Abstract
Background: Major depressive disorder (MDD) is the most common psychological disorder and affects many people worldwide. Surveying the prevalence of mental disorders, especially general disorders, such as major depressive disorder, is highly important for health professionals and policymakers. Due to a wide variation of studies concerning the prevalence of major depressive disorder in Iran, the present study was conducted to integrate such results.
Methods: To conduct this study, English (PubMed/Medline, Scopus and Web of Science) and Persian (MHRN, Noormgs, Magiran, Iran-Medex, Irandoc, and SID) databases, from 1990 to 2018, were explored. All articles related to the point prevalence of depressive disorders in the general population of Iran were reviewed. The inclusion criteria of the present study were as follow: cross sectional studies based on general populations; the expression of the point prevalence rate and incidence of major depressive disorder for people over 15 years; and the use of a structured or semi-structured clinical interview for diagnosis of the disorder. Studies that were not original (such as review studies) and those that did not represent general populations were excluded from the study. To analyze the data obtained from this study, the second version of Comprehensive Meta-Analysis (CMA) software was used. The total point prevalence was calculated using the meta-analysis method, and the I2 index was used to measure the heterogeneity of the studies.
Results: Of 6734 studies, 30 studies with a total sample size of 37 867 were finally included based on proposed inclusion and exclusion criteria. The sample included 20641 women (55%), and 17 226 (45%) men. In the present meta-analysis study, due to significant heterogeneity (I=97.1%, p=0.001) among studies, the randomized method was used, and the total point prevalence was 4.1% (CI: 3.1% 5.5%). The overall point prevalence of major depressive disorder was 4.8% (CI: 3.6% -5.6%) in women and 2.3% (CI: 1.6% -3.6%)in men, which indicated that the incidence of this disorder was 1.95 times more in women than in men.
Conclusion: This meta-analysis study found a considerable prevalence of major depressive disorder among Iranian participants and revealed that the point prevalence of the disease was more than two-fold in women compared to men. Considering these findings and the high burden of this disorder for communities, the need to formulate and implement prevention and treatment programs is highly required.
Keywords: Prevalence, Major depressive disorder, Iran, Meta-analysis, Systematic review
↑ What is “already known” in this topic:
Depression has an important role in people’s lives. Many studies have investigated the prevalence of depressive disorders in Iran during past decades.
→ What this article adds:
This systematic review and meta-analysis revealed the considerable prevalence of major depression disorder among Iranians.
Introduction
Major depressive disorder is the most common psychological disorder in the world and affects many people. This disorder causes several problems in professional life, social relationships, and the personal lives of individuals. About 350 million people are depressed worldwide (1); this number rised by about 18% between 2005 and 2015. According to the World Health Organization forecasts by 2020, this disorder will be in the second position in the list of the burden of disease. About 800 000 people die annually because of suicidal ideation due to this disorder (2, 3). The main symptoms of major depressive disorder include lack of positive emotions and lack of interest and pleasure, which accompany other symptoms such as sleeping problems, feelings of self-worthlessness, and thoughts of suicide and death. To diagnose this disorder, the symptoms listed in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) must be present on most days during the least 2 weeks (4).
The prevalence of major depressive disorder is affected by many factors such as culture, socioeconomic status, age, gender, marital status, physical health status, occupation, and other factors (5-7). A recent systematic review on the prevalence of major depressive disorder and its effective factors in 30 different countries showed that major depressive disorder has a point prevalence of 12.9%, the one-year prevalence of 7.2%, and a lifetime prevalence of 10.8%. The point prevalence of major depressive disorder was significantly higher in women (14.4%) and countries with moderate levels of human development index, including many Asian countries, had a higher prevalence of major depressive disorder (29.2%) (8).
Iran is one of the largest countries in western Asia with a population of more than 81 million, with diverse cultures. Fars, Kurds, Turks, Baluch, Turkmen, and Arabs live in Iran (9), and this cultural diversity affects the prevalence of depressive disorders (10). The results of a systematic review of the prevalence of major depressive disorder in Iran in 2010 showed that the point prevalence of major depressive disorder in Iran was 4.1% and the incidence of women with this disorder was 1.95 times more than that of men. The point prevalence of this disorder was not significantly different in urban and rural areas (10).
The prevalence of mental disorders, especially common disorders such as major depressive disorder, is significant for health professionals and policymakers and can help reduce social discrimination in the area of receiving health services (11). Many studies have been conducted on the prevalence of these disorders in many countries; and to make the information obtained from these studies understandable, there is a need to integrate their results in the form of systematic review (12). Many studies have been conducted in Iran on the prevalence of major depressive disorder. However, due to their wide variety in the population studied, measurement tools used, study years, and many other factors, there is a severe need to integrate their results for a better understanding. Therefore, the present study aimed to investigate all studies that had been conducted in Iran from 1990 to 2018 that examined the point prevalence of major depressive disorder in Iran to integrate the prevalence rates of these studies and to determine the overall point prevalence of major depressive disorder disorder in Iran.
