H1N1 and another H3N2 (Castrucci et al., 1993, Guan et al., 1996, Marozin et al., 2002, Meng et al., 2013). The hemagglutinin binds to the sialic acids at the cell surface for virus entry (Doms et al., 1986, Gambaryan et al., 2005). Swine influenza A viruses cause the typical swine flu with symptoms varying from fever and depression or coughing (barking) and discharge from the nose or eyes, as well as sneezing and breathing difficulties (Meng et al., 2013). The targets of these SIV subtypes are the cells of the respiratory epithelium (Punyadarsaniya et al., 2011).
Generally, PRCoV infection is common in pig fattening, but only limited information is available on the effect of co-infection with other viruses and their effect on disease outcome in the host (Jung et al., 2009). Studies on swine infected with PRCoV and SIV H1N1 showed clinical disease signs to be more severe in those swine infected with both viruses, but no difference in antibody responses against SIV H1N1 were measured (Van Reeth and Pensaert, 1994). Earlier studies on co-infection of swine infected intranasally and by aerosol with PRCoV and SIV H3N2 or H1N1 did not enhance the pathogenicity of these viruses (Lanza et al., 1992). Nasal swabs and tissue analysis showed isolated virus rather in mono- than co-infected swine, suggesting in vivo interference in the replication of PRCoV and SIV (Lanza et al., 1992). To further study this phenomenon other tools for analysis are necessary to get insight into the processes of viral infection in the respiratory tract. Precision cut lung slices (PCLS) are a useful tool to analyze viral infiltration ex vivo. Lung slices have been used in scientific studies from a variety of animals like rodents, caprine or bovine lung or even human lung (Abdull Razis et al., 2011, Banerjee et al., 2012, Braun and Tschernig, 2006, Goris et al., 2009, Kirchhoff et al., 2014a, Kirchhoff et al., 2014b). However, although porcine PCLS have been analyzed in the context of influenza A virus infection and co-infection with bacteria, the co-infection with coronaviruses remains to be investigated (Meng et al., 2013, Punyadarsaniya et al., 2011, Wu et al., 2016). Porcine lung slices are easy to produce and reproduce under stable conditions, while mimicking respiratory infection. In the present study infection of PCLS by PRCoV was analyzed and compared with infection by SIV H3N2 and H1N1. Finally, the influence of co-infection with both virus species on viral replication efficiency in the PCLS system was investigated. Possible differences or interferences in co- infections as result of innate immune responses are discussed.
2. Materials and methods
2.1. Cell culture
Newborn pig trachea cells (NPTr) were purchased from Istituto Zooprofilattico Sperimentale, della Lombardia e dell' E-milia Romagna, Brescia, Italy (Ferrari et al., 2003). NPTr and Madin-Darby canine kidney cells (MDCKII, provided by G. Herrler, Institute of Virology, University of Veterinary Medicine Hannover) were maintained in Eagle's minimal essential medium (EMEM) supplemented with 10% fetal calf serum (Biochrom AG, Berlin) (Richardson et al., 1981). Cells were incubated in a humidified atmosphere containing 5% CO2 at 37 °C and passaged every 2–3 days.
2.2. Swine lungs
Two different sources for swine lung were used. One part of the lung (n = 14) derived from local slaughterhouse of ca 9 month old pig (Hannoversche Schlachthof UG, Hannover, Germany). Further slices were produced from lungs of three month old healthy crossbred pigs obtained from conventional housing in the Clinics for Swine and Small Ruminants and the Institute for Physiology at the University of Veterinary Medicine Hannover. In total 13 independent experiments for PCLS production were done using lung from 20 pigs.
2.3. Precision cut lung slices
The left anterior, right apical and intermediate lobe of the swine lung was removed and carefully filled via the bronchioles with 37 °C warm low-melting agarose (AGAROSE LM; GERBU, Gaiberg, Germany) until lobes were completely inflated. Lobes were set on ice for up to 30 min for solidity of the lung tissue. The lobes were then set apart and cut transverse to the bronchioles. Pieces were fitted to a Krumdiek tissue slicer (TSE systems, model MD4000-01) by a stamper tool. Cylindrical pieces were set in the machine to produce slices of ca 250 μm thickness at a cycle speed of 60 slices/min. PCLS were collected in RPMI 1640 medium (Invitrogen/Gibco, Germany) without antibiotics. PCLS were selected in 24 well plates filled with 1 mL of RPMI 1640 medium with added antibiotics in a 500 L flask (2.5 mg amphotericin B/L, 1 mg clotrimazole/L, 10 mg enrofloxacin/L, 50 mg canamycin/L, 1:100 dilution of penicillin/streptomycin stock solution containing 10,000 U penicillin G/mL and 10 mg streptomycin/mL). The PCLS stayed at rest in a humidified atmosphere containing 5% CO2 at 37 °C for 24 h. Afterwards, medium was removed and new medium was added. Slices were separated again for their ciliary activity by light microscopy (Zeiss Axiovert 35).
