Abstract
Introduction
Patients with type 2 diabetes have lower quality of life, which is further impaired by diabetes complications and comorbidities. This study aims to evaluate the impact of diabetes complications and comorbidities on EuroQol Five-Dimension Three-Level (EQ-5D-3L) scores among patients with type 2 diabetes with ongoing oral drug treatments in China.
Methods
This retrospective cross-sectional analysis included 9570 patients with type 2 diabetes on oral drug treatments, who were enrolled from 75 hospitals in nine cities in China. Patient characteristics, including demographic data, health conditions, oral treatment history, and health insurance coverage, were collected through self-reported questionnaires. Health utility was measured by the EQ-5D-3L scale in the questionnaire and a Chinese version of the EQ-5D-3L scoring weights was applied in the analysis. The associations between complications and health utility were assessed using linear regression.
Results
A total of 7081 patients with complete survey data were included in the analytic sample; 3479 (49.13%) patients were female. The mean age was 59.6 years old, with a standard deviation (SD) of 12.64. The average duration with type 2 diabetes was 7.91 (SD = 6.22) years. A total of 5189 (73.28%) patients reported complications. Hypertension (51.25%) and hyperlipidemia (28.90%) were the most common complications. Other complications reported by patients included cardiovascular disease, stroke, retinopathy, nephropathy, diabetic foot, and hypoglycemia. On average, each patient had 1.54 complications. All complications and comorbidities decreased the EQ-5D-3L score. Among patients with complications, the worst effect on EQ-5D-3L score was caused by diabetic foot, decreasing by 0.118 (p < 0.001), followed by stroke (decreasing by 0.101, p < 0.001) and nephropathy (decreasing by 0.058, p < 0.001).
Conclusion
The diabetes complications and comorbidities among patients with type 2 diabetes were associated with poor health utility scores, especially for those with diabetic foot, stroke, and nephropathy.
Keywords: Complications, Quality of life, Type 2 diabetes
Key Summary Points
| Seventy-three percent of the Chinese patients with type 2 diabetes surveyed had at least one diabetes complication. |
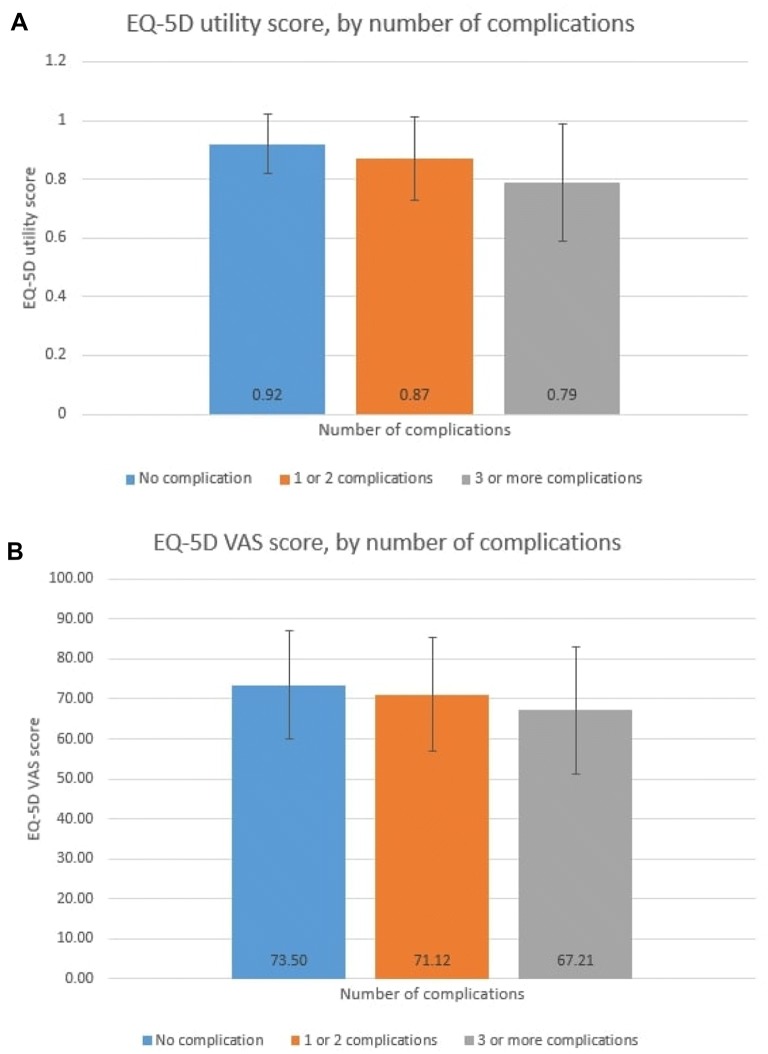
| Increased numbers of diabetes complications are associated with worse EQ-5D utility index and EQ-5D VAS score. |
| Cardiovascular disease, stroke, retinopathy, nephropathy, diabetic foot, and symptomatic hypoglycemia event were associated with EQ-5D disutility of 0.007–0.118. |
| Duration of type 2 diabetes for 10 years or longer had lower EQ-5D utility by 0.014. |
Introduction
Diabetes is an important public health problem in China. The prevalence rate of type 2 diabetes in China has increased from less than 5% of the Chinese population in the 1980s to more than 10% at present [1]. Diabetes-related complications are common in both outpatient and inpatient settings [2] and range in prevalence rate from 50% in outpatients to 90% in inpatients [3–5]. Common complications of type 2 diabetes include skin complications, eye complications, neuropathy, foot complications, nephropathy, hypertension, stroke, and heart diseases [6]. In the Chinese population, hypertension was identified as the most prevalent complication for Chinese patients with type 2 diabetes, followed by ischemic heart disease and chronic kidney disease [7].