Methods
This study was conducted according to the systematic and meta-analytic review (PRISMA) reporting guide (13). Before conducting this study, its protocol, including method of searching, inclusion criteria, method of extracting information, etc., was designed and published (14).
Information resources
For this study, the Institute of Scientific Information (ISI), PubMed, and NLM Gateway (for MEDLINE), and SCOPUS databases were selected as the primary sources of international electronic information. The Scientific Information Database (SID), Iran-Medex, Irandoc, MHRN, Noormgs, and Magiran databases were also investigated to access national information sources. According to the objectives of this study, all sources were studied from January 1990 through January 2018 without any restrictions on the language of the studies. The researchers also tried to search unpublished sources and reports using a manual search, and if necessary, communicate with the author to obtain the required information.
Search strategy and eligibility criteria
Searches on all databases were done by 2 researchers independently to increase search accuracy. Search strategy in international sources was designed in 3 steps, based on the Medical Subject Headings (MeSH) and other keywords, and the results of the third step were examined. The 3 steps of the search and the words used were as follow:
Step I- “"depressive disorder*" OR "mood disorder*" OR "affective disorder*" OR "depression*" OR "depressive symptom*" OR "depression symptom*" OR "emotional depression*" OR "emotional disorder*"”.
Step II- “Iran* OR Persia* OR I.R.Iran* OR IR.Iran*”.
Step III- step I AND step II.
To search the national databases, the mentioned English keywords, as well as their Persian equivalents, were used to search all sources, such as published articles, summaries of conferences, issues, and reports. Since many of the national databases were restricted by the use of search strategies, keywords were searched separately.
The inclusion criteria of the present study included cross-sectional studies based on the general populations, the expression of the point prevalence rate and incidence of major depressive disorder for people over 15 years, and the use of a structured or semi-structured clinical interview for diagnosis of the disorder (DSM-III-based clinical interview, DSM-IV-based clinical interview, Schedule for Affective Disorders and Schizophrenia, Structured Clinical Interview for DSM-IV Axis I Disorders, and Composite International Diagnostic Interview). Studies that were not original (such as review studies) and those that did not represent general populations, including studies that focused on the major depressive disorder of certain specific patients (eg, cancer, diabetes, etc.), those with special occupations (eg, workers of a particular factory), pregnant women or those who just had a baby, women during their menstruation, prisoners, and hospitalized patients were excluded from the study.
Selection of studies and data extraction
Two researchers independently studied the results of the initial search based on studies’ titles and abstracts and selected those that met the inclusion criteria. At this stage, duplicate studies were omitted, and in cases where the 2 researchers disagreed about a study, the disagreement was resolved based on the compromise or discussion or opinion of the third researcher. The same 2 researchers independently extracted information and completed standard forms designed for this purpose, which included information about the study characteristics such as title, first author, year of implementation and publication, location of deployment, sampling method, sample size, measurement tools, point prevalence, standard error, and confidence interval.
Quality assessment
To assess the quality of the selected articles, the tool presented in the study of Ibrahim et al was used (15). In this tool, 7 items are used for scoring the quality of the articles, and the total score of the sum of the scores for these 7 items is obtained; the items are as follow: (1) the target population is clearly defined; (2) complete, random, or consecutive sampling; (3) the targeted sample is representative, or there is evidence showing that the results can be generalized to the general population (4); the response rate is equal to or greater than 70%; (5) the instrument used to diagnose major depressive disorder is a valid tool; (6) the sample size is at least 300 individuals; (7) the confidence interval or standard error are reported. For each of these items, a score was assigned to each relevant study. For example, an article that has all of the above items but does not specify the confidence interval or standard error receives a maximum of 6 points. Two researchers independently evaluated the quality of the selected articles, and in cases where they differed, the difference was resolved by compromise or the opinion of the third researcher.
Statistical analysis
To analyze the data obtained from this research, the second version of the Comprehensive Meta-Analysis software (CMA) (16) was used. The pooled point prevalence was calculated using the meta-analysis method, and the I2 index was used to measure the heterogeneity between the studies. Whenever this index was higher than 0.50, the random model was used instead of the fixed model in the meta-analysis (17). Considering that based on the inclusion and exclusion criteria, there was no significant heterogeneity in the diagnostic tools and the age of the sample between the studies, and also considering the limitation in the detailed information of each study (such as lack of the prevalence in rural and urban areas separately in each study), the subgroup analysis was conducted solely based on gender. The bias of publication was evaluated by a funnel plot as well as Begg’s correction test. Significance level was set at p<0.05.
Results
Study selection
Of the 6734 studies found in the search of the databases, 1076 were duplicates and excluded and 4950 were also excluded at the initial screening stage. Finally, 30 papers with a total sample size of 37 867 were selected based on inclusion and exclusion criteria. Moreover, a national study with a sample size of 25180 was excluded because its information was published in the form of several other articles separated by different provinces. Details of the process of selecting studies are reported in Figure 1.