2.4. Infection of PCLS or NPTr cells
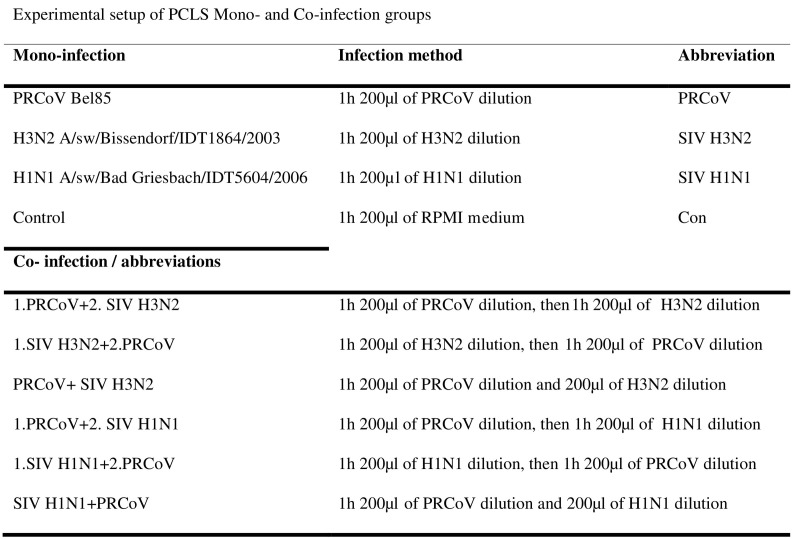
Swine influenza A virus subtype H3N2 (A/sw/Bissendorf/IDT1864/2003) was provided by Ralf Dürrwald, IDT Biologika GmbH, Dessau-Rosslau, Germany (titer 1.37 × 107 TCID50/mL). Swine influenza A virus subtype H1N1 (A/sw/Bad Griesbach/IDT5604/2006) was provided by Prof. Michaela Schmidtke, University of Jena, Germany (titer 1.71 × 106 TCID50/mL) and PRCoV Bel85 (titer 7.32 × 106 TCID50/mL) was provided by Luis Enjuanes (Department of Molecular and Cell Biology, Centro Nacional de Biotecnología, CSIC, Campus Universitario de Cantoblanco). All virus strains were diluted in RPMI to a titer of 5.5 × 105 TCID50/mL. In total, 200 μL of virus dilution was added to one PCLS per well. For mono-infection diluted virus was incubated with PCLS for 1 h. Different co-infection models were tested, starting with influenza virus incubation for 1 h followed by PRCoV incubation or vice versa. Additionally simultaneous infection of PCLS with the different influenza A virus subtypes and PRCoV for 1 h were performed. For control PCLS, 200 μL of medium was added for 1 h. In total 10 different mono- and co-infection groups were used per experiment (Fig. 1 ). On NPTr cells the same virus infection groups were used to analyze differences in mono- and co-infection in cell culture. Cells were seeded on cover slips in a 24 well plate and incubated by a multiplicity of infection of 1 for 1 h. After 72 h of infection cells were analyzed by antibody staining and supernatant was collected for titration of infectious virus.
Fig. 1.
Experimental setup of mono- and coinfection groups of PCLS and NPTr cells. Equal virus dilution was added to the samples, mono- infection by PRCoV and SIV H3N2 or SIV H1N1. Co-infections were done by addition of PRCoV and SIV H3N3/SIV H1N1 simultaneously or by pre-infection with PRCoV, following SIV H3N2/SIV H1N1 and vice versa.
2.5. Ciliary activity assay
PCLS produced from 6 independent experiments were analyzed for their ciliary activity individually under a light microscope (Zeiss Axiovert 35). The round shaped bronchi were divided into ten segments, each of which was monitored for presence or absence of ciliary beating like described before (Meng et al., 2013, Punyadarsaniya et al., 2011). Infection studies were performed with PCLS that showed initially 100% active ciliary beating. Uninfected control slices served as negative control in each experiment. Per swine, ciliary activity of PCLS was measured for each group daily in duplicate for up to 7d post infection to monitor their vitality.
2.6. Immunofluorescence assay
Immunofluorescence was used to show viral antigen in NPTr cells by staining the nucleoprotein of the viruses. All treatments were done at room temperature. First NPTr cells were fixed by 200 μL 3% paraformaldehyde for 20 min. Cells were washed three times in PBS and 200 μL 0.1 M glycine solution was added for 5 min. After washing, the cells were permeabilized with 200 μL 0.2% Triton X-100 for 20 min. All antibodies were diluted in PBS with 1% bovine serum albumin. The coronavirus nucleocapsid protein was stained by monoclonal mouse anti-coronavirus-antibody (FIPV3-70; Invitrogen, Thermo Fischer Scientific) diluted 1:1000 and incubated for 1 h. After washing, bound antibody was stained for 45 min by anti-mouse IgG CY3 conjugate (1:200, Sigma-Aldrich). Cover slips in the wells were washed again by PBS and influenza A virus was stained by influenza A virus nucleoprotein (NP) antibody (AbDSeroTec, Düsseldorf). Influenza NP antibody was diluted 1:750 and incubated on the cells for 1 h. After washing three times, NPTr cells were incubated with anti-mouse IgG FITC (Sigma-Aldrich) diluted 1:200 for 45 min. Nuclei were stained by DAPI (4′,6-diamidino-2-phenylindole) and coverslips were embedded in Mowiol and stored until analysis by fluorescence microscopy (Nikon Eclipse Ti-E).
2.7. Titer analysis
Virus titers were analyzed by harvesting the supernatant of mono- and co-infected PCLS as well as NPTr cells at 72 h post infection and stored at − 80 °C. Supernatant of PCLS and NPTr cells of at least 3 independent experiments were collected. PCLS supernatant of infection group SIV H1N1 + PRCoV was analyzed twice in independent experiments. The samples were used to perform endpoint dilution titration of the same supernatant on NPTr as well as MDCK II cells. Supernatant was diluted in 10-fold serial dilution steps with 100 μL per well in 4 repeats. The 96-well plates were visually analyzed after 72 h and scored for their virus induced cytopathogenic effects.
