Abstract
Hospital and healthcare facilities have diverse indoor environment due to the different comfort and health needs of its occupants. Currently, most ventilation studies revolve around specialised areas such as operating rooms and isolation rooms. This paper focuses on the ventilation of multiple-bed hospital wards in the tropical climate, taking into account the design, indoor conditions and engineering controls. General ward layouts are described briefly. The required indoor conditions such as temperature, humidity, air movements and indoor air quality in the ward spaces are summarized based on the current guidelines and practices. Also, recent studies and engineering practices in the hospital indoor environment are elaborated. Usage of computational fluid dynamics tools for the ventilation studies is discussed as well. As identified during the review, there is an apparent knowledge gap for ventilation studies in the tropics compared with temperate climates, as fact studies have only been published for hospital wards in countries with a temperate climate. Therefore, it is highlighted that specific tropical studies along with novel engineering controls are required in addressing the ventilation requirements for the tropics.
Keywords: Hospital wards, Indoor air quality, Engineering control, Numerical method, Tropical climates
Abbreviations: ACH, air changes per hour; ASHRAE, American society of heating, refrigerating and air-conditioning engineers; CDC, centers for disease control; CFD, computational fluid dynamic; HCW, healthcare workers; HEPA, high efficiency particulate air; HICPAC, healthcare infection control practices advisory committee; IAQ, indoor air quality; MRSA, methicillin-resistant Staphylococcus aureus; RANS, Reynolds averaged Navier–Stokes; RNG, re-normalisation group; SARS, severe acute respiratory syndrome; SBS, sick building syndrome; UV, ultraviolet; UVGI, ultraviolet germicidal irradiation; WHO, World Health Organization
1. Introduction
Hospital and healthcare facilities have diverse indoor environments due to the varying needs of patients and healthcare workers. The indoor environments range from a simple general practitioners’ room to an operating room. Furthermore, the recent pandemic of influenza creates the maximum likelihood for airborne transmission by congregating communicable and vulnerable individuals in healthcare facilities.
At this time, ventilation in healthcare facilities is important as it provides thermal comfort and protection from harmful emissions or airborne pathogenic materials to both patients and healthcare workers [1]. Typically, the ventilation requirements for spaces are governed by building codes, regulations and specific guidelines furnished by the local health authorities and others [2], [3], [4], [5]. These requirements vary by country, depending on the geographic location, economic background and the country’s specific needs.
The benefits of environmental control for isolation wards and operating room theatres have been recorded and analysed thoroughly. However, there is a lack of ventilation studies on open ward facilities, which is where most patients are placed, especially in the tropics. Recent outbreaks of pandemic diseases have heightened the risks associated with these facilities. Thus, in this paper, the current state of knowledge of the ventilation of multiple-bed hospital wards is reviewed.
2. Ventilation in healthcare facilities
By and large, the purpose of ventilation in any occupied space is to provide fresh air to the occupants and remove heat generated within a confined space. In healthcare facilities, the ventilation system should also help prevent diseases and treat patients.
Research has shown that the design characteristics of a healthcare facility, which include ventilation and layout improvements, can enhance the health outcome of the patients and provide a better working environment for employees [6]. Therefore, overall healthcare quality can be partly enhanced by improving the ventilation.
Many reports have shown that infectious diseases occur due to airborne transmission and surface contaminations by droplet nuclei. This topic is further elaborated in Section 6. Transmission of Severe Acute Respiratory Syndrome (SARS) has been documented in different circumstances and locations worldwide and is found to be highly communicable in healthcare settings [7], [8]. Airborne transmissions are not only limited to the SARS episode but also extend to nosocomial infections, which are more prevalent in healthcare settings, such as open wards and intensive care units [9], [10]. Apart from this, ventilation systems were also identified as a source of infection; in some cases, the systems were harbouring infectious pathogens [11], [12].
Recent literature has established a relationship between ventilation and health outcomes. In 2006, an interdisciplinary panel consisting of experts in medicine, epidemiology, toxicology, environmental chemistry, aerosol sciences, psychology, engineering and architecture reviewed the effects of ventilation on health in non-industrial indoor environments [13]. The group judged that 27 of the total 365 papers studied concurred that ventilation rates are associated with sick building syndrome (SBS), especially in offices. Furthermore, the group also highlighted the need for ventilation and health studies in warm and humid climates and polluted and public localities. Moreover, a list of 40 studies between 1960 and 2005 were appraised by another multidisciplinary panel. Subsequently, they also recognised that 10 studies have put forward substantial facts that show the relationship between ventilation and proliferation of infectious diseases, such as influenza and TB [14].
Healthcare workers, such as doctors, nurses and others, are exposed to infectious diseases and demanding work conditions in healthcare settings [7], [15]. Cases of transmission of contagions from patients and surface contaminations have been recorded. The risk of transmission is also increased by various environmental factors. Guidelines indicating the risks and control measures have been compiled in [2]. Several other studies have deliberated the risks of SBS in the healthcare environment, which are compiled in the 2003 Guidelines for Environmental Infection Control in Healthcare Facilities by the US Centers for Disease Control and Prevention (CDC) and the Healthcare Infection Control Practices Advisory Committee (HICPAC) [6].
Briefly, ventilation in healthcare facilities has a profound effect on the well-being of patients and employees in healthcare facilities. Thus, this paper focuses on the ventilation of multiple-bed hospital wards, including the design, indoor conditions and engineering controls.