Fig. 1.
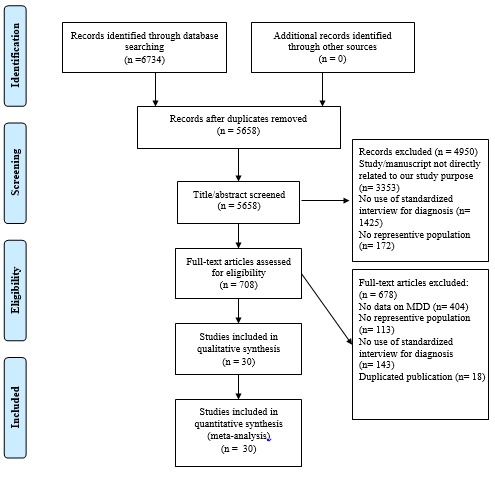
PRISMA flow diagram showing study selection process
Studies characteristics
All studies have been conducted from 1995 to 2015 in 18 different provinces of Iran, along with a national survey. The sample size of these studies was between 204 and 7886 people, of whom 20 641 (55%) were women and 17 226 (45%) were men. The minimum age of the sample in these studies was 15 years. At a 7-degree scale, the quality of the studies selected was between 4 and 7, with a mean of 5.06. Of the 30 final studies, 20 included both urban and rural areas, while 6 were limited to urban areas, and only one study was limited to rural areas. Among the studies reviewed, one study was related to high school students and 2 to university students. All studies had used clinical interview and measurement tools by blended methods to increase the accuracy of diagnosis. The tools used in the studies included DSM-III-based clinical interview, DSM-IV-based clinical interview, General Health Questionnaire (GHQ), Self-Reporting Questionnaire (SRQ-24), Symptom Checklist-90 Revised (SCL-90-R), Beck Depression Inventory (BDI), Schedule for Affective Disorders and Schizophrenia (SADS), Geriatric Depression Scale (GDS), Composite International Diagnostic Interview (CIDI), and Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). The details of the characteristics of the studies selected are summarized in Table 1.
Table 1. Characteristics of the included studies .
|
First author (reference) |
Year of publication | Province | Sample size | Female gender (%) | Age (years) | Population type | Sampling method | Diagnostic tools | Point prevalence (%) |
95% Confidence interval (CI) |
Quality score |
| Yaghoubi et al. (18) | 1995 | Guilan | 625 | 53.4 | ≥15 | Urban & Rural | Cluster random | GHQ & DSM-III based clinical interview | 6.2 | 4.6-8.4 | 5 |
| Sadeghi et al. (19) | 2000 | Kermanshah | 501 | 53.9 | ≥15 | Urban | Cluster random | SRQ-24 & DSM-IV based clinical interview | 1.6 | 0.7-3.5 | 5 |
|
Shamsalizadeh et al. (20) |
2001 | Tehran | 640 | 55.1 | ≥15 | Rural | Total population | GHQ & DSM-IV based clinical interview | 11.3 | 9.1-14.0 | 5 |
|
Khosravi (21) |
2002 | Chaharmahal and Bakhtiari | 450 | 57.7 | ≥15 | Urban & Rural | Systematic random | SCL-90-R & DSM-III based clinical interview | 4.7 | 3.1-7.0 | 5 |
| Kaviani et al. (22) | 2002 | Tehran | 1052 | 49.0 | 20-65 | Urban | Cluster random | BDI & DSM-IV based clinical interview | 6.8 | 5.4-8.5 | 5 |
|
Mohammadi et al. (23) |
2003 | Mazandaran | 1022 | 51.7 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 4.6 | 3.5-6.1 | 5 |
| Mohammadi et al. b (24) | 2003 | West Azerbaijan | 1041 | 50.1 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 4.6 | 3.5-6.1 | 5 |
| Hassanshahi et al. (25) | 2003 | Fars | 650 | 57.8 | ≥15 | Urban & Rural | Simple random | SCL-90-R & DSM-IV based clinical interview checklist | 7.2 | 5.5-9.5 | 5 |
| Omidi et al. (26) | 2003 | Isfahan | 650 | 50.0 | ≥15 | Urban | Systematic random | GHQ & DSM-IV based clinical interview checklist | 3.4 | 2.3-5.1 | 5 |
| Mohammadi et al. c (27) | 2003 | Kurdistan | 495 | 49.3 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 4.0 | 2.6-6.2 | 5 |
| Mohammadi et al. d (28) | 2003 | Kohgiluyeh and Boyer Ahmad | 337 | 49.2 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 0.3 | 0-2.1 | 5 |
| Mohammadi et al. e (29) | 2003 | Semnan | 280 | 53.2 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 3.6 | 1.9-6.5 | 4 |