2.8. Statistics
Statistical analysis was done using GraphPad Prism5. For analysis each infection group was compared. p-Values were analyzed by t-test for unpaired values. Significant differences were shown at p < 0.05, p < 0.025 or lower than p < 0.001 respectively.
3. Results
Infection by PRCoV and SIV H3N2 or SIV H1N1 of PCLS and NPTr cells was analyzed to determine potential differences in mono- and co-infection. In every experiment uninfected PCLS were evenly analyzed, to eliminate potential contaminations of the animals or cells by PRCoV or SIV (data not shown). Contamination of swine PCLS led to complete exclusion of the data obtained by respective animals.
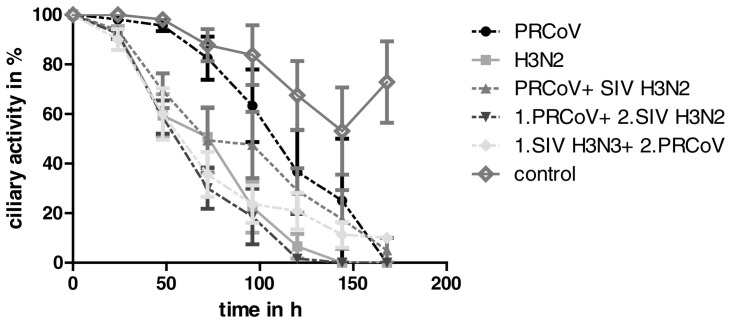
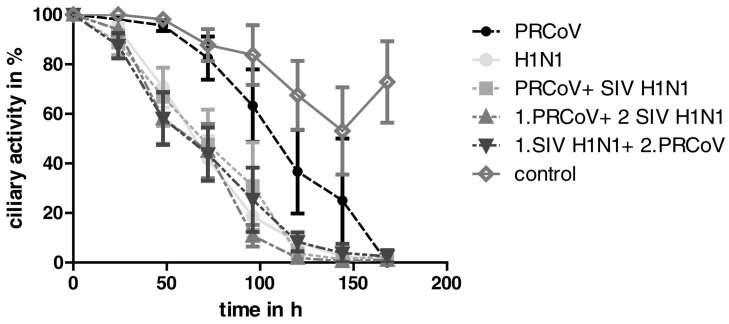
The ciliary activity of PCLS was reduced due to the infection of the bronchi and their epithelial cell layer by PRCoV, SIV H3N2, SIV H1N1 and their co-infection groups. Mono-infected PCLS showed only slight reduction of the ciliary activity when infected by PRCoV (Fig. 2, Fig. 3 ). However, a higher decrease in ciliary activity was found for SIV H3N2 as well as in all co-infection groups at all time points tested (Fig. 2). Differences in ciliary activity reduction between mono-infection of PRCoV and co-infection with SIV H3N2 were visible already after 48 h (Fig. 2). There was no measureable difference between the mono-infected slices by SIV H3N2 and the other co-infection groups. Comparison of PRCoV and SIV H1N1 showed similar differences of the coronavirus compared to all co-infection groups as were found for SIV H3N2 (Fig. 3). Furthermore, the SIV H1N1 and the co-infection groups did not show any difference in reduced activity of the ciliated cells at any time point (Fig. 3). This supported the tendency that PRCoV is able to induce ciliary activity reduction after 4 days, but on a much lower level than SIV H3N2 or SIV H1N1 and all co-infection groups. Whereas PRCoV infection after 72 h showed still round about 80% ciliary activity, mono-infection by SIV H3N2 or SIV H1N1 and all co-infection groups reduced the ciliary activity of the PCLS after 72 h by > 50% (Fig. 2, Fig. 3).
Fig. 2.
Ciliary activity of mono- and co-infected PCLS with PRCoV, SIV H3N2, and uninfected control slices, up to 168 h p.i.. Reduction in ciliary activity is shown on the y-axis.
Fig. 3.
Ciliary activity of mono- and co-infected PCLS with PRCoV, SIV H1N1, and uninfected control slices, up to 168 h p.i.. Reduction in ciliary activity is shown on the y-axis.
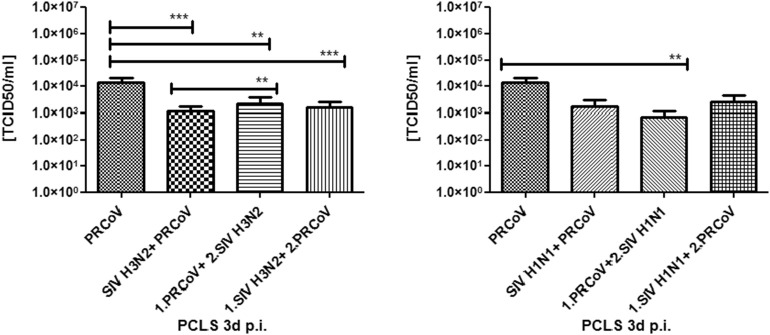
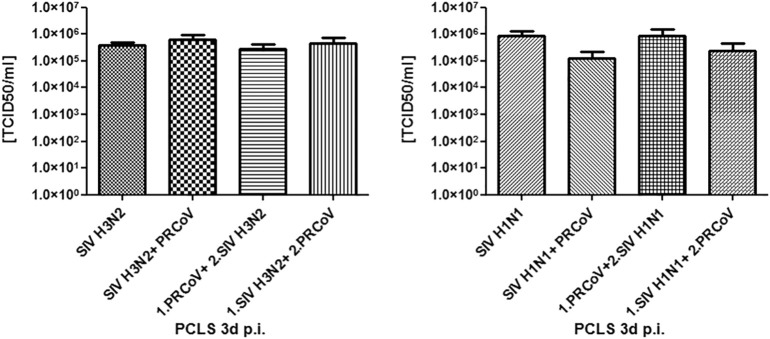
Supernatants of PCLS harvested 3 days post infection was analyzed by endpoint dilution on two different cell types. On NPTr cells mono-infection of PRCoV was compared to co-infection groups (Fig. 4 ). NPTr cells were susceptible to PRCoV infection, but only low cytopathic effect were seen by SIV infection of NPTr. There were significant differences between mono-infection with PRCoV and co-infections of the slices, especially with SIV H3N2 (Fig. 4). However, the titer of PRCoV was higher than the ones of co-infected slices. In co-infection only 1.PRCoV + 2.SIV H3N2 showed a significant higher titer than PRCoV + SIV H3N2 (p = 0.0108). All other combinations in co-infection with SIV H3N2 or SIV H1N1 did not reveal any significant differences between the titers of the PCLS supernatants (Fig. 4). PRCoV is not able to invade MDCKII cells, therefore these cells were used for titration of the same PCLS supernatants (Fig. 5 ). While excluding PRCoV titers from the analysis of co-infected PCLS, varying titer of the influenza viruses were measured. Virus in the PCLS supernatant at 3 days post infection showed no significant different amount of infectious SIV H3N2 or SIV H1N1 compared to any co-infection group (Fig. 5).