Moreover, direct medical expenses for patients with diabetes and complications are higher than those of patients without complications, and they increase with increases in the number of complications [2, 8]. From 2009 to 2011, there was an increasing trend in diabetes-related medical costs in China, from USD 1655 to USD 1857 [8]. Indirect medical costs, such as transportation, and loss in labor productivity due to health conditions can also be a huge financial burden on patients. For the health system, the estimated healthcare expenditure due to diabetes in 2017 was USD 549.4 per person with diabetes and total healthcare expenditure was USD 63.1 billion [9].
Patients with type 2 diabetes have lower health-related quality of life compared with healthy individuals [10]. Patients with cardiovascular complications or diabetic retinopathy had lower quality of life than patients with type 2 diabetes only [11–13]. Each additional complication can further decrease the health-related quality of life for patients with type 2 diabetes. In China, a previous study found that patients with type 2 diabetes experienced poor quality of life, and complications were associated with decreased quality of life [14]. A previous study in Taiwan focusing on patients with type 2 diabetes in outpatient settings found that greater negative impact of diabetes on quality of life was associated with younger age, male sex, more educated with low income, more diabetes complications, higher hemoglobin A1c (HbA1c), and using insulin [15].
In economic evaluation research, quality-adjusted life-years (QALYs) are widely used to address the benefit or harm of health interventions. QALYs are also commonly accepted as a reference standard to use in cost-effectiveness analysis. Health utility, as a measurement of QALYs, is the preferred value to represent patients’ overall health status. Ranging from 0 (equal to death) to 1 (equal to perfect health), health utility can summarize both positive and negative impacts of health interventions on health outcomes. By using health utility, it allows researchers to compare the health outcomes for different health conditions or different health interventions, and so on [16]. Many previous studies in health technology assessment have applied the EuroQol Five-Dimension questionnaire (EQ-5D) in measuring health utility, because it has both a qualitative evaluation method, the visual analogue score (VAS), and quantitative evaluation method, the preference-based measures [17].
Despite diabetes being an important public health issue in China, no previous studies have been conducted to estimate the decrements in health-related quality of life based on each complication condition among patients with type 2 diabetes in China. It is important and urgent to quantify the decrements in health to better understand the impact of each complication and to improve healthcare delivery for Chinese patients. The findings from this study can be further used in cost-effectiveness analysis of certain health interventions to improve quality of life among patients with type 2 diabetes on oral treatments and with complications. It can also provide recommendations for policymakers regarding healthcare resource allocation. The present study aimed to estimate the decrements of EuroQol Five-Dimension Three-Level (EQ-5D-3L) scores by diabetes complications and comorbidities in patients with type 2 diabetes and ongoing oral drug treatments in China.
Methods
Study Population
This study used secondary data from Han et al.’s study [14] conducted in China. The study randomly enrolled 9570 patients with type 2 diabetes and ongoing oral drug treatment from 75 hospitals in nine cities in China. Inclusion criteria were (1) patients must be at least 18 years old; (2) patients’ health conditions were qualified according to the 1999 World Health Organization (WHO) diagnostic standards of type 2 diabetes; (3) patients must have been on oral drugs constantly or inconstantly after being diagnosed but have not taken insulin as treatment; and (4) patients did not have cognitive function problems or problems in answering questions, and they were willing to participate in the study. Survey questionnaires were used to collect data [14]. This study used de-identified secondary data from a previous Chinese study. Informed consent was obtained prior to data collection. The previous study and data collection were approved by the Ethics Committee of Peking University People’s Hospital.