3. General design
Multiple-bed hospital ward is a generic term used to describe the concept of a non-partitioned area that contains several beds for patients who need a similar kind of care at a healthcare facility [16], [17], [18]. The number of beds in a ward differs from one facility to another. Therefore, the configuration of a multiple-bed hospital ward can range from 2 people per ward up to 30 people per ward in many localities, including Malaysia. Additionally, it is not uncommon to subdivide the ward into multiple units that hold 4 patients or up to 6 patients. Another practice is to have 1 patient per room as stipulated in [5], which is particularly common in the United States. However, multiple-bed configurations with defined limitations are allowed for the intensive care unit and critical care unit. Compared with other clinical spaces such as operating rooms and isolation rooms, which are studied thoroughly, the aforementioned spaces are limited to one person and a few healthcare workers, such as doctors and nurses. Depending on the activities conducted and the affected floor area of a ward, these spaces are much more constrained compared with operating theatres. Furthermore, multiple-bed hospital wards require lower capital expenditure, which is why they are more widely used in developing countries compared with single-patient rooms.
Basic ward design principles revolve around lighting, ventilation and cleanliness [19], [20]. The ward environment should be focused on the needs of patients and staff [21], [22]. Recent studies have implied the significance of meaningful and varying stimuli (odourless and pleasant experience) in a ward environment, suggesting links between physical environments to patients’ health outcomes. These conclusions support the idea that poorly designed or maintained hospital wards may displease patients and thus promote sickness in patients rather than assist the healing process [6].
Typically, the following are the four types of hospital ward designs being utilised throughout the world [16], [18], [22]: bay wards (Fig. 1 ), nightingale wards (Fig. 2 ), racetrack wards and hub and spoke units. The nightingale wards have beds along the perimeter of the space, with the nurses’ station located centrally. This allows the nurses to maximise their supervision of patients. This type of ward caters up to 30 adults or 24 children and is still widely used in many developing countries. Bay wards have a central nurses’ station and cubicle rooms, which house several beds. Racetrack wards are a variant of the bay wards as they have a different arrangement for the nurses’ station and beds. The hub and spoke units have the central nurses’ station as a hub and large rooms as radiating spokes.
Fig. 1.
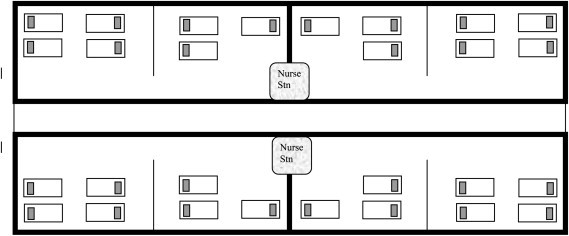
Bay wards arrangement.
Fig. 2.
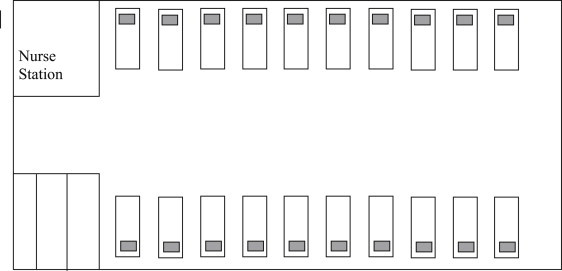
Nightingale wards arrangement.
Nursing activities and patient welfare are also influenced by ward designs [23]. Overall, racetrack wards have higher nursing quality scores (80%) and the lowest bed cost (£54), compared with other types of wards.
4. Tropical climate characteristics
Tropics are regions on earth by the equator between 23.5° North latitude and 23.5° South latitude. Temperatures are above 18 °C and with high precipitation throughout the year. Tropical climate is further subdivided to tropical savannah, tropical monsoon and tropical rainforest, distinguished by the amount of precipitation. Seasonal changes in the tropics are dominated by the movement of rain belts, resulting in a dry and wet seasons, rather than the various temperatures and day length of spring, summer, autumn and winter, which are experienced in the temperate climate. Temperature extremes are not uncommon in temperate climate areas. However, it may only be experienced in certain regions only [24].
These outdoor conditions of the tropics have primary influence on the outdoor fresh air indoor to the indoor space. It would be reflected on the equipment selection and sizing of the ventilation and air-conditioning system. Furthermore, thermal comfort requirement of the residents in the tropics would also be dictated by their long term conditioning to the climates.
5. Indoor conditions
Firstly, indoor conditions for healthcare facilities, such as operating rooms, isolation rooms and nursing wards, are particularly more stringent compared with other institutional buildings [1] and must also provide clean air to prevent and treat diseases.
Secondly, the healthcare workers’ comfort should be considered, and a safe working area should be ensured. Cases have been recorded where contagions have been transmitted from patients to healthcare workers [7]. In Hanoi, Vietnam, transmission rates were recorded to be up to 47.4% among nurses working in general wards, which emphasised the vulnerability of hospital workers to contagious diseases. Moreover, hospital-acquired infections become significant healthcare costs that use additional hospital days and resources. These concerns can be balanced with appropriate engineering controls in ventilation systems, which would enhance the healthcare system.
Indoor conditions encompass several criteria, including temperature, humidity, air movements and indoor air quality (IAQ). Each of these will be further elaborated in subsequent sections.
5.1. Temperature
The temperature of the environment within the healthcare facility should meet the thermal comfort requirements of the occupants, especially the patients. One point to consider is that their body temperature regulatory functions are damaged as a result of their conditions. Also, having a pleasant atmosphere assists in healing and soothes their moods. Hence, a desirable temperature should be maintained at satisfactory comfort conditions.
The desirable temperature range differs from one type of ward facility to another, according to the international guidelines and standards (Table 1 ). In the United States, guidelines are provided by ASHRAE [1], whereas in the UK, the guidelines are provided through publications, such as CIBSE Guides and the Health Technical Memorandum to assist engineers [4], [25]. However, in the tropics, similar guidelines are not available, and the aforementioned guidelines are referred to widely.
Table 1.