| Mohammadi et al. f (30) | 2003 | Tehran | 5311 | 48.5 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 3.3 | 2.8-3.8 | 5 |
|
Mohammadi et al. (31) |
2004 | Guilan | 925 | 50.8 | ≥15 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 3.0 | 2.1-4.4 | 5 |
| Mohammadi et al. b (32) | 2004 | East Azerbaijan | 1286 | 49.1 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 2.3 | 1.6-3.2 | 5 |
| Mohammadi et al. c (33) | 2004 | Hamadan | 664 | 48.2 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 2.6 | 1.6-4.1 | 5 |
| Mohammadi et al. d (34) | 2004 | Chaharmahal and Bakhtiari | 305 | 47.5 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 2.3 | 1.1-4.7 | 5 |
| Mohammadi et al. e (35) | 2004 | Ardebil | 394 | 47.5 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 4.8 | 3.1-7.4 | 5 |
| Mohammadi et al. f (36) | 2004 | Golestan | 518 | 47.9 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 1.9 | 1.0-3.5 | 5 |
| Mohammadi et al. g (37) | 2004 | South Khorasan | 2301 | 50.4 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 2.3 | 1.7-3.0 | 5 |
|
Mohammadi et al. (38) |
2005 | Kerman | 876 | 51.3 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 5.6 | 4.2-7.3 | 5 |
| Mohammadi et al. b (39) | 2005 | Qazvin | 354 | 50.8 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 2.8 | 1.5-6.2 | 5 |
|
Hosseinifard et al. (40) |
2005 | Kerman | 830 | 54.5 | 15-18 | High-school Students | Multistage | SCL-90-R & DSM-IV based clinical interview checklist | 2.4 | 1.6-3.7 | 5 |
| Parvizifard et al. (41) | 2006 | Kermanshah | 423 | 74.2 | 17-22 | University Students | convenience | SRQ-24 & DSM-IV based clinical interview checklist | 5.7 | 3.8-8.3 | 5 |
|
Modabernia et al. (42) |
2008 | Guilan | 4020 | 62.8 | 18-70 | Urban & Rural | Multistage cluster random | BDI & DSM-IV based clinical interview | 1.0 | 0.7-1.4 | 6 |
|
Mirabzadeh et al. (43) |
2009 | Tehran | 204 | 53.4 | ≥59 | Urban | Simple random | GHQ & GDS & CIDI | 10.7 | 15.4-26.5 | 4 |
| Parvaresh et al. (44) | 2010 | Kerman | 1527 | 67.6 | ≥15 | Urban | Cluster random | GHQ & DSM-IV based clinical interview | 6.8 | 5.7-8.2 | 6 |
|
Ahmadvand et al. (45) |
2012 | Isfahan | 1800 | 54.5 | ≥18 | Urban | Stratified random | GHQ & DSM-IV based clinical interview checklist | 8.2 | 7.0-9.6 | 5 |
| Yaghubi et al. (46) | 2014 | Tehran | 500 | 62.0 | NR | University Students | Quota Sampling | GHQ & CIDI | 8.5 | 6.4-11.3 | 5 |
| Sharifi et al. (47) | 2015 | National | 7886 | 57.0 | 15-64 | Urban & Rural | Multistage cluster random | CIDI & SCID-I | 12.7 | 12.0-13.5 | 7 |
|
Mohammadi et al. (48) |
2001 | National | 25180 | 49.7 | ≥18 | Urban & Rural | Multistage cluster random | SADS & DSM-IV based clinical interview | 1.8 | 1.0-2.9 | 5 |
Pooled point prevalence
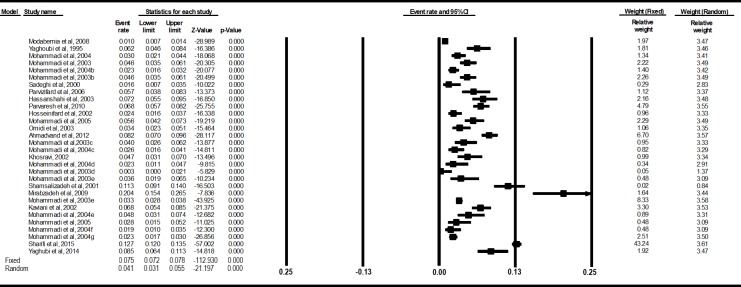
Studies that entered the final analysis showed that the point prevalence of major depressive disorder was between 0.3% and 12.7%. To calculate the point prevalence of the 30 final studies entered in this study, based on the evidence of significant heterogeneity (I2=97.1%, p=0.001), a randomized model was used in meta-analysis, based on which the pooled point prevalence was obtained equal to 4.1% (CI: 3.1-5.5%) (Fig. 2). The lowest point prevalence belonged to a study in Kohgiluyeh and Boyer Ahmad, with 0.3%, and the highest point prevalence to a national survey, with a major depressive disorder prevalence of 12.7%. The spatial distribution of major depressive disorder point prevalence is shown in Figure 3.
Fig. 2.
Forest plot of major depressive disorder point prevalences in the included studies
Fig. 3.
