Abstract
Presentation and lesion localisation Seven adult domestic shorthair cats were presented with a 1- to 6-day history of progressive neurological signs. A focal skin puncture and subcutaneous swelling over the dorsal part of the head were detected on physical examination. Neurological examination indicated lesion(s) in the right forebrain in four cats, multifocal forebrain in one cat, left forebrain in one cat, and multifocal forebrain and brainstem in the remaining cat. In all cats, magnetic resonance imaging revealed a space-occupying forebrain lesion causing a severe mass effect on adjacent brain parenchyma.
Clinical approach and outcome All cats were managed with a combination of medical and surgical treatment. At surgery a small penetrating calvarial fracture was detected in all cats, and a tooth fragment was found within the content of the abscess in two cats. The combination of surgical intervention, intensive care and intravenous antimicrobials led to a return to normal neurological function in five cats.
Practical relevance As this series of cases indicates, successful resolution of a brain abscess due to a bite injury depends on early recognition and combined used of antimicrobials and surgical intervention. A particular aim of surgery is to remove any skull and foreign body (tooth) fragments that may represent a continuing focus of infection.
Bacterial infection of the central nervous system (CNS) may result in an abscess — that is, a localised collection of purulent material within the CNS, its surrounding membranes, or in the epidural space. 1 Brain abscesses are uncommon in dogs and cats, and may arise as a result of various aetiological processes: spread from distant foci of infection (eg, bacterial endocarditis, lung abscesses); penetrating injury to the calvarium (eg, bite wound, bullet); direct extension of infection from nasal sinuses, ears and eyes, or from diseased maxillary tooth roots; use of contaminated surgical instruments; or penetration of the calvarium and brain substances by a foreign body (eg, plant material, sewing needle). 2–7 Additionally, brain abscesses can be the result of a compromised immune system. 8
Bacterial CNS abscesses can be polymicrobial and are more commonly associated with aerobic bacteria (eg, Streptococcus, Staphylococcus, Pasteurella and Nocardia species) than anaerobic bacteria (Bacteroides, Fusobacterium, Peptostreptococcus, Actinomyces and Eubacterium species). 3,9–11
This report describes seven cats with a brain abscess secondary to a bite injury diagnosed by magnetic resonance imaging (MRI) and managed with a combination of medical and surgical treatment.
Clinical histories
Seven adult cats aged between 3 and 13 years were presented for evaluation of progressive neurological signs ranging in duration from 1–6 days prior to presentation.
Cat 1
Case 1, a 3-year-old male entire domestic shorthair (DSH) cat, presented with a 1-day history of circling, head pressing, disorientation and a single focal seizure. Two days prior to the onset of neurological signs, the cat was reported to be inappetent and a subcutaneous abscess was identified over the dorsal part of the head. At that time clindamycin (Antirobe; Pfizer) 15 mg/kg PO and ketoprofen (Ketofen; Fort Dodge) 2 mg/kg SC were given. Due to deterioration in the clinical signs on the day of the referral the cat was given a single dose of amoxicillin clavulanate (Augmentin; GlaxoSmithKline) 17 mg/kg IV, metronidazole (Metronidazole; Baxter Healthcare) 10 mg/kg IV, meloxicam (Metacam; Pfizer) 0.3 mg/kg SC, dexamethasone (Dexadreson; Intervet) 1 mg/kg IV and intravenous isotonic sodium chloride infusion at maintenance rate.
On physical examination a focal skin puncture and a subcutaneous abscess on the right frontal part of the head were found. Neurological evaluation revealed an obtunded mental status, propulsive circling to the right, postural reaction deficits in all four limbs but more severe on the left side, left-sided Horner's syndrome, and an absent menace response and absent visual placing response with normal pupillary light reflex (PLR) in both eyes. These neurological findings suggested a predominantly right-sided forebrain lesion.
Cat 2
Case 2, a 7.5-year-old male neutered DSH cat, presented with a 6-day history of lethargy and anorexia; the cat's condition had deteriorated in the past 24 h with the onset of bilateral third eyelid protrusion and disorientation. Prior to referral, the cat was treated with a single dose of enrofloxacin (Baytril; Bayer HealthCare) 5 mg/kg SC, buprenorphine (Vetergesic; Alstoe) 0.02 mg/kg IM and intravenous Hartmann's fluid (Baxter Healthcare) at twice maintenance rate. The owner reported that 2 weeks earlier the cat had a fight which resulted in a wound on top of his head.
Physical examination revealed third eyelid protrusion, most pronounced in the right eye, and a healed wound on the right dorsal part of the head. Neurological examination revealed an obtunded mental status, circling to the right, an absent menace response and decreased visual placing response on the left side, left-sided Horner's syndrome and pain reaction on palpation of the skull. These neurological findings suggested a right forebrain lesion.
Cat 3
Case 3, a 5.5-year-old female neutered domestic longhair (DLH) cat, presented with a 1-day history of lethargy and cluster seizures. The cat was given a single dose of carprofen (Norocarp; Norbrook) 2 mg/kg SC and cefovecin sodium (Convenia; Pfizer) 8 mg/kg SC, prior to referral.
Physical examination revealed a subcutaneous abscess over the dorsal part of the head. Neurological evaluation revealed an obtunded mental status, postural reaction deficits in the right thoracic and pelvic limbs, and an absent menace response with normal PLR in both eyes, suggesting a predominantly left-sided forebrain lesion.