Comparison between guidelines and codes used in the tropics.
| Patient rooms | |||||
|---|---|---|---|---|---|
| References | Design temperature (F) | Relative humidity (%) | Minimum total air change rate (ACH) | Minimum outdoor air change rate (ACH) | Pressure relationship to adjacent room |
| ASHRAE handbook | 75 | 30 (Winter), 50 (Summer) | 4 | 2 | Neutral |
| AIA guidelines | 70–75 | Not specified | 6 | 2 | Not specified |
| CIBSE guide B | 72–75 (Winter); 77 (Summer) | 40–70 | 6 | Not specified | Not specified |
| HTM 2025 guidelines | 68–72 | 40–60 | Not specified | Not specified | Neutral |
| ASHRAE manual | 70–75 | 30–60 | 6 | 2 | Not specified |
| Intensive care rooms | |||||
| References | Design temperature (F) | Relative humidity (%) | Minimum total air change rate (ACH) | Minimum outdoor air change rate (ACH) | Pressure relationship |
| ASHRAE handbook | 75–80 | 30–60 | 6 | 2 | Positive |
| AIA guidelines | 70–75 | 30–60 | 6 | 2 | Not specified |
| CIBSE guide B | Not specified | Not specified | Not specified | Not specified | Not specified |
| HTM 2025 guidelines | 68–72 | 30–60 | Not specified | Not specified | Neutral |
| ASHRAE manual | Not specified | Not specified | Not specified | Not specified | Not specified |
One may also say that it is impossible to satisfy the total comfort of all the occupants in terms of indoor thermal conditions. Comfort also depends on occupants’ clothing, activity and air movements. In addition to these variables, patients’ physical strength also influences their thermal comfort needs. A study by Hwang et al. [26] has shown the dissimilarity in thermal comfort perception and comfort range against the ASHRAE Standard 55. More than 75% of the respondents were neutral in their preferences, even when there was only a 40% conformance to ASHRAE recommendations of comfort zone. This view is also consistent with the findings of Nicol [27] and Mallick [28]. Nicol [27] presented evidence and methods that complement existing standards, such as ISO 7730, using adaptive thermal comfort standards derived from local subjective measurements. With this criterion, the comfort range can be above or below 2–3 °C of the optimal figure and be considered satisfactory. In addition, Mallick [28] suggested that for people in a warm humid climate, comfort perceptions are governed by local acclimatisation to high temperatures and humidity. As a result from his study, the comfort temperature range is between 24 °C and 32 °C with relative humidity values between 50% and 90% with or without air movements in the selected space.
Ultimately, in terms of temperature, the thermal comfort requirement for a patient population is different from that of a healthy population. Note that in the study conducted by Hwang et al. [26], the preference temperature in summer season is higher than thermal neutrality for patients in the range of 0.4–0.6 °C, but lower for the healthy population at 0.8–1.0 °C.
5.2. Humidity
In addition to temperature and air movement, humidity is another internal climate characteristic. Room hygiene and thermal comfort levels are very much related to humidity levels.
The desirable ranges of humidity are also furnished in Table 1, according to the international guidelines and standards. Also, humidity levels have some bearing on thermal comfort levels. Yu et al. [29] showed that in a tropical climate, the humidity level is a governing factor in the variations of thermal sensations when subjects are exposed to an almost constant room temperature of 23 °C and a room average velocity of 0.07 m/s. However, certain medical conditions require an extreme level of temperature and relative humidity to assist in the healing process. For example, in a burn unit, a temperature of 32 °C and a relative humidity of 95% may be required so the patient does not lose bodily fluids. Similarly, it was found that a temperature of 32 °C and a relative humidity of 35% have positive effects when treating certain arthritis conditions [30].
Humidity levels also influence the growth and transfer of airborne microorganisms. Additionally, high humidity levels result in moisture being absorbed in building materials, which supports microbial growth [10]. Studies have indicated that humidity level influences the survival rates of microorganisms. Humid conditions also may increase the settling rate of aerosols due to the heavy droplets become dry and remain suspended in the air for a longer duration. Mucus coatings on special tissues in respiratory tracts can become dry in extreme dry conditions, which functions to capture particles prior to being breathed deep into the lungs. In addition, high humidity level exceeding 60% in the operating room can result in sweating for patients. This would pose further infection risks for patients [31].
5.3. Air movement and distributions
Air movement and distribution is another indoor condition that needs attention. Airflow pattern is a significant factor affecting the needs of staff and patients in a ward. For instance, droplet transport from patients’ respiratory activities is closely related to airflow patterns. In addition, airflow patterns will also affect the thermal comfort of both the staff and patients.
Typically, there are two types of ventilation systems practised in hospital wards, namely the mixing type and displacement type. The former supplies air along the perimeter surface of the space, and air is later extracted by the perimeter outlets, as shown in Fig. 3 . Air movement is due to momentum flows from the outlet diffusers and temperature differences. The air distributions can also be enhanced using a different type of outlet arrangement, such as downward ventilation and horizontal airflow. In contrast, the latter supplies air in the most direct way possible to the occupied zone, as illustrated in Fig. 4 [32].
Fig. 3.
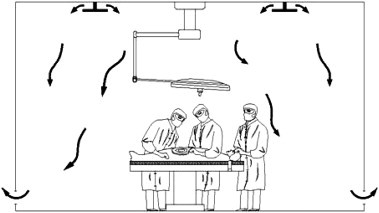
Mixing ventilation.
Fig. 4.
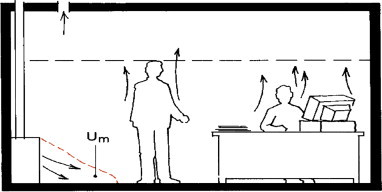
Displacement ventilation [31].
Three different ventilation systems were compared for a two-bed hospital ward in a recent study. The results have recommended that mixing and downward ventilation systems to be used in hospital wards with multiple beds, where droplet nuclei are well mixed. On the other hand, displacement ventilation is not recommended due to possibility of high exposure level from patients’ exhaled droplet nuclei towards other patients and HCWs. It was also concluded that thermal stratification locking contributes to the concentrated layer of exhaled droplet nuclei in displacement ventilation. The study has also shown that bed distances of up to 1.0 m do not make any significant impact on the personal exposure level of the pollutant released from one bed to another. It can be summarized that mixing ventilation and downward ventilation is more effective than displacement ventilation for minimizing the infection risks [33].