Fig. 4.
Endpoint dilution titration of PCLS supernatant 3 d p.i. on NPTr cells. Comparison of mono- and co-infection by PRCoV and SIV H3N2 (left), or SIV H1N1 (right). **p < 0.025, ***p < 0.001.
Fig. 5.
Endpoint dilution titration of PCLS supernatant 3 d p.i. on MDCK II cells. Comparison of mono- and co-infection by PRCoV and SIV H3N2 (left), or SIV H1N1 (right); (no significant differences).
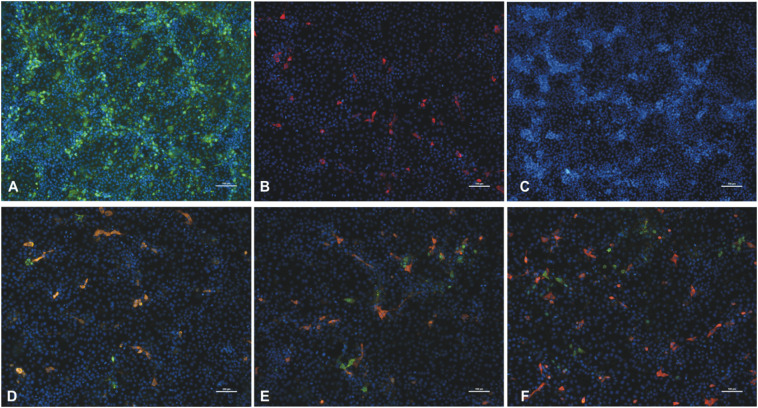
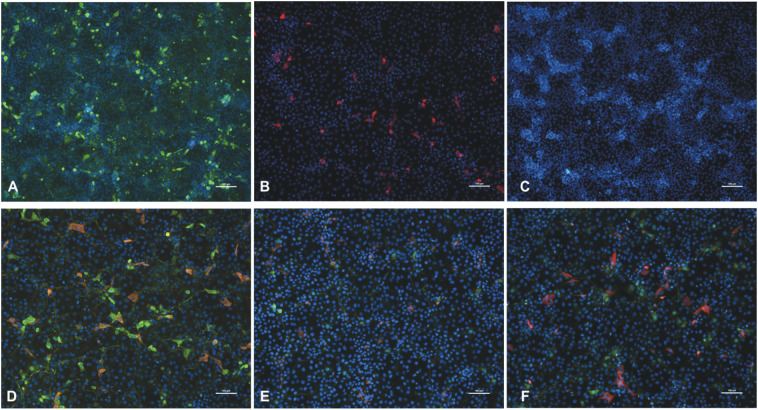
NPTr cells served as an additional model to analyze differences in mono- and co-infection by the coronavirus and SIVs. NPTr infection was done using an MOI of 1 and was analyzed by fluorescence microscopy 3 days post infection. Already fluorescence microscopy analysis of the mono-infection showed that SIV H3N2 was able to infect more cells than PRCoV (Fig. 6A/B). Furthermore, less SIV H3N2 viral nucleoprotein was visible in cover slips co-infected by both viruses (Fig. 6D, E, F). Here, no obvious differences between co-infections were visible. Equal tendencies were shown by cells co-infected with SIV H1N1 (Fig. 7 D, E, F). However, simultaneous infection of NPTr cells with PRCoV and SIV H1N1 indicated similar amounts of SIV H1N1 nucleoprotein compared to mono-infection (Fig. 7D).
Fig. 6.
NPTr cells infected by SIV H3N2 and PRCoV. Viral nucleoprotein of SIV H3N2 (green, A) or PRCoV (red, B), compared to uninfected control (C) was stained by monoclonal antibodies 3 d p.i.. Co-infection: PRCoV + SIV H3N2 (D), 1.PRCoV + 2.SIV H3N2 (E), 1.SIV H3N2 + 2.PRCoV (F). Nuclei were stained by DAPI (blue). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 7.