Data Source
Survey questionnaires were used to collect data in Han et al.’s study [14]. Data collected in the questionnaires included (1) sociodemographic characteristics, such as gender, age, education level, health insurance coverage, employment status, and income level; (2) medical history, such as body mass index (BMI), duration of type 2 diabetes, complications, and blood pressure; (3) EQ-5D-3L scale, including EQ-5D health utility and EQ-VAS (visual analogue scale).
Measurements
Health Utility
The EQ-5D-3L was used to measure health utility. EQ-5D is the most commonly used generic health status measurement. It contains health state description and evaluation. The health state description includes morbidity, self-care, usual activities, pain/discomfort, and anxiety/depression. In order to adapt this scale to the study population, it was scored by a Chinese version of the EQ-5D-3L scoring weights. Self-reported health status was calculated by EQ-VAS scale.
Explanatory Variables
Age, gender, education level, years since diagnosis were included from the survey questionnaire. Disease histories of hypertension, cardiovascular disease, stroke, retinopathy, nephropathy, diabetic foot, and hypoglycemia were included in the questionnaire. Hypoglycemia was further divided into symptomatic hypoglycemia and severe hypoglycemia.
Data Analysis
In the present study, descriptive analysis was performed to demonstrate the characteristics of the study population, including sociodemographic characteristics, complication rates, and EQ-5D health utility. Linear regression was used to analyze the associations between complications and health utility. The analysis was performed in Stata 10.
Results
Study Population
Among 9577 surveys, 7081 patients had complete information of interest. Mean age was 59.60 (standard deviation (SD) = 12.64) years old, 3479 (49.13%) patients were female, and average duration of type 2 diabetes was 7.91 (SD = 6.22) years. A total of 5189 (73.28%) patients had at least one complication.
To further describe the sociodemographic characteristics of the study population, patients were categorized into three groups based on the total number of complications: patients with no complications, patients with one to two complications, and patients with three or more complications (Table 1). Within each category, age, gender, education level, employment status, and monthly income level were significantly differently distributed. Patients with more complications were at least 60 years old. Over 85% of all the patients (n = 6036) had at least moderate elevation in HbA1c level (HbA1c ≥ 7%).
Table 1.
Demographic characteristics by number of complications
| Overall | No complication | 1 or 2 complications | 3 or more complications | |
|---|---|---|---|---|
| Total | 7081 (100.00) | 1892 (26.72) | 3613 (51.02) | 1576 (22.26) |
| Age, mean (SD)a | 59.60 (12.64) | 53.82 (12.37) | 60.12 (12.14) | 65.31 (11.12) |
| Age, N (%)a | ||||
| ≤ 45 years old | 873 (12.33) | 437 (23.10) | 376 (10.41) | 60 (3.81) |
| 46–59 years old | 2777 (39.22) | 892 (47.15) | 1418 (39.25) | 467 (29.63) |
| ≥ 60 years old | 3431 (48.45) | 563 (29.76) | 1819 (50.35) | 1049 (66.56) |
| Gender, N (%)a | ||||
| Male | 3602 (50.87) | 1075 (56.82) | 1821 (50.40) | 706 (44.80) |
| Female | 3479 (49.13) | 817 (43.18) | 1792 (49.60) | 870 (55.20) |
| Education levels, N (%)a | ||||
| Bachelor and above | 1346 (19.01) | 433 (22.89) | 689 (19.07) | 224 (14.21) |
| High school | 2252 (31.80) | 685 (36.21) | 1157 (32.02) | 410 (26.02) |
| Middle school and below | 3483 (49.19) | 774 (40.91) | 1767 (48.91) | 942 (59.77) |
| Employment status, N (%)a | ||||
| Employed | 1861 (26.28) | 788 (41.65) | 897 (24.83) | 176 (11.17) |
| Unemployed | 1077 (15.21) | 251 (13.27) | 546 (15.11) | 280 (17.77) |
| Retired | 3968 (56.04) | 794 (41.97) | 2094 (57.96) | 1080 (68.53) |
| Students | 9 (0.13) | 5 (0.26) | 3 (0.08) | 1 (0.06) |
| Others | 166 (2.34) | 54 (2.85) | 73 (2.02) | 39 (2.47) |
| Monthly income, N (%)a | ||||
| Less than RMB 2000 | 4198 (59.29) | 967 (51.11) | 2142 (59.29) | 1089 (69.10) |
| RMB 2001–5000 | 2402 (33.92) | 761 (40.22) | 1221 (33.79) | 420 (26.65) |
| RMB 5001–10,000 | 384 (5.42) | 132 (6.98) | 197 (5.45) | 55 (3.49) |
| More than 10,000 | 97 (1.37) | 32 (1.69) | 53 (1.47) | 12 (0.76) |
| Duration of type 2 diabetes, years, mean (SD)a | 7.91 (6.22) | 5.77 (5.20) | 7.86 (6.01) | 10.59 (6.76) |
| BMI level, N (%)a | ||||
| Normal/healthy (≤ 25 kg/m2) | 4321 (61.02) | 1337 (70.67) | 2157 (59.70) | 827 (52.47) |
| Overweight (25–30 kg/m2) | 2378 (33.58) | 502 (26.53) | 1254 (34.71) | 622 (39.47) |
| Obese (≥ 30 kg/m2) | 382 (5.39) | 53 (2.80) | 202 (5.59) | 127 (8.06) |
| HbA1c level, N (%)a | ||||
| Mild elevation (< 7%) | 1045 (14.76) | 274 (14.48) | 509 (14.09) | 262 (16.62) |
| Moderate elevation (7–9%) | 3008 (42.48) | 745 (39.38) | 1529 (42.32) | 734 (46.57) |
| Severe elevation (> 9%) | 3028 (42.76) | 873 (46.14) | 1575 (43.59) | 580 (36.80) |
aComparison between complication groups p < 0.0001
EQ-5D Health Utility
The average EQ-5D utility was 0.87 (SD = 0.15) and the mean EQ-5D VAS was 70.89 (SD = 14.60) (Table 2). It varied significantly across age groups, gender, education levels, employment status, and monthly income levels.