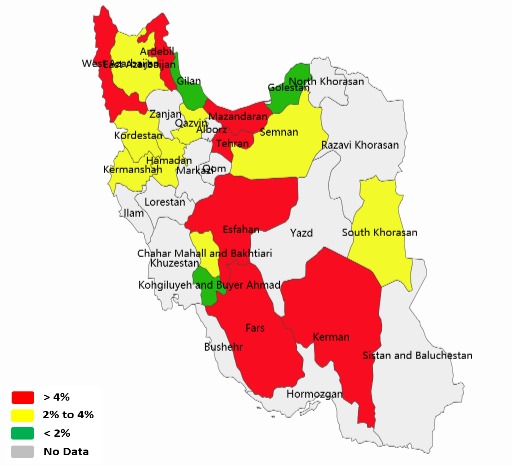
Spatial distribution of point prevalence of major depressive disorder in Iran
Publication bias
To measure the publication bias, the funnel plot and the Begg’s Correction Index were used. The funnel plot indicated no bias in the publication, which was also confirmed by the Begg’s Correction Index (p=0.134) (Fig. 4).
Fig. 4.
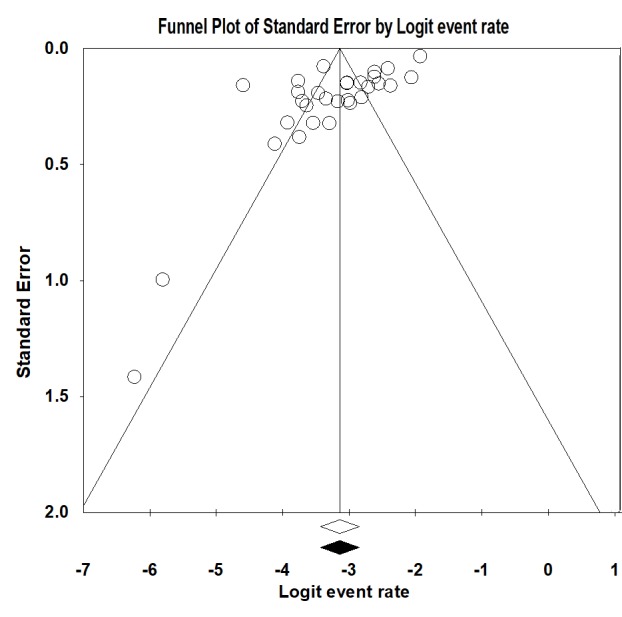
Funnel plot of the studies assessing the point prevalence of major depressive disorder
Analysis of subgroups
As discussed earlier, in the present study, the analysis of subgroups was performed solely based on gender. Accordingly, the total point prevalence of major depressive disorder was 4.8% (CI: 3.5-6.6%) in women and 2.3% in men (CI: 1.6-3.6%), which indicated the risk of this disorder was twice in women than in men.
Discussion
A study on the prevalence of mental disorders, especially common disorders such as major depressive disorder, which imposes a high burden on communities and can endanger the lives of many people (49), has a vital role in the formulation and development of prevention and treatment programs for mental health professionals (50). In recent years, many studies have been conducted on the prevalence of major depressive disorder in Iran and the dispersion of these studies required the implementation of a systematic and meta-analysis study. This study conducted a systematic review and meta-analysis of the studies conducted on the prevalence of major depressive disorder in Iran from 1990 to 2018. Also, through the precise and almost strict inclusion and exclusion criteria, this study aimed to select those papers that use accurate methods for diagnosing major depressive disorder and whose samples represented the general population.
The results of this study revealed a 4.1% point prevalence of major depressive disorder in Iran, where women, with a 4.8% probability, were exposed to risk twice as men, with a 2.3% probability. These results indicated that the point prevalence obtained in this study was slightly lower than that of the World Health Organization (WHO) in 2015 (4.9%), whose cause may be the much larger sample of the study by World Health Organization (51). According to the results of this study, the point prevalence of major depressive disorder in Iran among Asian countries is similar to Bangladesh (4.1%) and Sri Lanka (4.1%) and has lower statistics than countries such as Qatar (5.1%), United Arab Emirates (5.1%), Lebanon (4.7%), Oman (4.7%), India (4.5%) and Thailand (4.4%). Also, Iran is more vulnerable than many other countries such as Indonesia (3.7%), North Korea (3.7%), Maldives (3.7%), Yemen (6.3%), and Nepal (2.3%) (52).
The results of this study are also consistent with the Systematic Review of Sadeghirad et al (2010) (10), both of which representing a 4.1% point prevalence of major depressive disorder in Iran. The results of the present study showed that the incidence in women was slightly higher than that of men, which is in line with findings of many previous studies (8, 12, 53). This gender difference in major depressive disorder is highlighted in psychiatric literature, and some of its reasons can be attributed to psychological characteristics, biological differences, and gender roles (54, 55). The point prevalence of major depressive disorder in this study was more than twice the reported point prevalence of 1.8% in the 2001 National Research (56). This difference may be due to several reasons. First, because of the intervals of more than 17 years between the 2 studies, the possibility of an increase in the prevalence of major depressive disorder in Iran was not far from impossible, as the prevalence of major depressive disorder in many countries has increased in recent years (2, 52). Second, the tool used in the 2001 National Research (SADS) was different from many of the studies used in the present study, which can be one of the reasons for the difference in the disorder prevalence rates. Also, the number of sample of the 2 studies was different, which could be one of the reasons for the change in the reported prevalence rates.