NPTr cells infected by SIV H1N1 and PRCoV. Viral nucleoprotein of SIV H1N1 (green, A) or PRCoV (red, B), compared to uninfected control (C) was stained by monoclonal antibodies 3 d p.i.. Co-infection: PRCoV + SIV H1N1 (D), 1.PRCoV + 2.SIV H1N1 (E), 1.SIV H1N1 + 2.PRCoV (F). Nuclei were stained by DAPI (blue). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
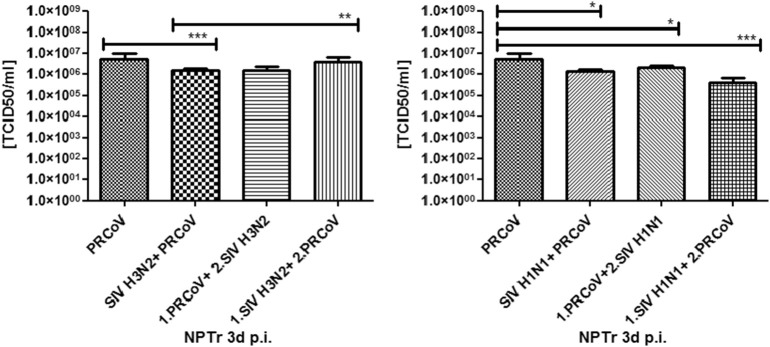
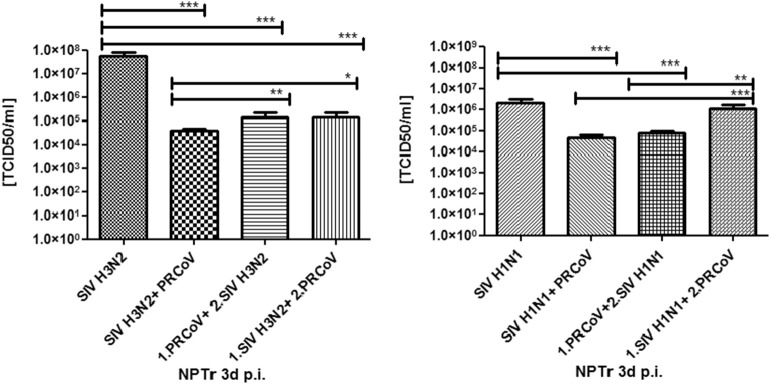
Finally, NPTr cell supernatants were titrated to compare mono- and co-infection by PRCoV and SIV H3N2 or SIV H1N1 with the infection of PCLS at 3d post infection. Interestingly, also the supernatant of the NPTr cells showed a higher virus titer of cells infected solely by PRCoV compared to co-infections (Fig. 8 ). This difference was significant for all co-infection groups with SIV H1N1 (Fig. 8). In SIV H3N2 co-infection groups this difference in titer only was significant for PRCoV + SIV H3N2 compared to PRCoV mono-infection (Fig. 8). Differences in virus titers between the groups of SIV H3N2 in NPTr cell co-infections were determined for 1.SIV H3N2 + 2.PRCoV vs. 1.PRCoV + 2.SIV H3N2 (p = 0.0051) and PRCoV + SIV H3N2 vs. 1.SIV H3N2 + 2.PRCoV (p = 0.0039). In contrast to this, co-infection groups of SIV H1N1 did not show any difference on NPTr cells. Additionally MDCKII cells were used to measure SIV titers. Here, SIV H3N2 mono-infection showed the highest measured titer of 5.56 × 107 TCID50/mL compared to all co-infections as well as SIV H1N1 mono-infection (Fig. 9 ). Cells infected by SIV H1N1 demonstrated again a significant higher virus titer compared to the corresponding co-infections (Fig. 9). Only 1.SIV H1N1 + 2.PRCoV had a similar virus titer to SIV H1N1 mono-infection. Other co-infection groups had a significant lower titer.
Fig. 8.
Endpoint dilution titration of NPTr cell culture supernatant 3 d p.i. on NPTr cells. Comparison of mono- and co-infection by PRCoV and SIV H3N2 (left), or SIV H1N1 (right). *p < 0.05, **p < 0.025, ***p < 0.001.
Fig. 9.
Endpoint dilution titration of NPTr cell supernatant 3 d p.i. on MDCK II cells. Comparison of mono- and co-infection by PRCoV and SIV H3N2 (left), or SIV H1N1 (right). *p < 0.05, **p < 0.025, ***p < 0.001.
This study illustrated that co-infection of PCLS or NPTr cells by PRCoV and SIV H3N2/H1N1 did not cause any further reduction of ciliary activity, or accumulation of nucleoprotein in NPTr cells, nor higher virus titers in the supernatant of PCLS or NPTr cells compared to single infection. The comparison of mono- and co-infection of PCLS showed a restriction of virulence for each virus species when administered simultaneously. PRCoV as well as SIV H3N2 or SIV H1N1 in mono-infection showed in almost all combinations a significant higher titer than co-infections. Random differences were measured between the co-infection groups. Co- infection of PRCoV + SIV H3N2 vs. 1.SIV H3N2 + 2.PRCoV showed significant lower titer (p = 0.0112). Similar results were measured for the same co-infection combination of SIV H1N1 instead of SIV H3N2 (p = 0.001). All titers measured for co-infection groups never exceeded mono-infection titers.
4. Discussion
In the present study it was shown that PCLS can be used as an infection model for PRCoV, as well as for co-infection studies with SIV H3N2/H1N1. PRCoV showed on the one hand only limited ability in reduction of ciliary activity, but on the other hand higher titers in PCLS supernatants than the co-infection with porcine influenza viruses.