Table 2.
EQ-5D health utility by demographic characteristics
| EQ-5D health utility (range 0–1) | EQ-5D VAS (range 0–100) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | p value | Mean | SD | p value | |
| Total | 0.87 | 0.15 | 70.89 | 14.60 | ||
| Age | < 0.001 | < 0.001 | ||||
| ≤ 45 years old | 0.92 | 0.09 | 73.06 | 14.36 | ||
| 46–59 years old | 0.90 | 0.12 | 72.04 | 14.47 | ||
| ≥ 60 years old | 0.83 | 0.18 | 69.40 | 14.62 | ||
| Gender | < 0.001 | < 0.001 | ||||
| Male | 0.88 | 0.14 | 71.76 | 14.42 | ||
| Female | 0.85 | 0.16 | 69.98 | 14.73 | ||
| Education levels | < 0.001 | < 0.001 | ||||
| Bachelor and above | 0.90 | 0.11 | 74.05 | 13.91 | ||
| High school | 0.88 | 0.13 | 72.22 | 14.18 | ||
| Middle school and below | 0.84 | 0.18 | 68.80 | 14.81 | ||
| Employment status | < 0.001 | < 0.001 | ||||
| Employed | 0.92 | 0.09 | 74.01 | 14.00 | ||
| Unemployed | 0.82 | 0.20 | 67.15 | 15.43 | ||
| Retired | 0.86 | 0.16 | 70.56 | 14.16 | ||
| Students | 0.92 | 0.06 | 80.28 | 13.47 | ||
| Others | 0.85 | 0.15 | 67.39 | 18.41 | ||
| Monthly income | < 0.001 | < 0.001 | ||||
| Less than RMB 2000 | 0.85 | 0.17 | 69.30 | 14.78 | ||
| RMB 2001–5000 | 0.89 | 0.13 | 72.85 | 14.04 | ||
| RMB 5001–10,000 | 0.92 | 0.10 | 74.21 | 13.56 | ||
| More than 10,000 | 0.92 | 0.09 | 77.70 | 14.70 | ||
| BMI level | 0.1188 | 0.9813 | ||||
| Normal/healthy (≤ 25 kg/m2) | 0.87 | 0.15 | 70.86 | 14.71 | ||
| Overweight (25–30 kg/m2) | 0.87 | 0.15 | 70.93 | 14.35 | ||
| Obese (≥ 30 kg/m2) | 0.85 | 0.18 | 70.91 | 15.03 | ||
| HbA1c level | 0.010 | 0.002 | ||||
| Mild elevation (< 7%) | 0.88 | 0.15 | 73.03 | 15.50 | ||
| Moderate elevation (7–9%) | 0.87 | 0.15 | 71.56 | 14.21 | ||
| Severe elevation (> 9%) | 0.86 | 0.16 | 69.48 | 14.54 | ||
Complications
The most prevalent complication in the study population was hypertension; 3629 (51.25%) patients had hypertension, followed by hyperlipidemia (2046 patients, 28.89%), and retinopathy (1341 patients, 18.94%). Other most prevalent complications included in the questionnaire were cardiovascular disease (18.30%), neuropathy (14.80%), nephropathy (10.97%), stroke (8.33%), and diabetic foot (3.45%) (Table 3).
Table 3.