Thermal comfort perception is also affected by the local air movements, metabolic rate and an occupant’s clothing. A local air speed of 0.25 m/s or less is considered comfortable for occupants. Differences in metabolic rates and clothing between patients and hospital staffs would also result in dissimilar perceptions and requirements.
Memarzadeh and Manning [34] evaluated the efficacy of a ventilation system with a multitude of arrangements of air outlets, seasons and ventilation rates in a typical single-patient room by calculating the various ventilation indices. The results showed that a ventilation rate of 4 ACH provides an adequate condition and can be optimised with 5 or 6 ACH. Moreover, a concurrent study conducted on isolated rooms also recommended using 6 ACH for the thermal comfort of patients.
In addition to comfort concerns, the ventilation system should also be used to maintain conditions within the spaces or maintain the pressure differential between spaces according to regulatory requirements. Satisfying this condition will stop the spread of airborne pollutants between rooms as much as possible. For example, protective isolation rooms are required to be negative pressure rooms [1], [2], [5]. A negative pressure room includes a ventilation system that facilitates airflows from the corridors into the negative pressure room, ensuring that polluted air shall not leak out from the isolation room to another hospital space, as shown in Fig. 5 .
Fig. 5.
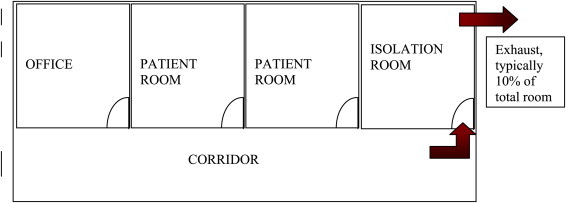
Negative pressurisation relationship.
An operating theatre ventilation system has been researched widely in terms of room layout, pressurisation and air distributions to create ultra-clean ventilation from laminar airflow systems [35], [36]. Operating theatre areas are prone to surgical site infection risks caused by airborne bacteria, which subsequently led to the current technical standards, such as the Health Technical Memorandum and microbial measurement tools [37]. Additionally, clean room technology standards are being recommended to select the bacterial threshold limits in operating rooms [38]. Ho et al. [39] presented a three-dimensional analysis for pollutant removal and thermal comfort in an operating room where air flows from high sidewall grilles and is exhausted through low sidewall grilles on the opposed walls. Consequently, supply grilles, which are located at the centre of the room, showed better effectiveness. This result again confirmed that airflow patterns substantially influence the efficacy of thermal comfort and pollutant removals. Furthermore, Rui et al. [40] established the critical outlet velocities in an operating room; exceeding the critical outlet velocity increases bacteria deposits, especially in upper surfaces.
Alternatives, such as a horizontal airflow system, have been investigated and showed good performance in removing pollutants [41]. Qian et al. [42] carried out a full-scale experiment of a general hospital ward to examine the feasibility of a downward ventilation system similar to those used in isolation rooms to prevent cross infections. It was concluded that it is impossible to produce unidirectional flow according to the CDC recommendation of 4 ACH. Similarly, Philips et al. [43] demonstrated that it is not easy to ensure that an entire room space achieves the 12 ACH requirements even with a 15 ACH supply rate to the room, and the minimum ACH rate does not adequately ventilate the room. Additionally, the use of age-of-contaminant for comparing the efficiency of different ventilation solutions was recommended. Bryant also reiterated on the intricacy of the airflow and aerosol dispersion patterns within an isolation room and highlighted the importance of protecting the hospital staff that treat patients with infectious disease [44].
Movements by objects, such as persons and sliding doors, also disturb the air distribution and result in fluctuating indoor conditions. For instance, a 1-year field investigation of an ICU room in Taiwan established that patients’ visiting activities impacted the indoor air quality, particularly for coarse-sized particle concentrations. The results showed that the coarse-particle concentration increased as the number of patient visitors increased [45]. Furthermore, another study was conducted utilising a CFD simulation to investigate the effects of a moving person and the movement of a sliding door in an isolation room. In both cases, air distributions were easily affected by the moving objects. In particular, for the door movement, pollutant transfer was influenced by the specified pressure difference between rooms when the door was opened [46].
To summarise, different room configurations coupled with the airflow intricacies result in a multitude of ventilation solutions that address comfort and hygiene requirements. The selection of a particular solution can be determined using various indices that describe the efficiencies and effectiveness in terms of comfort and pollutant removal.
5.4. Indoor air quality
Good indoor air quality (IAQ) is essential for a healthy indoor environment. A poor air quality environment will cause a multitude of health problems, such as allergies, eye irritations and respiratory problems. Poor IAQ is caused by indoor pollutants. Indoor air of healthcare facilities, such as hospitals and clinics, may contain a variety of particulate pollutants, such as bio-aerosols and gaseous pollutants (waste anaesthetic gas). Therefore, hospital IAQ is evaluated based on particle counts, bacterial counts, fungal concentration, viral concentration and chemical parameters [47].
Indoor pollutants arise from a multiple of sources but are not limited to within the hospital environment. However, a major indoor source of bio-aerosol and gaseous pollutants is from respiratory activities of infectious patients and from activities within the ward room itself, such as bed-making and sterilisation. Other causes of poor IAQ from indoor pollutants are ill-planned building usage, defective designs, lack of maintenance and operation of the air-conditioning and mechanical ventilation systems [35], [36], [47], [48], [49].
Activities in the ward, such sterilisation and bed-making, also contribute to air quality deterioration. Beggs et al. [50] reviewed the aerial dissemination of pathogen-bearing particles in various hospital activities and surmised what causes environmental contamination. Chemical parameters, such as disinfectants, sterilising substances and anaesthetic gases, can also be found in hospitals. Subsequently, adverse health effects and discomfort due to these contaminations have been recorded.
Bio-aerosol pollutants require major attention in hospital environments and are closely linked to respiratory activities and infectious diseases. A number of studies have investigated these types of pollutants. This is elaborated further in Refs. [10], [51].
