Abstract
The appearance in south China and subsequent global epidemic of Sars in 2003, and its re-emergence this year, is focusing attention on the growing threat of animal diseases making the jump from their normal hosts to human populations. Nigel Williams reports.
Many new human diseases of animal origin are expected to appear over the coming decades as a result of environmental disruption, global warming and behavioral change, scientists at a meeting at the Royal Society in London warned last month as a growing number of scientists and other bodies contemplate future threats from infections presently occurring in animals that may spread to humans.
The reappearance of Severe acute respiratory syndrome (Sars) in China, the potentially lethal pneumonia-like disease that killed 800 people in 27 countries last year, is a signal to the world of the threat from emerging infections that appear to have jumped from animals, researchers said.
The first case of Sars since last year's outbreak was confirmed last month in a television journalist from Guangzhou, the southern Chinese city in the province of Guangdong. Further cases have since been confirmed by the Chinese authorities.
Professor Tony McMichael, director of the National Centre for Epidemiology and Population Health at the Australian National University, Canberra, said: “Sars, Aids, Ebola and Marburg's disease have all emerged in the past 30-40 years. There have been 30 new diseases since 1975 and we can expect a similar number in the future.”
Most new infections have occurred as a result of increased human contact with animals. Aids is believed to have arisen when humans moved into the forests of Africa on logging expeditions and killed chimpanzees for their meat, McMichael said.
Malik Peiris, professor of microbiology at Hong Kong University and one of the first scientists to identify the Sars virus, said there was an urgent need to monitor viruses that jumped from animals to humans. Many did not cause disease in their original animal hosts so were not picked up by conventional veterinary checks, he said.
“We were fortunate. Sars was a global health problem solved with a global effort. It will not be the last and a global effort to solve future health problems will be very important,” he said.
Professor Nan Shan Zhong of the Guangzhou Respiratory Disease Research Institute said there were clues that suggested a link between Sars and the civet cat, bred for food in China. A similar coronavirus to that linked with the Sars outbreak (Sars-CoV) was highly concentrated in the cats’ faeces and the first cases last year occurred in animal traders. Thousands of the cats were killed last month after the Chinese government ordered a cull following the latest cases of Sars and banned their sale in markets.
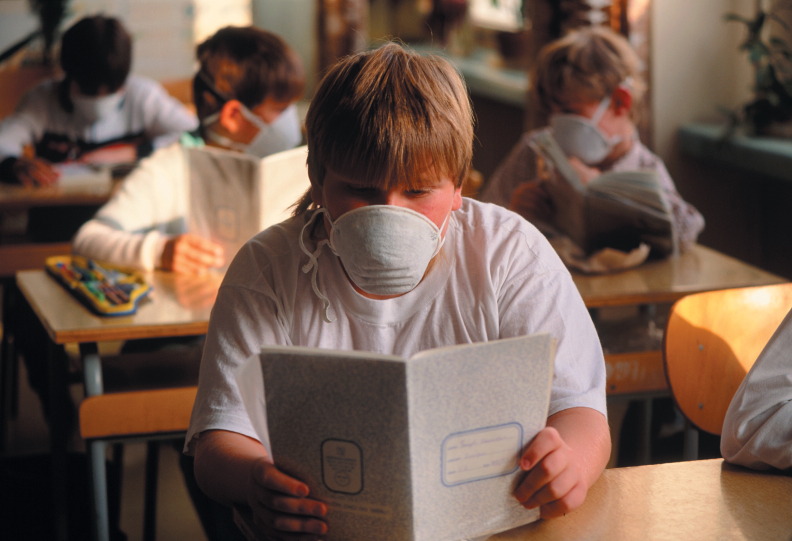
All countries have been asked by the WHO to maintain their ability to detect and respond to the re-emergence of the disease. But clinicians and researchers are hampered by a number of factors. These include the fact that there are no specific clinical features of Sars, the lack of a rapid diagnostic test that can reliably detect the Sars-CoV in the first few days after the onset of clinical symptoms, and the seasonal occurrence of other respiratory diseases, including influenza. ‘The major problem in the coming year will be the management of false alarms triggered by suspect clinical cases,’ says Roy Anderson, professor of infectious disease epidemiology at Imperial College London.