Bacterial CNS abscesses can be polymicrobial and are more commonly associated with aerobic bacteria than anaerobic bacteria.
Cat 4
Case 4, a 4-year-old male neutered DSH cat, presented with a 1-day history of seizure, head pressing, reluctance to move and pyrexia (39.4°C). The cat had been started on amoxicillin clavulanate (Synulox; Pfizer) 12.5 mg/kg PO q12h for 2 days prior to referral.
On admission, physical examination revealed a wound over the right dorsal part of the head. Neurological examination revealed an obtunded mental status, lateral recumbent posture, tetraparesis, delayed postural reactions in all four limbs, an absent menace response in both eyes, and severe anisocoria with a dilated and unresponsive right pupil. The neurological findings suggested a predominantly right-sided forebrain lesion with possible right-sided tentorial herniation secondary to elevated intracranial pressure (ICP).
Cat 5
Case 5, a 12.5-year-old neutered female DSH cat, presented for a small puncture wound on the right frontal part of the head assumed to be subsequent to a cat fight. At the time the cat was pyrexic (39.7°C) and was treated with cefovecin sodium (Convenia; Pfizer) 8 mg/kg SC and meloxicam (Metacam; Pfizer) 0.3 mg/kg SC single dose. Six days later the cat re-presented as an emergency following a rapid onset of neurological signs.
Physical examination was unremarkable; the wound was already healed and body temperature was back to normal. Neurological examination revealed an obtunded mental status, compulsive circling to the left, bilaterally absent menace response, slight anisocoria with dilated left pupil, and poor consensual PLR, photophobia and central blindness in the right eye. The lesion localisation was left forebrain.
Cat 6
Case 6, a 10-year-old male DSH cat, presented with a 7-day history of depressed mental status, circling to the right and pacing aimlessly. The cat was initially treated by the owner with cephalexin (Ceporex; Teofarma) 15 mg/kg PO q12h for 2 days, and after that was presented to the referring veterinarian for an abscess over the dorsal part of the head. The abscess was flushed and clindamycin (Antirobe; Pfizer) 20 mg/kg PO q24h and meloxicam (Metacam; Pfizer) 0.15 mg/kg SC q12h were started, but 12 h later the cat had deteriorated with bilateral myosis, bilateral absent menace response and circling to the right. Enrofloxacin (Baytril; Bayer HealthCare) 5 mg/kg SC and prednisolone (Prednicare; Animalcare) 2 mg/kg PO q24h were started for 7 days, but clinical signs progressed with bilateral third eyelid protrusion, mydriasis, an absent PLR and rectal temperature of 39°C.
At the time of presentation the cat was pyrexic (41.1°C). Neurological examination revealed a severely obtunded mental status, upper motor neuron ambulatory tetraparesis, intermittent head pressing, right-sided circling, abnormal postural reactions in all four limbs but worse on the left side, bilaterally absent menace response with intact PLR and decreased physiological nystagmus in both eyes. The lesion localisation was multifocal forebrain and brainstem.
Cat 7
Case 7, a 13-year-old male DSH cat, presented with a 2-day history of lethargy and swelling over the dorsal part of the head. Two months earlier the cat had undergone a left rostral tentorial craniectomy for meningioma resection, from which he recovered uneventfully. The cat was not on any medication at the time of referral.
Physical examination was unremarkable except for the presence of a wound and an abscess on the right dorsal part of the head. Neurological examination revealed an obtunded mental status, intermittent circling to the right, mild hemiparesis and delayed postural reactions on the left side, and an absent menace response in the left eye. These signs were consistent with a right forebrain lesion.
Differential diagnoses considered.
All cats had regular contact with other cats. Differentials considered based on the results of neurological examination included an inflammatory/infectious CNS disease, primary or metastatic brain tumour and, less likely, a cerebral bleed. In view of the presence of a focal skin puncture or subcutaneous swelling over the calvarium in all cats, an infectious process was considered the main differential.
MRI examination and findings
All cats underwent MRI of the brain. Images were acquired on MRI units at different centres (1.5 T Gyroscan NT Intera, Philips Medical Systems, Surrey, UK [cats 1 and 2]; Vet Esaote 0.2 Tesla permanent magnet, Esaote, Genoa, Italy 1.0 [cats 3, 4 and 5]; 0.4 T Aperto MRI, Hitachi, Tokyo, Japan [cat 6]; T Signa Horizon LS 1.0 GE Medical Systems Milwaukee, WI [cat 7]).
Asaminimum, T2-weighted images (WI) in two planes (transverse and sagittal) were obtained. Transverse T1WI, and transverse T1WI after intravenous IV paramagnetic contrast medium (gadolinium) administration, were also obtained in all cases, with the exception of one cat (cat 4) because of financial restrictions. Transverse fluid attenuation inversion recovery (FLAIR) images were performed in two cases (cats 1 and 2). Additional sequences were obtained as requested by the attending neurologist and radiologist. All images were interpreted by a board-certified veterinary radiologist and/or board-certified veterinary neurologist.
Cat 7 underwent repeat MRI of the brain 2 weeks after surgery and 2 years later for meningioma regrowth. Cat 6 had another MRI study performed 7 weeks after surgery.