Measuring the ciliary activity is mostly limited to the conditions of the PCLS themselves. This was seen in control slices that dropped in ciliary activity after > 4 days, similar to earlier studies (Meng et al., 2013, Punyadarsaniya et al., 2011). This may be caused by the fact that the medium was not changed. However, there were obvious differences from uninfected to infected PCLS at similar time points. SIV H3N2 ciliary activity showed a concrete reduction, comparable to another study done with the same SIV strain (Punyadarsaniya et al., 2011). SIV H1N1 however, revealed a more reduced ciliary activity than shown before by the same strain (Meng et al., 2013). This effect may be explained by a slightly higher titer used in this study for infection of the slices. Single infection by PRCoV had the lowest effect on ciliary activity over time compared to all other mono- and co-infections. No differences between the SIV strains and their co-infections were visible concerning PCLS ciliary activity.
In contrast to the minor reduction of ciliary activity by PRCoV are the virus titers in PCLS supernatants analyzed on NPTr cells. PCLS mono-infected by PRCoV displayed higher virus titers compared to co-infections with SIV H3N2. Same tendencies were measured for co-infections with SIV H1N1, even though this was only significant for co-infection starting with PRCoV. Influenza virus titers in the PCLS supernatant compared on MDCKII cells did not reveal any differences to combined infections. In conclusion, coronaviruses seemed to be suppressed by the co-infection with the SIVs in PCLS. Moreover, influenza virus infection on the PCLS was not influenced by co-infections with PRCoV.
Fluorescence microcopy of infected NPTr cells indicated that PRCoV was not able to replicate within the cells to the same level as SIV H3N2 or SIV H1N1, even though all different virus strains were inoculated with the same MOI and analyzed at 3 days post infection. The amount of PRCoV infected cells did not differ between the mono- and co-infections. In contrast there was a difference between mono- or co-infected cells by SIV H3N2/H1N1. In NPTr cells the SIVs seemed to be influenced negatively by PRCoV. Furthermore, only few cell co-infections by overlapping antigen staining were detected in PRCoV and SIV infected cells.
Titration of SIV H3N2 as well as SIV H1N1 on MDCKII cells showed higher titers from SIV single infected NPTr cells. That means, that SIV H3N2 and SIV H1N1 virus titers were reduced due to PRCoV co-infection. Finally PCLS as well as porcine cell cultures of respiratory origin disclosed a clear interference between PRCoV and SIV H3N2 as well as SIV H1N1 when combined.
Earlier studies involving mono- and co-infection with PRCoV and SIV H1N1 or SIV H3N2 in vivo illustrated results that pointed in the same direction (Lanza et al., 1992). Pathogenesis was compared mainly by clinical assessment, necropsy findings in the lung and virus isolation by nasal swaps and tissue samples over time (Lanza et al., 1992). Comparing co-infection of simultaneously given viruses to mono-infection showed no increase in respiratory symptoms or lung lesions (Lanza et al., 1992). Mean duration of excreted influenza virus was shorter in dual than in single-infected pigs (Lanza et al., 1992). Interestingly, in tissues of mono-infected swine with PRCoV, the virus was isolated for a longer period of time than by co-infections with SIV H3N2/H1N1 (Lanza et al., 1992). This proves some interesting overlap to our results showing lower virus titers in co-infected PCLS compared to the mono-infection with PRCoV. Simultaneously, no enhanced or even lower pathogenicity was detected by co-infection of the swine compared to mono-infection (Lanza et al., 1992).
Both the corona- and influenza viruses were reduced in virus titers when combined in PCLS as well as in NPTr cells. This indicates that the viruses target roughly the same cell types, even though dissimilar cell receptors are used for cell entry. It seems that after entry of one virus species the cell becomes refractory for infection with the remaining other virus species resulting in lower infection rates. One explanation for this negative mutual interference might be the blockage or steric hindrance of cellular receptors by the first interacting virus. Furthermore, innate immune responses influence virus replication and may lead to a reduction in virus titers after co-infection with both virus species. Induction of intracellular signaling cascades by RNA viruses results in the activation of transcription factors, which regulate the expression of abundant other genes, such as interferons (IFN) and IFN-stimulated genes, as well as pro-inflammatory cytokines and chemokines (Katze et al., 2008).
Several cell mechanisms are linked to IFN induction connected to influenza A viruses. Broadly studied IFN induced proteins, are Mx proteins influencing influenza A virus infection. Mx proteins are dynamin-like large GTPases that are highly induced by IFN α and β, but are not constitutively present in normal cells (Haller and Kochs, 2002, Zimmermann et al., 2011). Infection of PCLS with SIVs may cause Mx protein activation. Therefore, the PCLS system might be used to analyze the role of Mx proteins in porcine respiratory infection. Influenza strains differ in their sensitiveness to antiviral effects of Mx proteins (Zimmermann et al., 2011). This does have an impact on virus replication and pathogenic outcome and could also be a reason why on the one hand co-infections are not as successfully in viral replication than mono-infection of PCLS, but on the other hand why different SIVs also cause different amounts in virus titers.
Coronaviruses like PRCoV also induce early IFN-α immune responses (Jung et al., 2009). Co-infection studies with PRRSV and PRCoV tested in vivo in swine showed that ongoing PRRSV infection with subsequent PRCoV infection increased clinical illness, as well as lymphadenopathy as well as pulmonary disease (Jung et al., 2009). It could be shown that PRRSV in contrast to PRCoV suppresses early IFN induced immune modulatory effects and therefore enhanced PRCoV pathogenic outcome due to preliminary infection (Jung et al., 2009). In context of these studies, a suppressed activation of IFN innate immune responses can increase viral pathogenesis and replication in the respiratory tissue. Pre-infection with PRCoV had in contrast no effect on PRRSV infection (Jung et al., 2009).