In addition, poor materials in buildings have been recorded as a source of pollutants. For example, a 700-bed hospital in Malaysia experienced substantial mould contamination that resulted in the suspension of hospital operations [30]. Results from the IAQ audit pointed to building defects and the improper operation of the air-conditioning system as the cause of the widespread of mould growth. Similarly, another case in Leeds, UK, recognised the exhaust ducting system as the source of a methicillin-resistant Staphylococcus aureus (MRSA) outbreak in an orthopaedic ward [12].
6. Engineering controls
6.1. Filtration
Filtration is one type of IAQ engineering control used in healthcare facilities. Filtration is an economical yet efficient method that improves indoor air quality. Furthermore, it is also an integral part of the air-conditioning and ventilation system. Additionally, air filtration presents a good solution that improves the IAQ but does not completely prevent infections.
Filtration requirements for facilities such as operating rooms [38], where requirements are similar to clean room applications, are well defined. Therefore, there is a trend to utilise clean room application standards in hospital environments.
Overall, guidelines and regulations stipulate air purity levels should be kept within limits. Airborne pollutants usually attach themselves to dust particles or water molecules [35]. The minimum ASHRAE standards [36] can be fulfilled using standard filters with gaskets and airtight frames. Most hospital bacteria can be isolated by 90–95% using efficient filters. Viruses are more demanding since their sizes are less than 1 micron. Additionally, high efficiency particulate air (HEPA) filters are widely recommended for healthcare facilities [2], [6], [24]. HEPA-type filters provide higher filtering efficiency and are recommended for specific applications; however, due to their expensive cost, their use should be kept at a minimum. The results have shown that the concentration of Aspergillus spores decreases by removing infectious droplets. Other findings have shown that immune-compromised patients have lower infections rates in isolation rooms with HEPA filters.
6.2. Ultraviolet irradiation
In many studies, ultraviolet irradiation, better known as ultraviolet germicidal irradiation (UVGI), has been recognised as a way to control microbial pollutants and is recommended in a few guidelines, such as Ref. [2]. Briefly, air flowing through the ducts is sterilised when UVGI is installed in the duct. Additionally, UVGI can be part of the room air circulation when installed independently.
Escombe et al. [52] studied the outcomes of upper room UV lights in a clinical setting in Peru. Based on guinea pig air sampling models, UV light could prevent 70% of the TB infections and more than half of the TB diseases. It was concluded that this type of control measure prevented most TB transmission. Therefore, UV lights are recommended for hospital spaces, such as sitting areas and emergency ward, where rooms are crowded regularly.
6.3. Natural ventilation
Natural ventilation is another method used to provide high airflow rates with low energy consumption. This method is particularly encouraged in the UK and is commonly practised in other tropical countries as a low-cost option, for example in Malaysia, Singapore and Peru.
Natural ventilation is derived from the natural forces which drive outdoor air through purpose built, building envelope openings such as windows, doors and ventilators and variable depending building design and outdoor climatic conditions relative to the indoor conditions. It also provides certain advantages in terms of capital and operational costs and capable of providing high ventilation rates. However, it is very dependent on outdoor climatic conditions and poses control challenges due to lack of sustainable negative pressure.
There are several natural ventilation designs suitable for tropical climate conditions when evaluated for thermal comfort and infection control, which are single sided corridor, courtyard and wind tower designs. Recent advances have also made natural ventilation an attractive option to be used in healthcare settings especially when used with mechanically assisted system or with advanced control systems for optimised system performances.
World Health Organization (WHO) has recommended that to prevent airborne infections, adequate ventilation shall be crucial for all patient care areas which include wards. The minimum ventilation rates based on the WHO recommendations are shown in Table 3 [53].
Table 3.
Natural ventilation requirement according to WHO guidelines.
| Room type | Minimum hourly averages natural ventilation rates | Remarks |
|---|---|---|
| General wards | 60 l/s per patient | Applies for any other patient care area such as corridors where emergency care is undertaken |
| Airborne precaution rooms | 160 l/s per patient | Only applicable for new facilities and major renovations |
| Corridors | 2.5 l/s per m3 | For spaces without fixed number of patients. |
Note: Overall, airflow shall drive the air from the agent sources to area where sufficient dilution is available and preferably outdoors.
In Lima, Peru, the effects of natural ventilation have been studied in terms of airborne infection transmission risks [54]. Using a Wells-Riley model, it was predicted that a mechanically ventilated room had a 39% infection rate compared with 33% in a modern ventilated room; the infection rate was predicted to be 11% for pre-1950s naturally ventilated facilities. These results showed that the risks are lower for a naturally ventilated facility compared to a mechanically ventilated room.
Qian et al. [55] investigated the natural ventilation in hospital wards in Hong Kong. Ventilation rates of 18 ACH and 24 ACH were shown to reduce the risk of cross infections of airborne diseases. Consequently, it was suggested to be suitable for hospital wards. This study also demonstrated that a ward with a natural ventilation system can be converted into a temporary isolation room by incorporating exhaust fans throughout the ward space. This type of system would correspond to a mechanically assisted system.
However, naturally ventilated facilities need to be designed and constructed properly for natural ventilation to achieve the required ventilation rates. Else, it would lead to potential thermal discomfort and transmission of infections among patients and HCWs.
7. Infections and airborne transmissions
Infection risk studies in a healthcare facility, particularly in a multiple-bed hospital ward, are of vital importance when considering a patient’s well-being. Healthcare facilities pose the greatest risk of infection because communicable and susceptible individuals congregate together, resulting in frequent airborne nosocomial transmission. Nosocomial infections result in prolonged hospitalisation and increased expenditure for the patients.
Many studies and reports have identified contaminated air and ventilation system deficiencies as the cause of nosocomial infections [3], [6], [19], [33]. Numerous studies have established the prevalent infection transmission modes in a tropical healthcare setting, highlighting the associated risks [9], [15]. Table 2 shows the main airborne diseases for humans.