In all cats, MRI study revealed a predominantly intra-axial space-occupying lesion in the frontal or parietal region, diffusely hypointense on T1WI, with a hyperintense core and hypointense margins on T2WI, and strong ring enhancement. There were severe secondary effects on adjacent brain parenchyma such as perilesional white matter oedema with subfalcine (cats 1 and 2), subtentorial (cats 1, 2, 6 and 7) and foramen magnum brain herniation (cat 7) (Figs 1 and 2). In all cats, a skull defect and ventrally displaced bone fragment was identified between the brain mass lesion and subcutaneous tissue swelling detected on physical examination. This swelling appeared as hyperintensity on T2WI with contrast enhancement in the overlying temporalis muscle on T1WI (Fig 2). In cat 7, a skull defect was observed at the level of the left parietal lobe, which was the site of the previous debulking meningioma surgery.
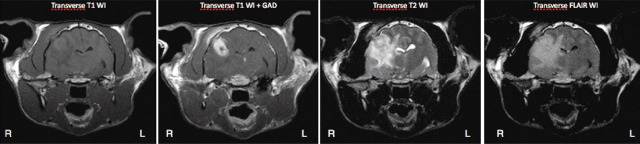
FIG 2.
MR images from case 2 — tranverse T1WI before and after gadolinium administration, T2WI and FLAIR. The images reveal an intra-axial lesion in the right frontoparietal lobe, with an isointense core surrounded by hypointense margins on T1WI, hyperintense on T2WI and on FLAIR, with marked contrast enhancement on T1WI. The mass is surrounded by a diffuse perilesional oedema which contributes to the mass effect on the brain parenchyma, causing a subfalcine brain herniation and midline shift. The muscles and subcutaneous tissue over the visible skull lesion are hyperintense on T2WI and show diffuse contrast uptake on T1WI
FIG 1.
Magnetic resonance (MR) images from case 1 — T1WI before and after gadolinium (GAD) administration, T2WI and FLAIR. The images reveal an intra-axial space-occupying lesion with well-defined margins in the right frontoparietal lobe, with an isointense core in FLAIR, hyperintense on T2WI and hypointense on T1WI with marked ring enhancement. The perilesional oedema is moderate in this case. The muscles and subcutaneous tissue above the brain lesion and the skull are hyperintense on T2WI and show diffuse contrast uptake on T1WI
Additional diagnostic tests
A complete blood count (CBC), serum biochemical analysis or blood gas analysis, urinalysis and infectious disease serology were performed by the referring veterinarian or on referral admission (see Table 1, which lists predominantly abnormal findings). Thoracic radiographs were obtained in cats 2 and 7, and were normal. Abdominal ultrasound was performed in cat 2 and revealed enlargement of the right kidney and mesenteric lymph nodes, and one loop of fluid-filled intestine, findings that were considered compatible with a mild nephropathy and enteropathy. Cerebrospinal fluid (CSF) collection was not attempted in any of the cats in view of the imaging findings suggestive of raised ICP. Swabs and fluid content collected from the intracranial abscess during surgery were submitted for aerobic and anaerobic bacterial culture in cats 1, 2, 5, 6 and 7, and were positive in three cats. Pasteurella multocida and Escherichia coli, sensitive to all antibiotics tested, including penicillin G, ampicillin, sulphadiazime/trimethoprim, clavulanic acid/amoxicillin, oxy-tetracycline, cephalexin, cefuroxime, cefovecin and enrofloxacin, were isolated in cases 7 and 1, respectively; Corynebacterium species were isolated in case 2, and found to be resistant to enrofloxacin and sulphadiazime/trimethoprim but sensitive to all other tested antibiotics.
TABLE 1.
Diagnostic tests performed on seven cats with brain abscess secondary to a bite wound
| Cat 1 | Cat 2 | Cat 3 | Cat 4 | Cat 5 | Cat 6 | Cat 7 | |
|---|---|---|---|---|---|---|---|
| Blood gas analysis | Mg 0.57 mmol/l (RI 0.35–0.55); Glucose 7.47 mmol/l (RI 4.20–6.60); Hb 11.1 g/dl (RI 12.0–18.0); PCV 31%; TS 82 | Mg 0.6 mmol/l (RI 0.35–0.55); Glucose 6.67 mmol/l (RI 4.20–6.60); PCV 37%; TS 80 | Not performed | Not performed | pH 7.45 (RI 7.24–7.40) | Urea 5.1 mmol/l (RI 5.36–12.14); Glucose 7.5 mmol/l (RI 3.33–7.22) | Not performed |
| Haematology | Unremarkable according to the referring vet | Lymphopenia 0.23 × 10 9 /l (RI 1.5–7) | Not performed | Within normal limits | RBC 3.9 × 10 12 /l (RI 5–10); HCT 28.5% (RI 30–45); PLT >100 × 10 3 /μl (RI 175–600) | Not performed | Lymphopenia 1.3 × 10 3 /mm 3 (RI 1.8–6.5) |
| Biochemistry | Unremarkable according to the referring vet | Urea 5.9 mmol/l (RI 6.1–12); ALT 23 U/I (RI 25–130); CK 7738 U/I (RI 52–506) | Not performed | Amyl 1796 U/l (RI 100–1200); Glucose 14.59 mmol/l (RI 3.33–7.2); P 0.83 mg/dl (RI 2.4–8.2) | Within normal limits | Not performed | Glucose 274.5 mg/dl (RI 76–145); Lipase 2488 U/l (RI 100–1400) |
| Urinalysis | Not performed | SG 1030; pH 7; no growth on culture | Not performed | Not performed | Not performed | Not performed | Not performed |
| FIV/FeLV | Not performed | Negative | Negative | Negative | Negative | Not performed | Negative |
| Coronavirus | Not performed | Not performed | Not performed | Not performed | Not performed | Not performed | Negative |
| Toxoplasma | Not performed | Not performed | Not performed | Not performed | Not performed | Not performed | IgG 1:256 IgM negative |
| Swab from abscess | Positive | Positive | Not performed | Not performed | Negative | Negative | Positive |
Mg = magnesium, Hb = haemoglobin, PCV = packed cell volume, TS = total solids, RBC = red blood cells, HCT = haematocrit, PLT = platelet count, ALT = alanine transaminase, CK = creatine kinase, P = phosphorus, Amyl = amylase, SG = specific gravity, RI = reference interval
Cytology of the abscess fluid was performed in cat 1 and was consistent with a marked septic suppurative inflammation. The vast majority of the nucleated cells were neutrophils, which ranged from non-degenerate to markedly degenerate; lower numbers of macrophages were present. A large mixed population of bacteria was seen (rods, filamentous rods, cocci), often found in colony-like aggregates and occasionally phagocytosed by neutrophils.