Complication rates and decrements on EQ-5D scale
| Complications | N (%) | EQ-5D health utility | EQ-5D VAS | ||
|---|---|---|---|---|---|
| Mean (SD) | p value | Mean (SD) | p value | ||
| Hypertension | 3629 (51.25) | 0.85 (0.17) | < 0.001 | 69.79 (14.64) | < 0.001 |
| CVD | 1296 (18.30) | 0.81 (0.19) | < 0.001 | 68.32 (15.56) | < 0.001 |
| Hyperlipidemia | 2046 (28.89) | 0.85 (0.16) | < 0.001 | 70.57 (15.36) | 0.2414 |
| Stroke | 590 (8.33) | 0.74 (0.24) | < 0.001 | 65.92 (15.91) | < 0.001 |
| Retinopathy | 1341 (18.94) | 0.81 (0.18) | < 0.001 | 67.30 (15.55) | < 0.001 |
| Neuropathy | 1048 (14.80) | 0.81 (0.17) | < 0.001 | 67.57 (16.12) | < 0.001 |
| Nephropathy | 777 (10.97) | 0.78 (0.20) | < 0.001 | 66.08 (15.99) | < 0.001 |
| Diabetic foot | 244 (3.45) | 0.71 (0.23) | < 0.001 | 64.32 (16.32) | < 0.001 |
CVD cardiovascular disease
EQ-5D Index by Complications
By examining each complication individually, all the complications had significant impacts on EQ-5D utility (p < 0.001); the EQ-5D utility decrements ranged from 0.15 to 0.29 (Table 3). Although the study population had the lowest prevalence rate of diabetic foot, it had the greatest impact on EQ-5D utility and VAS index. Patients with diabetic foot had the lowest EQ-5D utility of on average 0.71 (SD = 0.23), and the lowest EQ-5D VAS of on average 64.32 (SD = 16.32). The impact was significantly different compared with those patients without diabetic foot (p < 0.000). In contrast, patients with the most prevalent complication, hypertension, had the highest EQ-5D utility of on average 0.85 (SD = 0.17), and the second highest EQ-5D VAS of on average 69.79 (14.64). The impact of hypertension on health utility was significant (p < 0.001). The impact of all the complications was also significant on the self-reported health status among the study population, except for hyperlipidemia (p = 0.2414).
In addition, instead of looking at each specific complication but using the number of complications, EQ-5D health utility and EQ-5D VAS index decreased with additional complications (Fig. 1a, b). Patients with no complications had the highest EQ-5D utility and VAS self-reported health status of on average 0.92 and 73.50, respectively. Patients with additional complications would have lower utility and self-reported health status. For instance, patients with three or more complications had the lowest scores in both the utility and VAS health status of on average 0.79 and 67.21, respectively (Fig. 1a, b).
Fig. 1.
a EQ-5D utility score by number of complications. Average EQ-5D utility score and standard deviation (SD) was classified by number of complications. Mean EQ-5D utility scores are shown at the bottom, SDs are shown at the top of each bar. EQ-5D utility score decreased with increasing number of complications. b EQ-5D VAS score by number of complications. Average EQ-5D VAS score and standard deviation (SD) was classified by number of complications. Mean EQ-5D VAS scores are shown at the bottom, SDs are shown at the top of each bar. EQ-5D VAS score decreased with increasing number of complications
Association Between EQ-5D Index and Complications
Table 4 shows the results from the ordinary least squares (OLS) regression to further describe the association between EQ-5D index and complications, controlling for all sociodemographic characteristics.
Table 4.