Table 2.
Communicable pathogens and corresponding diseases.
| Airborne pathogen | Disease |
|---|---|
| Adenovirus | Colds |
| Arenavirus | Haemorhagic fever |
| Coronavirus | Colds |
| Echovirus | Colds |
| Morbilivirus | Measles |
| Influenza | Flu |
| Parainfluenza | Flu |
| Paramyxovirus | Mumps |
| Parvovirus B19 | Fifth disease, Anemia |
| Reovirus | Colds |
| Respiratory Syntical Virus | Pneumonia |
| Rhinovirus | Colds |
| Togavirus | Rubella |
| Varicella-zoster | Chickenpox |
| Chlamydia pneumonia | Pneumonia, Bronchitis |
| Mycobacterium tuberculosis | TB |
| Yersinia pestis | Pneumonic plague |
Tang et al. [51] reviewed and elaborated on the aerosol transmission of infectious agents, the associated diseases and the control methods. It was pointed out that droplets are generated during talking, sneezing and coughing. Subsequently, these droplets lead to a generation of infectious agents or pathogens. The agents are able to transmit infections over short distances and in close contact. Large droplets become smaller through evaporation, causing outbreaks over larger areas. However, the susceptibility of an individual to be infected depends on the pathogen quantum exposed and their bodies’ resistance.
Weber and Stilianakis [56] reviewed the inactivation of influenza A viruses in the environment and its modes of transmission. The inactivation of influenza A viruses depends on many factors, such as relative humidity, temperature and UV radiation. From this review, the airborne mode is a significant transmission route for nosocomial infections in indoor spaces.
8. Numerical method
The advent of computational fluid dynamic (CFD) technology has provided a significant tool for comprehensive airflow analysis of an entire room [32], [43], [57], [58], [59]. The analysis is achieved by numerically solving a set of partial differential equations representing the conservation of mass, momentum, energy, pollutant concentrations and turbulent quantities. The followings are the three groups of basic equations that govern the numerical solution for the thermal comfort and pollutant dispersal in a space: the continuity equation, Navier–Stokes equation and energy equation. These equations can be solved by specifying the initial and boundary conditions. CFD modelling results can be shown through user friendly graphical tools. The accuracy of CFD modelling results must be verified by comparison with field data.
Generally, the airflow in healthcare premises is turbulent. Most CFD solutions predict turbulence with modelled transport equations for the turbulent kinetic energy (k) and its dissipation rate (ɛ), which is known as the k–ɛ model. The standard k–ɛ model is easy to program, numerically robust and reasonably accurate. Apart from the k–ɛ model, other CFD models include the re-normalisation group (RNG) k–ɛ model, Reynolds averaged Navier–Stokes (RANS) equations, Reynolds stress viscous model and large eddy simulation. More information on CFD theories and their applications can be found in [58], [59].
Philips et al. [43] analysed different ventilation systems of isolation rooms using CFD models and suggested the provision of an anteroom for contagious patients. Similarly, Cheong and Phua [59] examined the airflow and pollution dispersal profiles for a “negative pressure” isolation room through experiments and CFD simulations. Three airflow schemes were investigated, and the results suggested that airflow schemes and furniture layout influence the airflow pollutant distribution. Beggs et al. [50] performed a CFD simulation using a standard k–ɛ model to explore the effect of airflow direction on the bio-aerosol concentration generated in a ward space. The results showed a significant variation between the ventilation strategies employed. It was concluded that a ceiling diffuser ventilation scheme is the most effective, improving the pollutant removal efficiency up to a 5 times. Qian et al. [8] integrated the Wells-Riley equation in a CFD model to predict the spatial infection risk distribution in a hospital ward, and the findings concurred closely with the infection distribution profile among the exposed students and patients.
The above studies represent only a small amount of research that utilised CFD tools. To evaluate the comfort levels and pollutant removals, CFD tools are very helpful in determining the sufficiency of the current design and future improvements. Furthermore, CFD tools will save much time, effort and cost prior to a facility’s construction.
9. Conclusions
Ventilation in a ward needs to be favourable to occupants (patients and healthcare workers). The ventilation should also assist in preventing diseases and treating patients. Many studies have elaborated on the health benefits of ventilating wards and its intricacies. In this review, challenges in a multiple-bed ward environment have been identified and elaborated on. However, specific problems in the tropics need to be the focus in future works as there is a lack of tropical studies.
Indoor conditions in wards are very different compared with other environments, such as an office space. These conditions affect the well-being of patients and the transmission of infections. Engineering controls employed in healthcare settings differ in terms of parameters and needs. As identified during the review, there is an apparent knowledge gap for ventilation studies in the tropics compared with temperate climates, as fact studies and guidelines have only been published in countries of temperate climates.
A mechanical ventilation system significantly helps to improve the indoor environment. Also, natural ventilation is being explored to improve the indoor environment quality. Mixing ventilation and displacement ventilation are the most prevalent principles used to design ventilation systems, which when combined with other engineering controls, such as filtration and UVGI, can significantly improve the indoor environment. These systems need further optimisation for tropical conditions.
CFD modelling is a valued tool for analysing airflow and evaluating ventilation systems. Recent reviews have focused on specialised clinical areas, such as operating rooms and isolation rooms. Different conditions have been simulated and verified with field measurements. However, specific studies are needed for multiple-bed wards to bridge the knowledge gap regarding the thermal comfort, pollutant removals and transmission risk of airborne diseases. These studies along with novel engineering controls will assist in identifying the ventilation requirements for the tropics.