Treatment
All cats were managed with a combination of medical treatment, consisting of broad-spectrum antibiotics, and surgery performed within 3 days of referral admission. Because of rapid neurological deterioration and imaging evidence of suspected raised ICP, glucocorticoids and mannitol were given in almost all cases. Perioperative drugs are listed in Table 2.
TABLE 2.
Drug therapy, length of hospitalisation and outcome for seven cats with brain abscess secondary to a bite wound
| Route | Days Cat 1 | Days Cat 2 | Days Cat 3 | Days Cat 4 | Days Cat 5 | Days Cat 6 | Days Cat 7 | |
|---|---|---|---|---|---|---|---|---|
| Clavulanic acid plus amoxicillin | IV | 4 20mg/kg q8h | 10 20mg/kg q8h | 1 20mg/kg q8h | 5 17mg/kg q8h | |||
| PO | 30 12.5 mg/kg q12h | 50 12.5 mg/kg q12h | 28 20mg/kg q12h | 56 12.5 mg/kg q12h | ||||
| SC | 1 8 mg/kg q24h | |||||||
| Enrofloxacin | IV | 1 5mg/kg | 2 5mg/kg q12h | |||||
| PO | 56 5 mg/kg q12h | |||||||
| Marbofloxacin | IV | 5 2 mg/kg | ||||||
| SC | 2 2 mg/kg | |||||||
| PO | 4 2 mg/kg | |||||||
| Metronidazole | IV | 4 10 mg/kg q12h | 10 10 mg/kg q12h | 5 17 mg/kg q8h | 1 10 mg/kg q12h | |||
| PO | 16 10 mg/kg q12h | 50 10mg/kg q12h | 28 15mg/kg q12h | 4 10mg/kg q12h | ||||
| Sulphadiazime/trimethoprim | SC | 6 15mg/kg q12h | ||||||
| PO | 21 15 mg/kg q12h | |||||||
| Cephalosporin | IV | POp 22 mg/kg | POp 22 mg/kg | POp 22 mg/kg | 1 30mg/kg q6h | 4 22mg/kg q8h | ||
| IV | 2 20mg/kg q6h | POp 22 mg/kg | ||||||
| SC | 1 15mg/kg q24h | |||||||
| PO | 21 22 mg/kg q12h | |||||||
| Glucocorticoids | IV PO | 2 MPSS 30 mg/kg 1 Dex 0.2 mg/kg | 1 Dex 0.15 mg/kg | 1 MPSS 30 mg/kg | POp Dex 0.1 mg/kg 3 Dex 0.2 mg/kg | POp MPSS +1 30mg/kg 10 Pred1mg/kg 48 Pred 0.5 mg/kg | ||
| Furosemide | IV | 1 4mg/kg | DS 1mg/kg | |||||
| Mannitol | IV | POp 0.5 g/kg | POp 1 g/kg | POp 1g/kg twice | POp 1 g/kg | 1 1 g/kg stopped after 5 mins | POp 2 g/kg | DS 1g/kg |
| IV | 2 0.5 g/kg | 1 0.2 g/kg | 1 1g/kg | |||||
| Phenobarbitone | IV | 2 2mg/kg q12h | 2 3mg/kg q12h | POp 5.7 mg/kg | 4 3mg/kg | |||
| PO | 180 3 mg/kg q12h | 2 1.5 mg/kg q12h | ||||||
| Omeprazole | IV | 4 1mg/kg | ||||||
| Ranitidine | IV | 1 2mg/kg | ||||||
| Hospitalisation | 5 Recovered | 14 Recovered | 1 Euthan | 1 Euthan | 10 Recovered | 7 Recovered | 9 Recovered |
POp = perioperative, DS = during surgery, MPSS = methylprednisolone sodium succinate, Dex = dexamethasone, Pred = prednisolone, Euthan = euthanased
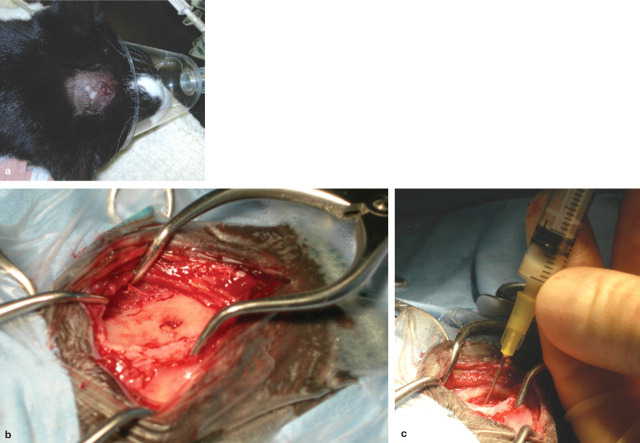
All cats were treated surgically via a rostro-tentorial craniectomy centered on the defect in the parietal bone (Fig 3). At surgery, the fascia and temporalis muscle appeared focally torn and necrotic and, below, a small penetrating fracture was detected in all cats. On completion of the craniectomy, the underlying brain appeared swollen and a mucopurulent discharge was present immediately in the surgical site. Swab and fluid content were taken for aerobic and anaerobic bacterial culture and susceptibility testing in five cats (1, 2, 5, 6 and 7). A large amount of purulent material was drained and a tooth fragment was found within the content of the abscess in cats 4 and 7. The surgical site was flushed with sterile saline and abnormal brain tissue was debrided. After extensive flushing the meninges were left open to allow for drainage; in cat 3 antibiotic was instilled (benzylpenicillin sodium, Crystapen; Genus Pharmaceuticals). The healthy fascia of the temporalis muscle was reattached to its origin, the subcutaneous abscess was removed, and subcutaneous tissue and skin were closed. In one case (cat 1) a drain was left in place for 3 days.