OLS regression for EQ-5D index
| Variable | EQ-5D health utility | EQ-5D VAS | ||||
|---|---|---|---|---|---|---|
| Coefficient | Standard error | p | Coefficient | Standard error | p | |
| Age (ref ≤ 45 years old) | ||||||
| 46–59 years old | 0.003 | 0.006 | 0.580 | 0.461 | 0.569 | 0.418 |
| ≥ 60 years old | – 0.034 | 0.006 | < 0.001 | – 0.502 | 0.599 | 0.402 |
| Gender (ref = male) | ||||||
| Female | – 0.016 | 0.003 | < 0.001 | – 0.530 | 0.353 | 0.134 |
| Education level (ref = bachelor degree or higher) | ||||||
| High school | – 0.008 | 0.005 | 0.119 | – 1.470 | 0.496 | 0.003 |
| Middle school or lower | – 0.026 | 0.005 | < 0.001 | – 3.898 | 0.487 | < 0.001 |
| Duration of TD2M (ref ≤ 5 years) | ||||||
| 6–9 years | 0.002 | 0.004 | 0.597 | 0.078 | 0.422 | 0.853 |
| ≥ 10 years | – 0.014 | 0.004 | < 0.001 | – 0.468 | 0.438 | 0.286 |
| Hypertension (ref = no) | ||||||
| Yes | – 0.007 | 0.004 | 0.046 | – 0.567 | 0.363 | 0.119 |
| Cardiovascular disease (ref = no) | ||||||
| Yes | – 0.028 | 0.005 | < 0.001 | – 1.013 | 0.465 | 0.029 |
| Stroke (ref = no) | ||||||
| Yes | – 0.101 | 0.006 | < 0.001 | – 3.340 | 0.567 | < 0.001 |
| Retinopathy (ref = no) | ||||||
| Yes | – 0.022 | 0.005 | < 0.001 | – 2.191 | 0.461 | < 0.001 |
| Nephropathy (ref = no) | ||||||
| Yes | – 0.058 | 0.006 | < 0.001 | – 3.283 | 0.567 | < 0.001 |
| Diabetic foot (ref = no) | ||||||
| Yes | – 0.118 | 0.009 | < 0.001 | – 4.260 | 0.940 | < 0.001 |
| Symptomatic hypoglycemia (ref = 0 event) | ||||||
| Additional event | – 0.007 | 0.002 | < 0.001 | – 0.281 | 0.197 | 0.153 |
| Severe hypoglycemia (ref = 0 event) | ||||||
| Additional event | – 0.008 | 0.004 | 0.049 | – 1.507 | 0.397 | < 0.001 |
In regard to EQ-5D health utility score, duration of type 2 diabetes for 10 years or longer had lower scores by 0.014 compared to those who had been diagnosed with type 2 diabetes for 5 years or less (p < 0.01). Cardiovascular disease, stroke, retinopathy, nephropathy, diabetic foot, and additional symptomatic hypoglycemia events were negatively associated with lower health utility score by 0.007–0.118 (p < 0.001). Hypertension or hyperlipidemia was associated with a decrease in the score, but the association was not significant (p > 0.05).
Most of the complications had similar effects on the EQ-5D VAS score. Diabetic foot was associated with greatest impairment as measured by a VAS reduction of 4.260 points (p < 0.001).
Discussion
To the best of our knowledge, this is the first study that estimates the decrements in health utility caused by complications among Chinese patients with type 2 diabetes and ongoing oral drug treatments. In our study population, the most common complication was hypertension, followed by hyperlipidemia, retinopathy, cardiovascular disease, neuropathy, nephropathy, stroke, and diabetic foot. All complications were negatively associated with the EQ-5D. Diabetic foot reduced the measured EQ-5D utility the most, while hypertension was associated with the greatest reduction in self-reported health status among the study population. Patients with more complications had lower EQ-5D health utility score and VAS score. Age 60 years or older, female sex, middle school or lower education level, and 10 years or longer duration of diagnosis were negatively associated with the EQ-5D health utility score.
Our findings are consistent with previous studies. In the UK, patients with type 2 diabetes and kidney disorders had the greatest decline in health utility, while in Sweden, patients with type 2 diabetes and stroke had the greatest decline in health utility [18]. Hypertension, obesity, and dyslipidemia were found to be highly prevalent among patients with type 2 diabetes receiving oral medications in a cross-sectional study at outpatient clinics in Bangladesh [19]. Other complications were eye problems, followed by chronic kidney diseases and cardiovascular diseases. While in our study we focused on patients with type 2 diabetes and ongoing oral drug treatments in outpatient settings, the highest prevalent complication in our study population was hypertension, followed by hyperlipidemia and cardiovascular disease. Obesity was not included in the questionnaire; thus, we did not evaluate the prevalence of obesity among the population. Zhang et al. [20] also found that major diabetes complications were associated with decreased health-related quality of life in a USA-based observational study of diabetes care in managed care, complications including heart disease, nonpainful diabetic neuropathy, congestive heart failure, and painful neuropathy. Similar findings to those of Zhang et al. were found in a Singapore population, using the 36-item Short Form (SF-36) health survey [21]. Complications such as coronary heart disease, peripheral neuropathy, and severe retinopathy were significantly associated with lower physical component scores. Other complications such as stroke, blindness, and renal failure in our analysis were also found to be negatively associated with health-related quality of life in an Australian study [22].