“Detection of the presence of the virus soon after onset of clinical symptoms remains difficult, with the most sophisticated tests still only providing a sensitivity of 60–70 per cent in samples taken at various times after the onset of fever,” he says. Sensitivity can be improved if samples from the lower respiratory tract can be obtained in the second week after the clinical symptoms have appeared, “but the procedures to obtain material for analysis are invasive and not without risk to the patient,” he says. Tests based on the detection of immune system markers in blood have appeared to be highly sensitive but only after at least 21 days since the onset of illness.
“It is difficult to escape the conclusion that the world community was very lucky this time round, given the low transmissibility of the agent and its biology where clinical symptoms appear well before peak infectiousness, plus the fact that fairly draconian public health measures could be put in place with great efficiency in Asian regions where the epidemic originated,” Anderson says.
Many other bodies and researchers worldwide are increasingly focusing on animal-to-human diseases in the light of last year's Sars outbreak. These species-hopping diseases include influenza, all the more dangerous because the virus can be passed from farm animals to human beings. The bird influenza ravaging several Asian countries — and which has been blamed for the deaths of at least three Vietnamese people — could precipitate a more serious global health crisis than Sars if it goes on to spread by human contact, the WHO has warned.
The alarm came as Vietnam reported several more suspected cases and suggested that pigs could be involved in the transmission of the virus from birds to humans. Millions of chickens and ducks have died or are being killed in Vietnam, Japan and South Korea, in efforts to contain the outbreak.
Another recent influenza epidemic led to the loss of tens of millions of poultry in Italy, the Netherlands, Germany, Belgium and other European countries, either from the sickness directly or as a result of preventative slaughter measures. Researchers believes some cases of human conjunctivitis and serious influenza resulted from this avian outbreak.
And in recent years, researchers have also recorded growing genetic and immunological variability in swine influenza in the face of widespread vaccine use.
Influenza remains a constant threat to humans because of the potential of the human strain to acquire major new antigens from avian strains. The terrible Spanish flu pandemic which resulted in the death of 20-40 million people after the First World War was attributed to a major antigenic change.
Evidence is growing that HIV passed from monkeys to people through the consumption of bushmeat. And other recent viruses are thought to be of animal origin. The Marburg virus, closely related to Ebola — which has caused lethal haemorrhagic fever in tropical Africa — was discovered more than 30 years ago when green monkeys captured in Uganda were brought to a laboratory in the German city of the same name. Seven people died from violent haemorrhagic fever.
A research consortium of German, Finnish, Lithuanian and Swedish laboratories has recently described the various forms of hantaviruses, which cause respiratory diseases, that infect small rodents in eastern Europe. Hantaviruses can pass to humans, particularly forest workers and farmers whose work brings them into contact with these animals. A particularly virulent form has been found in the Balkan states in Europe which has proved lethal in 12 per cent of human cases. The new analysis of the Hantavirus strains should help the development of analytical and diagnostic tests.
Global warming is allowing certain species, in particular insects, to colonise new regions where they can further propagate pathogens. Tropical deforestation is bringing humans into contact with animals they have not encountered before. The Hendra and Nipah viruses, discovered in the 1990s, and deadly in some 50 per cent of cases, appear to originate in fruit-eating bats from south-east Asian forests.
The increasing contact between humans and animal species is not matched by knowledge of the biochemical mechanisms that create a species barrier to infection. “Pathogen–host interactions are right now the subject of intense research. A better understanding of the pathogenesis mechanisms, facilitated by growing knowledge of genomes, should help us see more clearly,” says Alistair MacMillan of the UK's Central Veterinary Laboratory.
The USA-EU Biotechnology Research Task Force concluded at its meeting last summer that there was an urgent need to organize a meeting on this topic. This workshop will focus more particularly on experimental hypotheses and models that can potentially verify the molecular and environmental mechanism governing the transmission of infectious agents from one species to another, says Etienne Magnien, director for biotechnologies, food and agriculture at the European Commission's research directorate.
There is no doubt Sars has focused thinking on the challenges presented by the emergence of new human diseases arising from animals. Any many are pleased that WHO is strengthening its abilities. “The quick and effective response of WHO to the Sars crisis did much to restore faith amongst the many critics of the effectiveness of international agencies with large bureaucracies and limited resources for action,” says Anderson. “This strengthened approach to outbreak response will be reflected in the revised international health regulations, which set out roles and responsibilities for preventing transboundary spread of infectious diseases both on a routine basis and in crisis situations,” says David Heymann of the WHO.