FIG 3.
Surgical treatment of cat 1. (a) Presurgical appearance of the skin lesion. (b) Intraoperative view of the skull defect; purulent material is arising from the abscess. (c) Drainage and retrieval of pus from the brain abscess
Outcome.
Outcome was determined based on at least one re-examination at the referral centre in four cats (cases 2, 5, 6 and 7); follow-up of case 1 was obtained by means of owner telephone progress report 4 weeks after discharge. Two cats (cases 3 and 4), which required ventilatory support upon induction of anaesthesia, failed to regain consciousness and respiratory drive following surgery and were euthanased at the owners’ request within 1 h of surgery.
Cats 1, 2, 5, 6 and 7 improved significantly and were discharged within 3–12 days of surgery. At the time of discharge, neurological deficits were found, such as a unilateral reduced menace response in cats 5, 6 and 7, and ambulatory tetraparesis and an absent menace response in cat 2; neurological examination was normal in cat 1. Cats 2, 5, 6 and 7 were re-examined within 2–7 weeks of surgery and found to be normal except for a slightly reduced menace response in the left eye of cat 6.
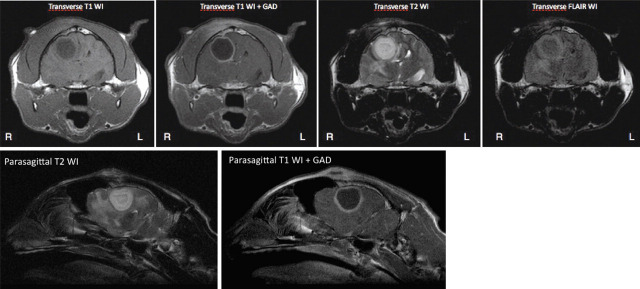
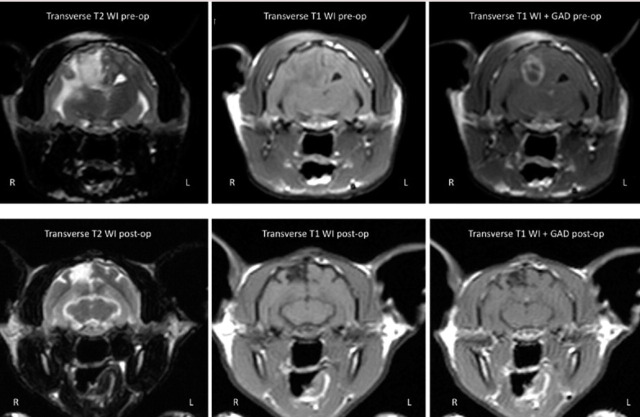
Cat 6 had a repeat MRI examination 7 weeks after surgery that showed a CSF cavity at the site of the previously resected abscess and no contrast enhancement (Fig 4). Cat 7 underwent repeat MRI of the brain 14 days after surgery, revealing an ex vacuo dilatation of the right ventriculus, and meningeal and superficial soft tissue contrast uptake at the site of the resected abscess.
FIG 4.
MR images from case 6 before and 7 weeks after surgery — transverse T1WI before and after gadolinium (GAD) administration, and T2WI. The preoperative images reveal an intra-axial lesion in the right parietal lobe, hyperintense on T2WI and hypointense on T1WI, with strong ring enhancement after gadolinium administration. The right temporalis muscle and the subcutaneous tissue above the brain lesion are hyperintense on T2WI and T1WI and show contrast uptake. The perilesional oedema is severe in this case, with midline shift. Post-surgery MRI scans of the brain reveal a CSF fluid cavity at the site of the previous resected abscess, with no contrast enhancement or parenchymal oedema
Discussion
This case series documents the occurrence of brain abscess subsequent to a bite wound in seven cats. All affected animals were presented several days after the injury with neurological signs consistent with a forebrain lesion; in one cat there were associated brainstem signs as well. In all cases a focal wound or a healed wound was observed on the dorsal part of the head on physical examination, and two cats were pyrexic (39.4°C and 41.1°C).