Since many studies were from different regions of the country, it was not possible to compare the prevalence of the disease in different years. However, a comparison of the results of the 2 national studies in 2001 (48) and 2015 (47) showed a significant increase in the prevalence of depression from 1.8 to 12.7. Altough it is recommended that further studies should be designed to find the possible causes of this increase, changing trends in sociological and economic issues can have effective roles in this increase.
Limitation
This study has some limitations that are to be considered. First, despite the high efforts of the researchers, some unpublished studies were inevitably omitted due to lack of access to their information. Second, due to the lack of reporting detailed information by many pieces of research, subgroup analysis was conducted solely based on gender, and no comparison was made between rural and urban areas, educational levels, and different social and economic levels. Finally, the failure to use multivariate analysis to control the moderating variables in the present study can affect the reported prevalence.
Conclusion
The current meta-analysis revealed a noticeable point prevalence of major depressive disorder in Iran, which was twice more in women than in men. Considering this information and the high cost of this disorder for communities, the need to formulate and implement preventive and treatment programs is felt more than ever. Also, no precise study has been conducted in many provinces of the country, and thus the prevalence rate of major depressive disorder is unclear in those areas, which can create problems for the health system in the future.
Acknowledgments
The authors appreciate Batul Taefi and Maziar Moradi Lakeh for their valuable comments on this project.
Funding
This study was granted by the Mental Health Research Center of Iran University of Medical Sciences, Tehran, Iran.
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Gharraee B, Zahedi Tajrishi K, Sheybani F, Tahmasbi N, Mirzaei M, Farahani H, Naserbakht M. Prevalence of major depressive disorder in the general population of Iran: A systematic review and meta-analysis. Med J Islam Repub Iran. 2019 (25 Dec);33:151. https://doi.org/10.34171/mjiri.33.151
References
- 1.Summergrad P. Investing in global mental health: the time for action is now. Lancet Psychiat. 2016;3(5):390–91. doi: 10.1016/S2215-0366(16)30031-1. [DOI] [PubMed] [Google Scholar]
- 2. World-Health-Organization. Depression. 2017.
- 3. World-Health-Organization. Depression. 2015.
- 4. Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013. [DOI] [PubMed]
- 5.Pramesona B, Taneepanichskul S. Prevalence and risk factors of depression among Indonesian elderly: A nursing home-based cross-sectional study. Neurol Psychiat Br. 2018;30:22–7. [Google Scholar]
- 6.Kugbey N, Nortu TA, Akpalu B, Ayanore MA, Zotor FB. Prevalence of geriatric depression in a community sample in Ghana: Analysis of associated risk and protective factors. Arch Gerontol Geriatr. 2018;78:171–6. doi: 10.1016/j.archger.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 7.Tuithof M, ten Have M, van Dorsselaer S, Kleinjan M, Beekman A, de Graaf R. Course of subthreshold depression into a depressive disorder and its risk factors. J Affect Disord. 2018;241:206–15. doi: 10.1016/j.jad.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci Rep. 2018;8(1):2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vatanka A. The Authoritarian Resurgence: Iran Abroad. J Democr. 2015;25:63. [Google Scholar]
- 10.Sadeghirad B, Haghdoost AA, Amin-Esmaeili M, Ananloo ES, Ghaeli P, Rahimi-Movaghar A. et al. Epidemiology of major depressive disorder in Iran: a systematic review and meta-analysis. J Prev Med. 2010;1(2):81. [PMC free article] [PubMed] [Google Scholar]
- 11.Rondet C, Cornet P, Kaoutar B, Lebas J, Chauvin P. Depression prevalence and primary care among vulnerable patients at a free outpatient clinic in Paris, France, in 2010: results of a cross-sectional survey. BMC Fam Pract. 2013;14(1):151. doi: 10.1186/1471-2296-14-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Bromet EJ. The epidemiology of depression across cultures Annu. Rev Public Health. 2013;34:119–38. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naserbakht M, Djalalinia S, Tayefi B, Gholami M, Ardabili ME, Shariat SV. et al. National and sub-national prevalence, trend, and burden of mental disorders and substance abuse in Iran: 1990-2013, study protocol. Arch Iran Med. 2014;17(3):182–8. [PubMed] [Google Scholar]