5. Conclusion
The porcine respiratory coronavirus was able to infect porcine PCLS. The effect on ciliary activity by PRCoV was low compared to SIV mono-infection and co-infection groups. The infectious titers of co-infection groups with PRCoV and SIV H3N2 or SIV H1N1 were never higher, but in most cases lower than titers of mono-infected PCLS or NPTr cells. A clear restriction of virulence by both the coronavirus as well as influenza A viruses was detected. This is in accordance to earlier in vivo studies investigating PRCoV and SIV co-infection. The underlying mechanism that causes a restriction in virulence by co-infection with different RNA viruses remains to be investigated. Finally, PCLS are a promising tool to analyze the potential of viral co-infection in swine.
Acknowledgements
Financial support was provided by a grant to C.S.-W. (SCHW 1408/1-1) from the German Research Foundation (DFG). C.S.-W. was funded by the Emmy Noether Programme from the DFG.
This work was performed by TK in partial fulfillment of the requirements for a Dr. rer. nat. degree from the University of Veterinary Medicine Hannover.
We acknowledge the support of the Institute for Physiology and the Clinic for Swine at the University of Veterinary Medicine Hannover for providing swine lung. We thank S. Uhlenbruck for technical assistance and L. Enjuanes, R. Dürrwald, and M. Schmitzke for providing viruses.
References
- Abdull Razis A.F., Bagatta M., De Nicola G.R., Iori R., Ioannides C. Up-regulation of cytochrome P450 and phase II enzyme systems in rat precision-cut rat lung slices by the intact glucosinolates, glucoraphanin and glucoerucin. Lung Cancer. 2011;71:298–305. doi: 10.1016/j.lungcan.2010.06.015. [DOI] [PubMed] [Google Scholar]
- Banerjee A., Trivedi C.M., Damera G., Jiang M., Jester W., Hoshi T., Epstein J.A., Panettieri R.A., Jr. Trichostatin A abrogates airway constriction, but not inflammation, in murine and human asthma models. Am. J. Respir. Cell Mol. Biol. 2012;46:132–138. doi: 10.1165/rcmb.2010-0276OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard S., Bottreau E., Aynaud J.M., Have P., Szymansky J. Natural infection with the porcine respiratory coronavirus induces protective lactogenic immunity against transmissible gastroenteritis. Vet. Microbiol. 1989;21:1–8. doi: 10.1016/0378-1135(89)90013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgueil E., Hutet E., Cariolet R., Vannier P. Experimental infection of pigs with the porcine respiratory coronavirus (PRCV): measure of viral excretion. Vet. Microbiol. 1992;31:11–18. doi: 10.1016/0378-1135(92)90136-H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun A., Tschernig T. Animal models of asthma: innovative methods of lung research and new pharmacological targets. Exp. Toxicol. Pathol. 2006;57(Suppl. 2):3–4. doi: 10.1016/j.etp.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Castrucci M.R., Donatelli I., Sidoli L., Barigazzi G., Kawaoka Y., Webster R.G. Genetic reassortment between avian and human influenza A viruses in Italian pigs. Virology. 1993;193:503–506. doi: 10.1006/viro.1993.1155. [DOI] [PubMed] [Google Scholar]
- Cox E., Hooyberghs J., Pensaert M.B. Sites of replication of a porcine respiratory coronavirus related to transmissible gastroenteritis virus. Res. Vet. Sci. 1990;48:165–169. doi: 10.1016/S0034-5288(18)30984-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmas B., Gelfi J., L'Haridon R., Vogel L.K., Sjostrom H., Noren O., Laude H. Aminopeptidase N is a major receptor for the entero-pathogenic coronavirus TGEV. Nature. 1992;357:417–420. doi: 10.1038/357417a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doms R.W., Gething M.J., Henneberry J., White J., Helenius A. Variant influenza virus hemagglutinin that induces fusion at elevated pH. J. Virol. 1986;57:603–613. doi: 10.1128/jvi.57.2.603-613.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari M., Scalvini A., Losio M.N., Corradi A., Soncini M., Bignotti E., Milanesi E., Ajmone-Marsan P., Barlati S., Bellotti D., Tonelli M. Establishment and characterization of two new pig cell lines for use in virological diagnostic laboratories. J. Virol. Methods. 2003;107:205–212. doi: 10.1016/s0166-0934(02)00236-7. [DOI] [PubMed] [Google Scholar]
- Gambaryan A.S., Karasin A.I., Tuzikov A.B., Chinarev A.A., Pazynina G.V., Bovin N.V., Matrosovich M.N., Olsen C.W., Klimov A.I. Receptor-binding properties of swine influenza viruses isolated and propagated in MDCK cells. Virus Res. 2005;114:15–22. doi: 10.1016/j.virusres.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Goris K., Uhlenbruck S., Schwegmann-Wessels C., Kohl W., Niedorf F., Stern M., Hewicker-Trautwein M., Bals R., Taylor G., Braun A., Bicker G., Kietzmann M., Herrler G. Differential sensitivity of differentiated epithelial cells to respiratory viruses reveals different viral strategies of host infection. J. Virol. 2009;83:1962–1968. doi: 10.1128/JVI.01271-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y., Shortridge K.F., Krauss S., Li P.H., Kawaoka Y., Webster R.G. Emergence of avian H1N1 influenza viruses in pigs in China. J. Virol. 1996;70:8041–8046. doi: 10.1128/jvi.70.11.8041-8046.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller O., Kochs G. Interferon-induced mx proteins: dynamin-like GTPases with antiviral activity. Traffic (Copenhagen, Denmark) 2002;3:710–717. doi: 10.1034/j.1600-0854.2002.31003.x. [DOI] [PubMed] [Google Scholar]
