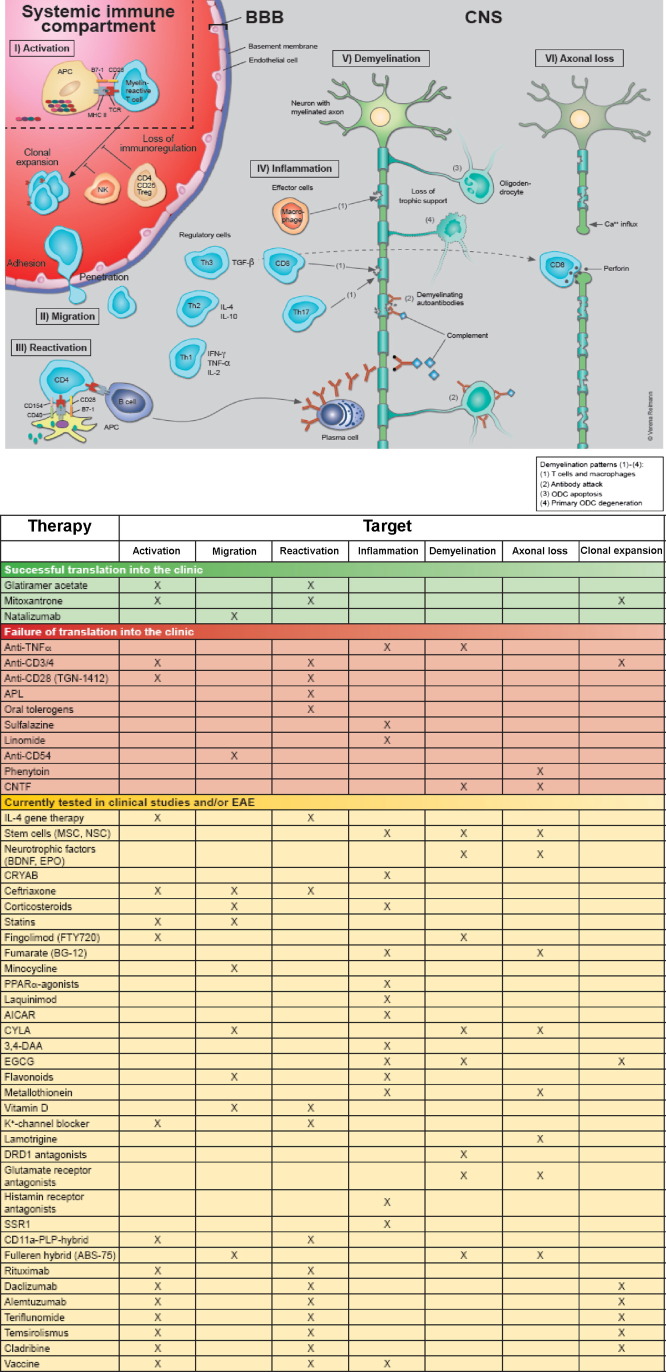
Fig. 4.
Putative pathogenic mechanisms of MS. Auto-reactive lymphocytes may be recruited from peripheral lymphoid organs and after migration through the BBB reactivated in the CNS, where an inflammatory cascade is initiated leading to subsequent damage of myelin and axons. Alternatively, primary oligodendroglial and axonal degeneration may be followed by an inflammatory autoimmune process. The adjacent table depicts the putative pathogenic processes that are targeted by established and experimental therapies. Treatments are grouped according to the contribution made by EAE to their development, i.e. they are either successfully translated into the clinic (green), only successful in EAE (red) or currently tested in EAE and/or MS (yellow). Abbreviations: AICAR, 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside; APC, antigen-presenting cell; APL, altered peptide ligand; BBB, blood–brain barrier; BDNF, brain-derived neurotrophic factor; CD, cluster of differentiation; CNS, central nervous system; CNTF, ciliary neurotrophic factor; CRYAB, αB-crystallin; CYLA, Calpain inhibitor; 3,4-DAA, N-(3,4,-dimethoxycinnamoyl) anthranilic acid; DRD1, dopamine receptor type 1; EGCG, (−)-epigallocatechin-3-gallate; IL, interleukin; IFN-γ, interferon-γ; major histocompatibility complex; MOG, myelin oligodendrocyte glycoprotein; MP, methylprednisolone; MRI, magnetic resonance imaging; NK, natural killer; ODC; oligodendrocyte; PLP, proteolipid protein; PPAR-α, peroxisome proliferator-activated receptor-α; SSRI, selective serotonin reuptake inhibitor; Tc, cytotoxic T cell; TCR, T cell receptor; TGF-β, transforming growth factor-β; Th cell, helper T cell; TNF-α, tumor necrosis factor-α.