References
- 1.ASHRAE . American Society of Heating Refrigerating and Air-Conditioning Engineers; Atlanta, USA: 2007. ASHRAE applications handbook. [Google Scholar]
- 2.CDC . U.S. Department of Health and Human Services Centers for Disease Control and Prevention (CDC); USA: 2005. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings. [Google Scholar]
- 3.Australian Government Department of Health and Ageing . Australian Government Department of Health and Ageing; Australia: 2004. Infection control guidelines for the prevention of transmission of infectious diseases in the health care setting. [Google Scholar]
- 4.The Chartered Institution of Building Services Engineers . The Chartered Institution of Building Services Engineers; London: 2004. CIBSE guide B. [Google Scholar]
- 5.AIA . American Institute of Architects; Washington, DC: 2006. Guidelines for design and construction of hospital and health care facilities. [Google Scholar]
- 6.Ulrich R., Zimring C., Quan X., Joseph A., Choudhary R. The Center for Health Design for the Designing the 21st Century Hospital Project; 2004. The role of the physical environment in the hospital of the 21st century: a once-in-a-lifetime opportunity. [Google Scholar]
- 7.Reynolds M.G., Huy Anh B., Thu V.H., Montgomery J.M., Bausch D.G., Shah J.J. BMC Public Health; 2006. Factors associated with nosocomial SARS-CoV transmission among healthcare workers in Hanoi, Vietnam, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qian H., Li Y., Nielsen P.V., Huang X. Spatial distribution of infection risk of SARS transmission in a hospital ward. J Build Environ. 2009;44:1651–1658. [Google Scholar]
- 9.Feldman C., Sarosi G.A. Springer; 2004. Tropical and parasitic infections in the intensive care unit. [Google Scholar]
- 10.Kowalski W.J., Banfleth W. HPAC; July 1998. Airborne respiratory diseases and mechanical systems for control of microbes. 34–48. [Google Scholar]
- 11.Wan Hanifah W.H., Lee J.K.F., Quah B.S. Comparison of the pattern of nosocomial infections between the neonatal intensive care units of Hospital Kuala Terengganu and Universiti Sains Malaysia, Kelantan. Malays J Med Sci. 2000;7:33–40. [PMC free article] [PubMed] [Google Scholar]
- 12.Kumari D.N.P., Haji T.C., Keer V., Hawkey P.M., Duncanson V., Flower E. Ventilation grilles as a potential source of methicillin-resistant Stuhylococcus aureus. J Hosp Infect. 1998;39:127–133. doi: 10.1016/s0195-6701(98)90326-7. [DOI] [PubMed] [Google Scholar]
- 13.Sundell J., Helvin H., Novosel D. National Center for Energy Management and Building Technologies; Alexandria: 2006. Ventilation rates and health: report of an interdisciplinary review of the scientific literature. [Google Scholar]
- 14.Li Y., Leung G.M., Tang J.W., Yang X., Chao C.Y.H., Lin J.Z. Role of ventilation in airborne transmission of infectious agents in the built environment – a multidisciplinary systematic review. Indoor Air. 2007;17:2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 15.Siegel J.D., Rhinehart E., Jackson M., Chiarello L. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35:65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guy A. Sir Isaac Pitmann & Sons, Ltd.; Bath: 1954. Hospital planning requirements. [Google Scholar]
- 17.Gainsorough H., Gainsborough J. The Architectural Press; London: 1964. Principles of hospital design. [Google Scholar]
- 18.Cox A. Butterworth-Heinemann Ltd.; 1990. Hospitals and health care facilities: a design and development guide. [Google Scholar]
- 19.Tai L.L., Ng S.H. Quality of Health Care Section, Medical Development Division. s.l.: National Audit on Adult Intensive Care Unit, Ministry of Health Malaysia; 2005. A national survey of intensive care resources in Malaysia. [Google Scholar]
- 20.Rubin H.R., Owens A.J., Golden G. The Center for Health Design, Inc.; 1998. Status report (1998): an investigation to determine whether the built environment affects patients’ medical outcomes. Quality of Care Research, The Johns Hopkins University. [PubMed] [Google Scholar]
- 21.Joseph A., Rashid M. The architecture of safety: hospital design. Curr Opin Crit Care. 2007;13:714–719. doi: 10.1097/MCC.0b013e3282f1be6e. [DOI] [PubMed] [Google Scholar]
- 22.Marberry Sara O. Van Nostrand Reinhold; 1995. Innovations in healthcare design. [Google Scholar]
- 23.Keith H. UK ward design: patient dependency, nursing workload, staffing and quality—an observational study. Int J Nurs Stud. 2008;45:370–381. doi: 10.1016/j.ijnurstu.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Pidwirny M. Fundamentals of physical geography. 2nd ed. 2006. Climate classification and climatic regions of the world.http://www.physicalgeography.net/fundamentals/7v.html Online [accessed 27.10.10] [Google Scholar]
- 25.National Health Service . National Health Services Estates; 1994. Design considerations: ventilation in health care premises. Health Technical Memorandum 2025. [Google Scholar]
- 26.Hwang R.L., Lin T.P., Cheng M.J., Chien J.H. Patient thermal comfort requirement for hospital environments in Taiwan. Build Environ. 2007;42:2980–2987. [Google Scholar]
- 27.Nicol F. Adaptive thermal comfort standards in the hot-humid tropics. Energy Build. 2004;36:628–637. [Google Scholar]
- 28.Mallick F.H. Thermal comfort and building design in the tropical climates. Energy Build. 1996;23:161–167. [Google Scholar]
- 29.Yu WJ, Cheong KWD, Kosonen R, Xie YH, Leow HC. A thermal comfort study on displacement ventilation in the tropics. In: International society of indoor air quality and climate, healthy buildings proceeding; 2003.
- 30.ASHRAE . American Society of Heating Refrigerating and Air-Conditioning Engineers; Atlanta, USA: 2003. HVAC design manual for hospitals and clinics. [Google Scholar]
- 31.Lian KS, Inangda PSN, Ramly A. Sources of indoor air quality problem in a new hospital in Malaysia; 2007.