In the reviewed literature there are only two veterinary case reports of a successfully treated brain abscess due to a bite wound, one in a dog 7 and one in a cat, 12 and few reports in humans, 13–16 all of which have been treated with a combination of medical and surgical therapy; in a further report, a brain abscess in a cat due to a bite wound was diagnosed by post-mortem examination. 3 In human medicine, an intracranial pyogenic bacterial focus of infection remains a potentially fatal condition despite modern neurosurgical techniques, antibiotic treatment and the use of advanced imaging, such as computed tomography (CT) and MRI, allowing prompt diagnosis.
The successful management of brain abscesses depends on early recognition, the site of entry, surgical treatment, optimal culture conditions and use of the appropriate antibiotic. With respect to pathogenesis, brain abscesses are almost always secondary to a focus of infection elsewhere in the body, and may develop either after neurosurgery or brain trauma. 17 There is the additional possibility of infection resulting from bite wounds and migrating foreign body material.
Stages of abscess development
Based on an animal model with CT scans, a series of stages of abscess development has been described: 18
Days 1–3, ‘early cerebritis' This stage is characterised by a necrotic central focus, oedema, and a surrounding zone of perivascular inflammatory infiltrate comprising polymorphonuclear cells, lymphocytes and plasma cells.
Days 4–9, ‘late cerebritis' The necrotic zone becomes more discrete and is surrounded by a zone of hyperplastic fibroblasts and neovascularisation, extracellular oedema and hyperplastic astrocytes.
Days 10–14, ‘early capsule' At this stage a distinct collagen capsule begins to appear with a well developed layer of fibroblasts and an associated persistent cerebritis and neovascularity.
From day 14, ‘late capsule' This stage corresponds to the completion and thickening of the capsule, which directly limits the spread of infection. In this late phase, there is ongoing encapsulation and the necrotic centre continues to reduce in diameter.
In all seven cats, MRI revealed an intra-axial mass lesion that was diffusely hypointense on T1WI, with a hyperintense core and hypointense peripheral ring on T2WI. This was causing a severe mass effect on adjacent brain parenchyma with subfalcine, caudal subtentorial and foramen magnum herniation, as well as severe perilesional white matter oedema (Figs 1, 2 and 4). Differentials considered based on the results of both neurological examination and MRI included an infectious CNS disease and a primary or metastatic brain tumour. Meningiomas are the most common brain tumour in cats and they have a varied appearance on T1WI and T2WI, usually isointense and in some cases hypointense on T1WI and hyperintense on T2WI; however, these tumours tend to show homogeneous contrast enhancement and are extra-axial in location. Ring enhancement is often associated with gliomas, but these neoplasms arise from an intra-axial location.
According to the reviewed literature, 19–21 the MRI findings in our cases were suggestive of an abscess in the late cerebritis phase (see box).
Therapeutic approach
The anatomic location, number and size of abscesses, as well as the stage of abscess formation and neurological status of the patient, can influence the strategy for managing brain abscessation. Frequently a combination of medical and surgical treatment is required.
MRI features.
In the first phase, a brain abscess appears to be hypointense on T1WI and hyperintense on T2WI and FLAIR images. In the late phase, ring enhancement may be present, and it is sometimes possible to observe a thin-walled rim of high signal (isointense to slightly hyperintense) on T1WI and hypointense on T2WI/FLAIR pre-contrast images; this is most likely due to paramagnetic free radicals secondary to the oxidative effect of the respiratory burst of the bacteria and produced within macrophages during active phagocytosis at the abscess rim. Typically, a mature abscess appears on T1WI as a round and well-demarcated hypointense region with mass effect and peripheral low intensity oedema beyond the margins of the lesion. In T2WI and FLAIR images the necrotic material is hyperintense relative to the CSF and to the surrounding parenchyma of the brain. After gadolinium administration, the abscess always shows ring enhancement and, less commonly, a multiloculated enhancement.
Brain abscesses may sometimes mimic necrotic tumours and cystic metastases, but recent studies have shown that cerebral abscesses show restricted diffusion on diffusion-weighted imaging (DWI). 22
Neuroimaging studies have been the most useful diagnostic tools in detecting and localising early brain abscesses. 17
A non-surgical approach is only possible when the aetiological agent is known based on positive cultures from CSF or fluid drained from the abscess. In the present cases, CSF collection was not performed due to the risk of brain herniation associated with raised ICP. Furthermore, CSF evaluation may be of little value in excluding an abscess from the differential diagnosis list as cultures are often negative in the face of bacterial infection of the CNS, and CSF analysis is rarely specific for bacterial abscesses. 23,24
Antibiotics
All patients were started on broad-spectrum antibiotics while awaiting the results of culture of swab material and fluid collected from the abscess during surgery. Positive cultures were obtained in three out of four cats for P multocida, E coli and Corynebacterium species, reflecting the most common bacteria found in a cat's mouth. In a study from Sweden where oral swabs were collected from 38 cats that had bitten humans, microbial culture yielded Pasturella species in 30 (79.9%) cats; 27 of the 30 (90%) samples yielded P multocida (one sample yielded P haemolytica, and two microbial growths were not speciated). Additional isolates included Prevotella oris-buccae and Enterobacter cloacae (from one sample each). Cultures of samples collected via gingival scraping from a group of 25 control cats all yielded P multocida; a member of the Enterobacteriaceae family and viridians group streptococci were detected in samples from two and one control cat(s), respectively. 25
Rational antimicrobial therapy in patients with brain abscessation depends on selecting antibiotics that are able to penetrate the blood—brain barrier and into the abscess cavity and that have good activity against the suspected pathogens. Ideally, intravenous therapy is recommended for at least the first 3–5 days of therapy; moreover in humans at least a 6- to 8-week treatment course is war-ranted. 17 The blood–brain barrier prevents the diffusion of many antibiotics in the CNS and this represents a major limitation with regard to reaching therapeutic drug concentrations in the CSF. High intravenous doses of ampicillin and third generation cephalosporins cross both healthy and inflamed meninges extremely well, 26,27 enrofloxacin and metronidazole are excellent antibiotics and trimethoprim-sulfonamide is bactericidal and readily penetrates the blood—brain barrier, even when it is not inflamed. 27
Glucocorticoids
Five of seven cats received glucocorticoids for a period ranging from 1–58 days. Although glucocorticoid use in the face of infection is usually contraindicated, in human medicine there is abundant evidence that a transient anti-inflammatory dose of dexamethasone (0.15 mg/kg) q6h for 4 days can lead to lower ICP, lower inflammatory mediator concentrations, less CNS inflammation and generally a significant improvement in outcome in people with bacterial meningitis. 28–30 Inflammatory mediators, such as tumour necrosis factor, prostaglandins, interferons and interleukin-1, are produced in response to bacteria and bacterial cell wall lysis by the white blood cells attracted to the infection focus as a result of chemotaxis, and promote meningeal and ependymal inflammation resulting in oedema, infarction and vasculitis.
