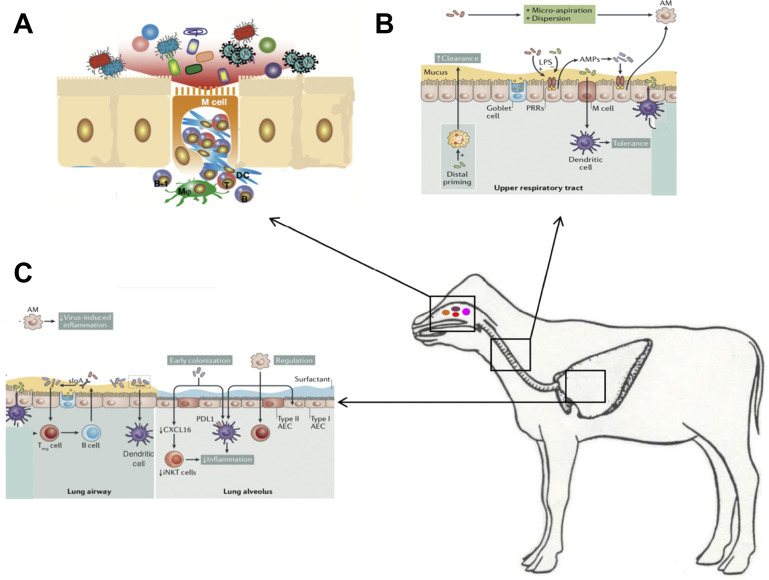
Fig. 10.
Respiratory mucosal immune system. (A) The nasal associated lymphoid tissue including the tonsils is an important site for immune responses and microbiome interactions and respiratory pathogen carriage. Microfold cells (M cells) specialize in antigen uptake and are present throughout the respiratory and GI mucosal immune system. The cilia of M cells are shorter than those of conventional epithelium cells. These cells are like a window to the immune system and allow interaction with viruses, bacteria, and other components of the microbiome. On its basal side, the M cell develops a pocket-like structure that can hold immunocompetent cells. M cells, such as macrophages (MΦ), function in active antigen uptake. Because lysosome development in M cells is poor, in most cases the incorporated antigens are just passed through the M cells unmodified and then taken up by DCs, which then interact with T cells, which in turn interact with B cells. (B) URT and (C) lower respiratory tract (LRT). The URT mucous is thicker than the LRT and the ME are taller and decrease in size as one descends into the LRT and the alveoli. Resident microorganisms prime immune cells include ME, neutrophils, and dendritic cells, which all contribute to the clearance of pathogens. Moreover, microbial signaling is necessary for the recruitment and activation of regulatory cells, such as anti-inflammatory alveolar macrophages and Treg cells. The host responds to microbial colonization through the release of AMPs and sIgA. Sensing of the microbiota involves microfold (M) cells that activate tolerogenic dendritic cells. In addition, alveolar dendritic cells can directly sample luminal microorganisms. These pathways lead to the regulation of inflammation and the induction of tolerance in the respiratory tract. It is also likely that early bacterial colonization is key to long-term immune regulation, which is illustrated by the microbiota-induced decrease in CXC-16 (Cxcl16) gene, which prevents the accumulation of inducible natural killer T cells, and by the programmed death ligand 1–mediated induction of tolerogenic dendritic cells. This tolerant milieu, in turn, contributes to the normal development and maintenance of resident bacterial communities, which are also influenced by host and environmental factors. AEC, alveolar epithelial cell; AM, alveolar macrophages; iNKT, inducible natural killer T cells; PDL1, programmed death ligand 1; PRR, pattern recognition receptor; URT, upper respiratory tract.
(Adapted from Sato S, Kiyono H. The mucosal immune system of the respiratory tract. Curr Opin Virol. 2012;2(3):225-232 and Man WH, de Steenhuijsen Piters WAA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol. 2017;15(5):259-270; with permission.)