- 15.Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yaghoubi N, Nasr M. Shahmohammadi Epidemiology of mental disorders in urban and rural areas of Sowmaesara Gilan. Andisheh va Rafter. 1995;2:55–65. [Google Scholar]
- 19.Sadeghi K, Saberi M, Osareh M. Epidemiology of mental illness in the urban population of Kermanshah. Iran J Psychiatry Clin Psychol. 2000;6(22-23):16–25. [Google Scholar]
- 20.Shamsalizadeh N, Boualhari J, Shahmohammadi D. Epidemiology Of Mental Disorders In A Village In Tehran Province. Iran J Psychiatry Clin Psychol. 2001;7(1-2):19–26. [Google Scholar]
- 21.Khosravi S. The study of epidemiology of mental disorder among the population above 15 years of urban and rural of Brojen town. J Shahrekord Univ Med Sci. 2002;4(4):31–9. [Google Scholar]
- 22.Kaviani H, As AA, Nazari H, Hormozi K. Prevalence of depressive disordrs in Tehran resident population (year 2000) Tehran Uni Med J. 2002;60(5):393–9. [Google Scholar]
- 23.Mohammadi M, Rahgozar M, Mesgarpour B, Barimani F, Taheri S, Malekzadeh S. An epidemiological study of psychiatric disorders in mazandaran province Year 2001. J Mazandaran Uni Med Sci. 2003;13(41):8–19. [Google Scholar]
- 24.Mohammadi M, Rahgozar M, Bagheri Yazdi S, Mesgarpour B, Dadras M, Gharibkhani H. et al. An epidemiological study of psychiatric disorders in west Azerbaijan province (year 2001) J Mazandaran Uni Med Sci. 2003;13(41) [Google Scholar]
- 25.Hassanshahi M, Goodarzi M, Mirjafari S, Farnam R. Prevalence of Psychiatric Disorders in the city of Arsanjan. The Quarterly Journal of Fundamentals of Mental Health. 2003;2004(5):19–20. [Google Scholar]
- 26.Omidi A, Tabatabai A, Sazvar S, Akkashe G. Epidemiology of mental disorders in urbanized areas of Natanz. Iran J Psychiatry Clin Psychol. 2003;8(4):32–8. [Google Scholar]
- 27.Mohammadi M, Bagheri Yazdi S, Rahgozar M, Mesgarpour B, Saram N, Shabrang M. et al. The Epidemiological Study of Psychiatric Disorders in Kurdistan Province. Sci J Kurdistan Uni Med Sci. 2003;7(3):9–19. [Google Scholar]
- 28.Mohamadi M, Rahgozar M, Msgarpour B, Nazari M. An Epidemiological Study of Psychiatric Disorders in Kohgilouie & BoyerAhmad Province (Year 2001) Armaghane danesh. 2003;8(2):10–24. [Google Scholar]
- 29.Mohammadi M, Bagheri Yazdi S, Rahgozar M, Mesgarpour B, Behnam B, Imani E. et al. An epidemiological study of psychiatric disorders in Semnan province in the year 2001. Shiraz Uni Med Sci. 2003;5(1):7–17. [Google Scholar]
- 30.Mohammadi M, Rahgozar M, Bagheri Yazdi A, Naghavi H, Pour Etemad HR, Amini H. et al. Epidemiological study of psychiatric disorders in Tehran province. Iran J Psychiatry Clin Psychol. 2003;9(2):4–13. [Google Scholar]
- 31.Mohammadi M, Rahgozar M, Bagheri Yazdi S, Mesgarpour B, Khalkhali M, Farsi M. et al. An epidemiological study of psychiatric disorders in Guilan province (year 2001) J Guilan Univ Med Sci. 2004;13(51):1–13. [Google Scholar]
- 32.Mohammadi M, Bagheri Yazdi A, Rahgozar M, Mesgarpour B, Kokabeh F, Gharehdaghi K. et al. An Epidemiological Study of Psychiatric Disorders in East Azerbaijan Province (Year 2001) Med J Tabriz Uni. 2004;38(64):67–73. [Google Scholar]
- 33.Mohammadi M, Bagheri Yazdi A, Rahgozar M, Mesgarpour B, Babalhavaegi A, Lotfi A. et al. An epidemiological study of psychiatric disorders in Hamadan province, 2001. Sci J Hamdan Uni Med Sci. 2004;3(33):28–36. [Google Scholar]
- 34.Mohamadi M, Rahgozar M, Bagheri Yazdi A, Mesgarpour B, Nikfarjam M, Raeisi M. An epidemiological study of psychological disorders in chaharmahal & bakhtiari province, 2001. J Shahrekord Uni Med Sci. 2005;6(4):33–42. [Google Scholar]
- 35.Mohamadi M, Rahgozar M, Bagheri Yazdi A, Mesgarpour B, Niktash J, Davarnia B. et al. An epidemiological study of psychiatric disorders in Ardebil province. Urmia Med J. 2004;3(57):174–83. [Google Scholar]
- 36.Mohammadi M, Rahgozar M, Mesgarpour B, Hosseini S, Safari Z, Moumeni F. An epidemiological study of psychiatric disorders in Golestan province (Year 2001) J Gorgan Uni Med Sci. 2004;6(13):67–77. [Google Scholar]