Successful management of brain abscess depends on early recognition, the site of entry, surgical treatment, optimal culture conditions and use of the appropriate antibiotic.
Our patients were treated with several different glucocorticoids. Three cats received methylprednisolone sodium succinate on the assumption that a high dose protocol of this drug would provide benefit via free radical scavenging action; however, a recent study has disputed this hypothesis. 31 Based on evidence published in the human literature, dexamethasone may have been a more appropriate choice in our cats.
Mannitol
In addition, and in accordance with the literature, all patients received mannitol at least once during surgery, in order to decrease ICP. Mannitol is considered the first-line therapy for decreasing ICP, promoting the shift of water from the intracellular and interstitial spaces of the brain to the vasculature, inducing an osmotic diuresis and reducing cerebral oedema. 32 Moreover, it has also been reported to limit secondary oxidative injury in the brain. 33
Surgery
In addition to intensive care and intravenous antimicrobials, all our patients underwent surgical treatment consisting of a rostrotentorial craniectomy, removal of the content of the abscess and extensive flushing of the surgical site before closing. In human medicine surgical management of brain abscesses has evolved recently with the development of mini-invasive surgical techniques such as stereotactic aspiration of the abscess. Surgical intervention is considered the gold standard treatment for brain abscess 34 and, at the same time, it allows collection of material from within the abscess itself for definitive diagnosis and culture/sensitivity testing. Furthermore, in the current series of cases, surgical treatment enabled the removal of skull fragments and foreign bodies, such as the tooth fragments found in two cats, that may represent a continuing focus of infection.
Conclusions
This is the first case series and, to our knowledge, only the third report of treatment of brain abscess due to a bite wound in companion animals, and the second in cats. This series indicates that successful management in such cases depends on early recognition, and combined used of antimicrobials and surgical intervention in order to remove skull and foreign body (tooth) fragments that may represent a continuing focus of infection.
References
- 1. Roos K. Nonviral infections In: Goetz C, Pappert E, eds. Textbook of clinical neurology. Philadelphia: WB Saunders, 2000; 842–67. [Google Scholar]
- 2. Sturges BK, Dickinson PJ, Kortz GD, et al. Clinical signs, magnetic resonance imaging features, and outcome after surgical and medical treatment of otogenic intracranial infection in 11 cats and 4 dogs. J Vet Intern Med 2006; 20: 648–56. [DOI] [PubMed] [Google Scholar]
- 3. Barrs VR, Nicoll RG, Churcher RK, Beck JA, Beatty JA. Intracranial empyema: literature review and two novel cases in cats. J Small Anim Pract 2007; 48: 449–54. [DOI] [PubMed] [Google Scholar]
- 4. Mateo I, Lorenzo V, Muñoz A, Pumarola M. Brainstem abscess due to plant foreign body in a dog. J Vet Intern Med 2007; 21: 535–38. [DOI] [PubMed] [Google Scholar]
- 5. Bach JF, Mahony OM, Tidwell AS, Rush JE. Brain abscess and bacterial endocarditis in a Kerry Blue Terrier with a history of immune-mediated thrombocytopenia. J Vet Emerg Crit Care 2007; 17: 409–15. [Google Scholar]
- 6. Kent M. Bacterial infections of the central nervous system. In: Greene CE, ed. Infectious diseases of the dog and cat. 3rd edn. St Louis: Saunders/Elsevier, 2006: 962–974. [Google Scholar]
- 7. Bilderback AL, Faissler D. Surgical management of a canine intracranial abscess due to a bite wound. J Vet Emerg Crit Care 2009; 19: 507–12. [DOI] [PubMed] [Google Scholar]
- 8. Smith PM, Haughland SP, Jeffery ND. Brain abscess in a dog immunosuppressed using cyclosporine. Vet J 2007; 173: 675–78. [DOI] [PubMed] [Google Scholar]
- 9. Irwin PJ, Parry BW. Streptococcal meningoencephalitis in a dog. J Am Anim Hosp Assoc 1999; 35: 417–22. [DOI] [PubMed] [Google Scholar]
- 10. Vite CH. Inflammatory diseases of the central nervous system. In: Vite CH, ed. Braund's clinical neurology in small animals: localization, diagnosis and treatment. Ithaca, NY: International Veterinary Information Service. Available at http://www.ivis.org. [Google Scholar]