- Jung K., Alekseev K.P., Zhang X., Cheon D.S., Vlasova A.N., Saif L.J. Altered pathogenesis of porcine respiratory coronavirus in pigs due to immunosuppressive effects of dexamethasone: implications for corticosteroid use in treatment of severe acute respiratory syndrome coronavirus. J. Virol. 2007;81:13681–13693. doi: 10.1128/JVI.01702-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung K., Renukaradhya G.J., Alekseev K.P., Fang Y., Tang Y., Saif L.J. Porcine reproductive and respiratory syndrome virus modifies innate immunity and alters disease outcome in pigs subsequently infected with porcine respiratory coronavirus: implications for respiratory viral co-infections. J. Gen. Virol. 2009;90:2713–2723. doi: 10.1099/vir.0.014001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katze M.G., Fornek J.L., Palermo R.E., Walters K.-A., Korth M.J. Innate immune modulation by RNA viruses: emerging insights from functional genomics. Nat. Rev. Immunol. 2008;8:644–654. doi: 10.1038/nri2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchhoff J., Uhlenbruck S., Goris K., Keil G.M., Herrler G. Three viruses of the bovine respiratory disease complex apply different strategies to initiate infection. Vet. Res. 2014;45:20. doi: 10.1186/1297-9716-45-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchhoff J., Uhlenbruck S., Keil G.M., Schwegmann-Wessels C., Ganter M., Herrler G. Infection of differentiated airway epithelial cells from caprine lungs by viruses of the bovine respiratory disease complex. Vet. Microbiol. 2014;170:58–64. doi: 10.1016/j.vetmic.2014.01.038. [DOI] [PubMed] [Google Scholar]
- Kuntz-Simon G., Madec F. Genetic and antigenic evolution of swine influenza viruses in Europe and evaluation of their zoonotic potential. Zoonoses Public Health. 2009;56:310–325. doi: 10.1111/j.1863-2378.2009.01236.x. [DOI] [PubMed] [Google Scholar]
- Lanza I., Brown I.H., Paton D.J. Pathogenicity of concurrent infection of pigs with porcine respiratory coronavirus and swine influenza virus. Res. Vet. Sci. 1992;53:309–314. doi: 10.1016/0034-5288(92)90131-K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marozin S., Gregory V., Cameron K., Bennett M., Valette M., Aymard M., Foni E., Barigazzi G., Lin Y., Hay A. Antigenic and genetic diversity among swine influenza A H1N1 and H1N2 viruses in Europe. J. Gen. Virol. 2002;83:735–745. doi: 10.1099/0022-1317-83-4-735. [DOI] [PubMed] [Google Scholar]
- Meng F., Punyadarsaniya D., Uhlenbruck S., Hennig-Pauka I., Schwegmann-Wessels C., Ren X., Durrwald R., Herrler G. Replication characteristics of swine influenza viruses in precision-cut lung slices reflect the virulence properties of the viruses. Vet. Res. 2013;44:110. doi: 10.1186/1297-9716-44-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punyadarsaniya D., Liang C.H., Winter C., Petersen H., Rautenschlein S., Hennig-Pauka I., Schwegmann-Wessels C., Wu C.Y., Wong C.H., Herrler G. Infection of differentiated porcine airway epithelial cells by influenza virus: differential susceptibility to infection by porcine and avian viruses. PLoS One. 2011;6 doi: 10.1371/journal.pone.0028429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasschaert D., Gelfi J., Laude H. Enteric coronavirus TGEV: partial sequence of the genomic RNA, its organization and expression. Biochimie. 1987;69:591–600. doi: 10.1016/0300-9084(87)90178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasschaert D., Duarte M., Laude H. Porcine respiratory coronavirus differs from transmissible gastroenteritis virus by a few genomic deletions. J. Gen. Virol. 1990;71(Pt 11):2599–2607. doi: 10.1099/0022-1317-71-11-2599. [DOI] [PubMed] [Google Scholar]
- Richardson J.C., Scalera V., Simmons N.L. Identification of two strains of MDCK cells which resemble separate nephron tubule segments. Biochim. Biophys. Acta. 1981;673:26–36. [PubMed] [Google Scholar]
- Siddell S.G., Anderson R., Cavanagh D., Fujiwara K., Klenk H.D., Macnaughton M.R., Pensaert M., Stohlman S.A., Sturman L., van der Zeijst B.A. Coronaviridae. Intervirology. 1983;20:181–189. doi: 10.1159/000149390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel V. Caister Academic Press; Norfolk, UK: 2007. Coronaviruses: Molecular and Cellular Biology. [Google Scholar]
- Van Reeth K., Pensaert M.B. Porcine respiratory coronavirus-mediated interference against influenza virus replication in the respiratory tract of feeder pigs. Am. J. Vet. Res. 1994;55:1275–1281. [PubMed] [Google Scholar]
- Wu N.H., Yang W., Beineke A., Dijkman R., Matrosovich M., Baumgartner W., Thiel V., Valentin-Weigand P., Meng F., Herrler G. The differentiated airway epithelium infected by influenza viruses maintains the barrier function despite a dramatic loss of ciliated cells. Sci Rep. 2016;6:39668. doi: 10.1038/srep39668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann P., Manz B., Haller O., Schwemmle M., Kochs G. The viral nucleoprotein determines Mx sensitivity of influenza A viruses. J. Virol. 2011;85:8133–8140. doi: 10.1128/JVI.00712-11. [DOI] [PMC free article] [PubMed] [Google Scholar]