As shown in Table 4, all the complications had negative impacts on the EQ-5D utility and self-reported health status among the study population. However, when controlled for other variables in the OLS regression (Table 4), the impacts of hypertension and hyperlipidemia were not significant on the EQ-5D utility and the self-reported health status. Furthermore, in our study population, hyperlipidemia was found to be positively associated with the EQ-5D VAS score. One possible reason is that lacking information for durations of the complications may lead to a biased estimator. For example, one study estimating the impact of six diabetes-related complications on quality of life using multiple rounds of EQ-5D questionnaires in diabetic patients in the UK found different short-term and long-term impact of myocardial infarction (MI) on quality of life [23]. Another possible reason is that the interactions between the complications may have an impact on the quality of life, but they were not included in the regression analysis. For example, macrovascular complications, including coronary artery disease, myocardial infarction, stroke, congestive heart failure, and peripheral vascular disease, are well recognized with long-term hypertension. Microvascular complications, such as retinopathy, nephropathy, and neuropathy, are associated with hyperglycemia [24]. In addition, among outpatients with type 2 diabetes, microvascular and macrovascular complications also interact with somatic neuropathy [25]. Future study can consider including these interactions when analyzing the impacts of complications on health utility.
There are some limitations in our study. First, the data we used was extracted from survey questionnaires; self-reported information would introduce information bias and recall bias, especially when it comes to diabetes duration or duration of oral drug treatment. Second, our study population included patients in outpatient settings and it was difficult for patients to adhere to lifestyle management or disease risk management. Because it lacks medication adherence monitoring, it may lead to the development of complications and ineffective diabetes management. Thus, without considering the medication adherence of oral drug treatment among the patients, the estimators may be biased. Third, cardiovascular disease included in the questionnaire was broad, so we could not obtain an in-depth understanding of impacts of specific cardiovascular conditions, such as myocardial infarction, ischemic heart disease, or heart failure, on health utility. Finally, there is a great chance that the selected patients had a more severe condition, such as having more complications or blood pressure that was not well controlled. The estimated impacts of the complications on the health utility may not be representative of those patients with a more stable health condition.
Conclusions
Among patients with type 2 diabetes and ongoing oral drug treatments, complications and comorbidities have significant decrements on health utility scores, especially among those with diabetic foot, stroke, and nephropathy. The disutility from each complication can be used for future economic evaluations among this population.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
YZ analyzed and interpreted the data and wrote the manuscript. JW provided the data that was used for this secondary analysis. YC reviewed the manuscript with substantial edits. LS provided administrative, technical, or logistic support, and supervised the study progress. All authors read and approved the final manuscript. Dr. Wu is a co-corresponding author and data guarantor. She made the same contribution as Dr. Shi.
Prior Presentation
This study was an extension of a previous Chinese study. The previous study was published in Chinese Journal of Endocrinology and Metabolism in 2013 [14]. The previous study has not been presented at any conferences. This present study has been presented as a poster at the International Society of Pharmacoeconomics and Outcomes Research (ISPOR) Annual Conference in 2017.
Disclosures
Yichen Zhang, Jing Wu, Yingyao Chen, and Lizheng Shi have nothing to disclose.
Compliance with Ethics Guidelines
This study used de-identified secondary data from a previous Chinese study. Informed consent was obtained prior to data collection. The previous study and data collection were approved by the Ethics Committee of Peking University People’s Hospital.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to participants’ confidentiality but are available from the corresponding author on reasonable request.
Open Access
This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.11822244.
Contributor Information
Jing Wu, Email: jingwu@tju.edu.cn.
Lizheng Shi, Email: lshi1@tulane.edu.
References
- 1.World Health Organization. Rate of diabetes in China “explosive”. 2018. https://www.who.int/china/news/detail/06-04-2016-rate-of-diabetes-in-china-explosive-#:~:text=. Accessed Dec 2019.
- 2.Mao W, Yip CMW, Chen W. Complications of diabetes in China: health system and economic implications. BMC Public Health. 2019;19(1):269. doi: 10.1186/s12889-019-6569-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan C, Yang W, Jia W, Weng J, Tian H. Management of Chinese patients with type 2 diabetes, 1998–2006: the Diabcare-China surveys. Curr Med Res Opin. 2009;25(1):39–45. doi: 10.1185/03007990802586079. [DOI] [PubMed] [Google Scholar]
- 4.He M, Ma J, Wang D, et al. The disease burden analysis of 295 inpatients with diabetes mellitus from Tongji Hospital in China. Diabetes. 2010;591:A642. [Google Scholar]
- 5.Liu Z, Fu C, Wang W, et al. Prevalence of chronic complications of type 2 diabetes mellitus in outpatients—a cross-sectional hospital-based survey in urban China. Health Qual Life Out. 2010;8(1):62. doi: 10.1186/1477-7525-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Complications. http://www.diabetes.org/living-with-diabetes/complications/. Accessed Dec 2019.