- 11. Kent M. Bacterial infections of the central nervous system. In: Greene CE, ed. Infectious diseases of the dog and cat. s3rd edn. St Louis, Saunders/Elsevier, 2006: 962–74. [Google Scholar]
- 12. Wouters EGH, Beukers M, Theyse LFH. Surgical treatment of a cerebral brain abscess in a cat. Vet Comp Orthop Traumatol 2011; 24: 72–75. [DOI] [PubMed] [Google Scholar]
- 13. Santana-Montero BL, Ahumada-Mendoza H, Vaca-Ruíz MA, et al. Cerebellar abscesses caused by dog bite: a case report. Childs Nerv Syst 2009; 25: 1137–41. [DOI] [PubMed] [Google Scholar]
- 14. Ulivieri S, Oliveri G, Filosomi G. A case of Capnocytophaga canimorsus brain abscess secondary to dog's bite. G Chir 2008; 29: 79–80. [PubMed] [Google Scholar]
- 15. Sutton LN, Alpert G. Brain abscess following cranial dog bite. Clin Pediatr (Phila) 1984; 23: 580. [PubMed] [Google Scholar]
- 16. Klein DM, Cohen ME. Pasteurella multocida brain abscess following perforating cranial dog bite. J Pediatr 1978; 92: 588–89. [DOI] [PubMed] [Google Scholar]
- 17. Lu CH, Chang WN, Lui CC. Strategies for the management of bacterial brain abscesses. J Clin Neurosci 2006; 13: 979–85. [DOI] [PubMed] [Google Scholar]
- 18. Britt RH, Enzmann DR, Yeager AS. Neuropathological and computerized tomographic findings in experimental brain abscess. J Neurosurg 1981; 55: 590–603. [DOI] [PubMed] [Google Scholar]
- 19. Grossman RI, Yousem DM. Infectious and noninfectious inflammatory diseases of the brain. In: Neuroradiology: the requisites. 2nd edn. St Louis, Elsevier, 2003: 273–330. [Google Scholar]
- 20. Weingarten K, Zimmerman RD, Becker RD, Heier A, Haimes AB, Deck MDF. Subdural and epidural empyemas: MR imaging. AJNR Am J Neuroradiol 1989; 10: 81–87. [DOI] [PubMed] [Google Scholar]
- 21. Seiler G, Czinauskas S, Scheidegger J, Lang J. Low-field magnetic resonance imaging of a pyocephalus and a suspected brain abscess in a German Shepherd dog. Vet Radiol Ultrasound 2001; 42: 417–22. [DOI] [PubMed] [Google Scholar]
- 22. Chang SC, Lai PH, Chen WL, et al. Diffusion-weighted MRI features of brain abscess and cystic or necrotic brain tumors: comparison with conventional MRI. Clin Imaging 2002; 26: 227–36. [DOI] [PubMed] [Google Scholar]
- 23. Radaelli ST, Platt SR. Bacterial meningoencephalomyelitis in dogs: a retrospective study of 23 cases (1990–1999). J Vet Intern Med 2002; 6: 159–163. [DOI] [PubMed] [Google Scholar]
- 24. Munana KR. Encephalitis and meningitis. Vet Clin North Am Small Anim Pract 1996; 26: 857–74. [PubMed] [Google Scholar]
- 25. Westling K, Farra A, Cars B, et al. Cat bite wound infections: a prospective clinical and microbiological study at three emergency wards in Stockholm, Sweden. J Infect 2006; 53: 403–7. [DOI] [PubMed] [Google Scholar]
- 26. Fenner WR. Central nervous system infections. In: Greene CE, ed. Infectious diseases of the dog and cat. Philadelphia, WB Saunders, 1998: 647–57. [Google Scholar]
- 27. Dewey CW. Encephalopathies: disorders of the brain. In: A practical guide to canine and feline neurology. 2nd edn. Oxford: Wiley-Blackwell, 2008: 115–220. [Google Scholar]
- 28. Jafari H, McCracken GJ. Dexamethasone therapy in bacterial meningitis. Pediatr Ann 1994; 23: 82–88. [DOI] [PubMed] [Google Scholar]
- 29. Coyle PK. Glucocorticoids in central nervous system bacterial infection. Arch Neurol 1999; 56: 796–801. [DOI] [PubMed] [Google Scholar]
- 30. de Gans J, van de Beek D. Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347: 1549–56. [DOI] [PubMed] [Google Scholar]
- 31. Edwards P, Arango M, Balica L, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroids in adults with head injury — outcome at 6 months. Lancet 2005; 365: 1957–59. [DOI] [PubMed] [Google Scholar]
- 32. Sande A, West C. Traumatic brain injury: a review of patho-physiology and management. J Vet Emerg Crit Care 2010; 2: 177–90. [DOI] [PubMed] [Google Scholar]
- 33. Mizoi K, Suzuki J, Imaizumi S, Yoshimoto T. Development of new cerebral protective agents: the free radical scavengers. Neurol Res 1986; 8: 75–80. [DOI] [PubMed] [Google Scholar]
- 34. Hakan T, Ceran N, Erdem I, Berkman MZ, Gökta P. Bacterial brain abscesses: an evaluation of 96 cases. J Infect 2006; 52: 359–66. [DOI] [PubMed] [Google Scholar]