- 37.Mohammadi M, Bagheri Yazdi A, Rahgozar M, Mesgarpour B, Rezayi Ansari A, Haghdadi G. et al. Epidemiological study of psychiatric disorders in Khorasan province in 2001. J Sabzevar Uni Med Sci. 2004;11(1):6–17. [Google Scholar]
- 38.Mohamadi B, Bagheri Yazdi A, Rahgozar M, Mesgarpour B, Hosseini Fakhr G, Bargasteh H. et al. An epidemiological study of psychiatric disorders in Kerman province in the year 2001. The J Rafsanjan Uni Med Sci. 2005;4(3):136–45. [Google Scholar]
- 39.Mohammadi M, Bagheri Yazdi A, Rahgozar M, Mesgarpour B, Roshanpajoh M, Bagheri Tabrizi A. An epidemiological study of psychiatric disorders in Qazvin province (2001) J Qazvin Uni Med Sci. 2005;8(33):36–44. [Google Scholar]
- 40.Hosseinifard S, Birashk B, Atefvahid M. Epidemiology of mental disorders in high-school students in Rafsanjan. Iran J Psychiatry Clin Psychol. 2005;11(1):71–80. [Google Scholar]
- 41.Parvizifard AA, Shakeri J, Sadeqhi K, Ameri MR, Nezhadjafar P. Psychiatric disorders in first year students of Kermanshah University of medical sciences (2002) J Kermanshah Uni Med Sci. 2006;10(2):120–9. [Google Scholar]
- 42.Modabernia MJ, Tehrani HS, Fallahi M, Shirazi M, Modabbernia AH. Prevalence of depressive disorders in Rasht, Iran: A community based study. Clinical practice & epidemiology in mental health. 2008;4(1):20–6. doi: 10.1186/1745-0179-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mirab Zadeh A, Malakooti SK. Regional Demographical and Epidemiological Survey of Some Geriatricpsychiatric Disorders in Ekbatan District of Tehran. J Kerman Uni Med Sci. 2009;4(3):56–66. [Google Scholar]
- 44.Parvaresh N, Ziaaddini H, Nakhei N, Nahid A, Safavi H, Sajadi B. The Frequency of Mental Disorders among Kerman Residents above 15 Years of Age. J Kerman Uni Med Sci. 2014;18(4):291–300. [Google Scholar]
- 45.Ahmadvand A, Sepehrmanesh Z, Ghoreishi FS, Afshinmajd S. Prevalence of psychiatric disorders in the general population of Kashan, Iran. Arch Iran Med. 2012;15(4):205–9. [PubMed] [Google Scholar]
- 46.Yaghubi H, Karimi M, Omidi A, Mesbah N, Kahani Sh A-Q-QM. Prevalence of mental disorders and demographic factors that influence the freshmen students of Tehran City Universities of Medical Sciences. J Clin Psychol. 2014;6(2):95–104. [Google Scholar]
- 47.Vandad Sharifi M, Hajebi A, Radgoodarzi R. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med. 2015;18(2):76–84. [PubMed] [Google Scholar]
- 48.Mohammadi M, Davidian H, Nourbala A, Malek Afzali H, Naghavi H, Pouretemad HR. et al. An epidemiological study of psychiatric disorders in Iran, 2001. Hakim Res J. 2003;6(1):55–65. [Google Scholar]
- 49.Ahmed HU, Hossain MD, Aftab A, Soron TR, Alam MT, Chowdhury MWA. et al. Suicide and depression in the World Health Organization South-East Asia region: A systematic review. WHO South-East Asia journal of public health. 2017;6(1):60. doi: 10.4103/2224-3151.206167. [DOI] [PubMed] [Google Scholar]
- 50.Wang J, Wu X, Lai W, Long E, Zhang X, Li W. et al. Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ. 2017;7(8):e017173. doi: 10.1136/bmjopen-2017-017173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053):1545–602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. World Health Organization (WHO). Depression fact sheet. 2016. URL: http://www.who.int/mediacentre/factsheets/fs369/en/indexhtml [accessed 2014-08-22][WebCite Cache]. 2016.
- 53.Li W, Meng X, Xu Z, Yu Q, Shi J, Yu Y. et al. Prevalence, correlates of major depression: A mental health survey among undergraduates at a mainland C hinese university. Asia Pac Psychiat. 2016;8(3):206–14. doi: 10.1111/appy.12202. [DOI] [PubMed] [Google Scholar]
- 54.Albert PR. Why is depression more prevalent in women? Journal of psychiatry & neuroscience: JPN. 2015;40(4):219. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: analysis of the National Comorbidity Survey Replication. JAMA psychiat. 2013;70(10):1100–6. doi: 10.1001/jamapsychiatry.2013.1985. [DOI] [PubMed] [Google Scholar]
- 56.Mohammadi M, Davidian H, Nourbala A, Malek AH, Naghavi H, Pouretemad HR. et al. An epidemiological study of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;26:1–16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]