- 32.Schild P.G. Air Infiltration and Ventilation Centre; 2004. AIVC ventilation information paper. [Online] International Network for Information on Ventilation and Energy Performance. [Google Scholar]
- 33.Qian H., Li Y., Nielsen P.V., Hyldgaard C.E., Wong T.W., Chwang A.T.Y. Dispersion of exhaled droplet nuclei in a two-bed hospital ward with three different ventilation system. Indoor Air. 2006;16:111–128. doi: 10.1111/j.1600-0668.2005.00407.x. [DOI] [PubMed] [Google Scholar]
- 34.Memarzadeh F., Manning A. ASHRAE; 2000. Thermal comfort, uniformity, and ventilation effectiveness in patient rooms: performance assessment using ventilation indices. [Google Scholar]
- 35.Dascalaki E.G., Lagoudi A., Balaras C.A., Gaglia A.G. Air quality in hospital operating rooms. Build Environ. 2008;43:1945–1952. [Google Scholar]
- 36.Balaras C.A., Dascalaki E., Gaglia A. HVAC and indoor thermal conditions in hospital operating rooms. Energy Build. 2007;39:454–470. [Google Scholar]
- 37.Chow T.T., Yang X.Y. Ventilation performance in operating theatres against airborne infection: review of research activities and practical guidance. J Hosp Infect. 2004;56:85–92. doi: 10.1016/j.jhin.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 38.Dharan S., Pittet D. Environmental controls in operating theatres. J Hosp Infect. 2002;51:79–84. doi: 10.1053/jhin.2002.1217. [DOI] [PubMed] [Google Scholar]
- 39.Ho S.H., Rosario L., Rahman M.M. Three-dimensional analysis for hospital operating room thermal comfort and contaminant removal. Appl Therm Eng. 2009;29:2080–2092. [Google Scholar]
- 40.Rui Z., Guangbei T., Jihong L. Study on biological contaminant control strategies under different ventilation models in hospital operating toom. Build Environ. 2008;43:793–803. [Google Scholar]
- 41.Liu J., Wong H., Wen W. Numerical simulation on a horizontal airflow for airborne particles control in hospital operating room. Build Environ. 2009;44:2284–2289. [Google Scholar]
- 42.Qian H., Lia Y., Nielsen P.V., Hyldgaard C.E. Dispersion of exhalation pollutants in a two-bed hospital ward with a downward ventilation system. Build Environ. 2008;43:344–354. [Google Scholar]
- 43.Phillips D.A., Sinclair R.J., Schuyler G.D. American Society of Heating, Refrigerating and Air-Conditioning Engineers Inc.; 2004. Isolation room ventilation design case studies. IAQ 2004 Conference Proceedings. [Google Scholar]
- 44.Jennifer R.B. Transport of exhaled particulate matter in airborne infection isolation rooms. Build Environ. 2009;44:44–55. doi: 10.1016/j.buildenv.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang C.S., Chung F.F., Lin M.C., Wan G.H. Impact of patient visiting activities on indoor climate in a medical intensive care unit: a 1-year longitudinal study. Am J Infect Control. 2009;37:183–188. doi: 10.1016/j.ajic.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 46.Shih Y.C., Chiu C.C., Wang O. Dynamic airflow simulation within an isolation room. Build Environ. 2007;42:3194–3209. doi: 10.1016/j.buildenv.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheong K.W., Chong K.Y. Development and application of indoor air quality audit to an air-conditioned building in Singapore. Build Environ. 2001;36:181–188. [Google Scholar]
- 48.Badgwell M. An evaluation of air safety source-control technology for the post anesthesia care unit. J PeriAnesthesia Nurs. 1996;11:207–222. doi: 10.1016/s1089-9472(96)80020-7. [DOI] [PubMed] [Google Scholar]
- 49.Srinivasan A., Beck C., Buckley T., Geyh A., Bova G., Merz W. The ability of hospital ventilation system to filter aspergillus and other fungi following a building implosion. Infect Control Hosp Epidemiol. 2002;23:520–524. doi: 10.1086/502100. [DOI] [PubMed] [Google Scholar]
- 50.Beggs C.B., Kerr K.G., Noakes C.J., Hathway E.A., Sleigh P.A. The ventilation of multiple-bed hospital wards: review and analysis. Am J Infect Control. 2008;36:250–259. doi: 10.1016/j.ajic.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 51.Tang J.W., Li Y., Eames I., Chan P.K.S., Ridgway G.L. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J Hosp Infect. 2006;64:100–114. doi: 10.1016/j.jhin.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Escombe A.R., Moore D.A.J., Gilman R.H., Navincopa M., Ticona E. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Med. 2009;6(3) doi: 10.1371/journal.pmed.1000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Atkinson J., Chartier Y., Pessoa-Silva C., Jensen P., Li Y., Seto W.-H., editors. Natural ventilation for infection control in health-care settings – WHO guidelines. World Health Organization; 2009. [PubMed] [Google Scholar]
- 54.Escombe A.R., Oeser C.C., Gilman R.H., Navincopa M., Ticona E. Natural ventilation for the prevention of airborne contagion. PLoS Med. 2007;4:2. doi: 10.1371/journal.pmed.0040068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qian H., Li Y., Seto W.H., Ching P., Ching W.H., Sun H.Q. Natural ventilation for reducing airborne infection in hospitals. Build Environ. 2010;45:559–565. doi: 10.1016/j.buildenv.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weber T.P., Stilianakis N.I. Inactivation of influenza A viruses in the environment and modes of transmission: a critical review. J Infect. 2008;57:361–373. doi: 10.1016/j.jinf.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.American Society of Heating . Refrigerating and Air Conditioning Engineers Inc.; 2002. HVAC computational fluid dynamics. [chapter 33] [Google Scholar]
- 58.Qingyan C. Ventilation performance prediction for buildings: a method overview and recent applications. Build Environ. 2009;44:848–858. [Google Scholar]
- 59.Cheong K.W.D., Phua S.Y. Development of ventilation design strategy for effective removal of pollutant in the isolation room of a hospital. Build Environ. 2006;41:1161–1170. [Google Scholar]


