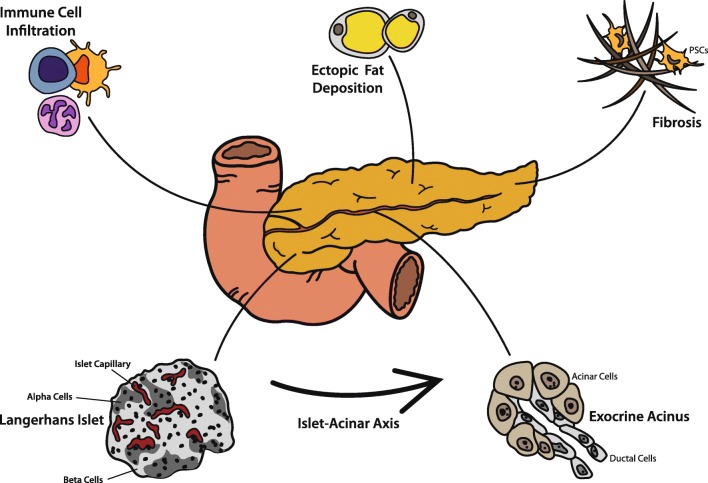
Fig. 2.
Contributing factors to exocrine pancreatic insufficiency in patients with diabetes. Due to portal vessels supplying exocrine acini with the secretome of endocrine islets, acinar cells are under endocrine control, in the short-term for well-regulated upregulation of pancreatic enzyme secretion and in the long-term for trophic control of both acinar cells and ductal cells. Overall and with time, the pancreata in patients with type 1 or type 2 diabetes get atrophic and exocrine function declines. Islet microvasculature might be affected by diabetic microangiopathy, and diabetic neuropathy is also discussed to influence this islet-acinar axis (not depicted specifically in this figure). Immune cell infiltration (mainly CD8+, CD4+, and CD11c+ cells) and autoantibodies targeting the exocrine compartment are frequently found in both type 1 and in type 2 diabetes. A rise in collagen deposition and loss of extracellular matrix remodeling facilitated by activated pancreatic stellate cells (PSCs) lead to an increased rate of pancreatic fibrosis in patients with diabetes. Additionally, ectopic fat accumulation has been discussed to contribute to development of EPI, however, data from the literature are controversial