- 7.Yang C, Huang Z, Sun KX, Hu YH, Bao XY. Comparing the economic burden of type 2 diabetes mellitus patients with and without medical insurance: a cross-sectional study in China. Med Sci Monit. 2018;24:3098–3102. doi: 10.12659/MSM.907909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang Y, Vemer P, Zhu J, Postma MJ, Chen W. Economic burden in Chinese patients with diabetes mellitus using electronic insurance claims data. PLoS One. 2016;11(8):e0159297. doi: 10.1371/journal.pone.0159297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Diabetes Federation. IDF Diabetes Atlas, 8th Edition: Country Report-China. 2017 Update. https://reports.instantatlas.com/report/view/704ee0e6475b4af885051bcec15f0e2c/CHN. Accessed 23 Jan 2020.
- 10.Neumann A, Schoffer O, Norstrom F, Norberg M, Klug SJ, Lindholm L. Health-related quality of life for pre-diabetic states and type 2 diabetes mellitus: a cross-sectional study in Vasterbotten Sweden. Health Qual Life Outcomes. 2014;24(12):150. doi: 10.1186/s12955-014-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaidya V, Gangan N, Sheehan J. Impact of cardiovascular complications among patients with type 2 diabetes mellitus: a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2015;15(3):487–497. doi: 10.1586/14737167.2015.1024661. [DOI] [PubMed] [Google Scholar]
- 12.Tan MC, Ng OC, Wong TW, Hejar AR, Anthony J, Sintonen H. The association of cardiovascular disease with impaired health-related quality of life among patients with type 2 diabetes mellitus. Singap Med J. 2014;55(4):209. doi: 10.11622/smedj.2014054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alcubierre N, Rubinat E, Traveset A, et al. A prospective cross-sectional study on quality of life and treatment satisfaction in type 2 diabetic patients with retinopathy without other major late diabetic complications. Health Qual Life Outcomes. 2014;12(1):131. doi: 10.1186/s12955-014-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han YR, Wu J, Cai DH, et al. Evaluation of health-related quality of life in type 2 diabetic patients with various complications and oral drug treatment. Chin J Endocrinol Metab. 2013;19(8):656–659. [Google Scholar]
- 15.Wang HF, Yeh MC. The quality of life of adults with type 2 diabetes in a hospital care clinic in Taiwan. Qual Life Res. 2013;22(3):577–584. doi: 10.1007/s11136-012-0178-7. [DOI] [PubMed] [Google Scholar]
- 16.Bakker C. Health related utility measurement: an introduction. J Rheumatol. 1995;22(6):1197–1199. [PubMed] [Google Scholar]
- 17.Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12:S5–S9. doi: 10.1111/j.1524-4733.2009.00515.x. [DOI] [PubMed] [Google Scholar]
- 18.Kiadaliri A, Gerdtham UG, Eliasson B, Gudbjörnsdottir S, Svensson AM, Carlsson K. Health utilities of type 2 diabetes-related complications: a cross-sectional study in Sweden. Int J Environ Res Public Health. 2014;11(5):4939–4952. doi: 10.3390/ijerph110504939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam SM, Alam DS, Wahiduzzaman M, et al. Clinical characteristics and complications of patients with type 2 diabetes attending an urban hospital in Bangladesh. Diabetes Metab Syndr. 2015;9(1):7–13. doi: 10.1016/j.dsx.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 20.Zhang P, Brown MB, Bilik D, Ackermann RT, Li R, Herman WH. Health utility scores for people with type 2 diabetes in US managed care health plans: results from Translating Research Into Action for Diabetes (TRIAD) Diabetes Care. 2012;35(11):2250–2256. doi: 10.2337/dc11-2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Venkataraman K, Wee HL, Leow MKS, et al. Associations between complications and health-related quality of life in individuals with diabetes. Clin Endocrinol. 2013;78(6):865–873. doi: 10.1111/j.1365-2265.2012.04480.x. [DOI] [PubMed] [Google Scholar]
- 22.Hayes A, Arima H, Woodward M, et al. Changes in quality of life associated with complications of diabetes: results from the ADVANCE study. Value Health. 2016;19(1):36–41. doi: 10.1016/j.jval.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 23.Alva M, Gray A, Mihaylova B, Clarke P. The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ. 2014;23(4):487–500. doi: 10.1002/hec.2930. [DOI] [PubMed] [Google Scholar]
- 24.Long AN, Dagogo-Jack S. Comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J Clin Hypertens. 2011;13(4):244–251. doi: 10.1111/j.1751-7176.2011.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salvotelli L, Stoico V, Perrone F, et al. Prevalence of neuropathy in type 2 diabetic patients and its association with other diabetes complications: The Verona Diabetic Foot Screening Program. J Diabetes Complicat. 2015;29(8):1066–1070. doi: 10.1016/j.jdiacomp.2015.06.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to participants’ confidentiality but are available from the corresponding author on reasonable request.