Summary
Background
We previously showed that small interfering RNAs (siRNAs) targeting the Zaire Ebola virus (ZEBOV) RNA polymerase L protein formulated in stable nucleic acid-lipid particles (SNALPs) completely protected guineapigs when administered shortly after a lethal ZEBOV challenge. Although rodent models of ZEBOV infection are useful for screening prospective countermeasures, they are frequently not useful for prediction of efficacy in the more stringent non-human primate models. We therefore assessed the efficacy of modified non-immunostimulatory siRNAs in a uniformly lethal non-human primate model of ZEBOV haemorrhagic fever.
Methods
A combination of modified siRNAs targeting the ZEBOV L polymerase (EK-1 mod), viral protein (VP) 24 (VP24-1160 mod), and VP35 (VP35-855 mod) were formulated in SNALPs. A group of macaques (n=3) was given these pooled anti-ZEBOV siRNAs (2 mg/kg per dose, bolus intravenous infusion) after 30 min, and on days 1, 3, and 5 after challenge with ZEBOV. A second group of macaques (n=4) was given the pooled anti-ZEBOV siRNAs after 30 min, and on days 1, 2, 3, 4, 5, and 6 after challenge with ZEBOV.
Findings
Two (66%) of three rhesus monkeys given four postexposure treatments of the pooled anti-ZEBOV siRNAs were protected from lethal ZEBOV infection, whereas all macaques given seven postexposure treatments were protected. The treatment regimen in the second study was well tolerated with minor changes in liver enzymes that might have been related to viral infection.
Interpretation
This complete postexposure protection against ZEBOV in non-human primates provides a model for the treatment of ZEBOV-induced haemorrhagic fever. These data show the potential of RNA interference as an effective postexposure treatment strategy for people infected with Ebola virus, and suggest that this strategy might also be useful for treatment of other emerging viral infections.
Funding
Defense Threat Reduction Agency.
Introduction
For more than 30 years, Ebola virus (EBOV) has been associated with periodic episodes of haemorrhagic fever in Central Africa that produce severe disease in infected patients. Mortality rates during outbreaks have ranged from 50% with the Sudan species of EBOV (SEBOV) to up to 90% with the Zaire species (ZEBOV).1 An outbreak towards the end of 2007, caused by an apparently new species of EBOV in Uganda, seemed to be less pathogenic than SEBOV or ZEBOV with a case fatality rate of about 25%.2
EBOV particles contain a non-infectious RNA genome of roughly 19 kilobases that encodes seven structural proteins and one non-structural protein. The gene order is 3′ leader, nucleoprotein, virion protein (VP) 35 (VP35), VP40, glycoprotein, VP30, VP24, polymerase L protein, and 5′ trailer.3 Four of these proteins—nucleoprotein, VP30, VP35, and the polymerase L protein—are associated with the viral genomic RNA in the ribonucleoprotein complex. The L protein and VP35 make up the polymerase complex, which transcribes and replicates the EBOV genome. The L protein provides the RNA-dependent RNA polymerase activity of the complex. This protein is an ideal target for antiviral interventions not only because its suppression should lead to a nearly complete loss of all RNA synthesis, but also because of the absence of similar proteins in mammalian cells. VP24 and VP35 are also promising targets for antiviral interventions since both have been shown to have inhibitory effects on the host type 1 interferon response. Specifically, VP35 functions as a type 1 interferon antagonist by blocking the activation of interferon regulatory factor 3 and possibly preventing transcription of interferon β.4 Consistent with these findings, mutations of ZEBOV VP35 rendered an adapted virus avirulent in guineapigs.5 VP24 expression interferes with type 1 interferon signalling,6 and mutations in VP24 have been linked to adaptation by ZEBOV to produce a lethal infection in mice7 and guineapigs.8
Although there are no vaccines or postexposure treatments for prevention or management of EBOV infections, progress has been made over the past few years in the development of candidate preventive vaccines that can protect non-human primates against infection with EBOV.1 Progress in the development of antiviral drugs and other postexposure interventions has been much slower. RNA interference represents a promising intervention for the treatment of diseases, including those caused by viruses. Indeed, RNA interference has been used in cell culture systems and rodents to inhibit the replication of several pathogens that cause disease in human beings. However, its usefulness as an effective treatment in non-human primate models of human infectious diseases has been assessed in only two studies.9, 10 Small interfering RNAs (siRNAs) inhibited the replication of hepatitis GB virus B in a non-lethal marmoset surrogate model of human hepatitis C.9 siRNAs against severe acute respiratory syndrome (SARS) coronavirus inhibited the virus replication in a non-lethal rhesus monkey model.10 However, unmodified immune stimulatory siRNAs were used in both of these studies, potentially confounding the interpretation of the results. Until now, the usefulness of RNA interference as a postexposure treatment has not been assessed in a lethal model of a human infectious disease in non-human primates.
In a previous study, we identified EK-1, an siRNA that targeted the ZEBOV polymerase L protein, and inhibited the replication of ZEBOV in vitro, and completely protected ZEBOV-infected guineapigs.11 Although EK-1 was effective, we chose to use a cocktail of three siRNAs in the present study, one each for ZEBOV L protein, VP24, and VP35 genes for further studies in non-human primates on the premise that a combination of siRNAs will aid in targeting potential RNA-interference escape mutants, as has been shown for HIV-1 and polio viruses.12 By targeting three different viral gene products, we also aimed to inactivate the virus in three different stages of its life cycle.
Methods
Design and in-vitro screening of siRNAs
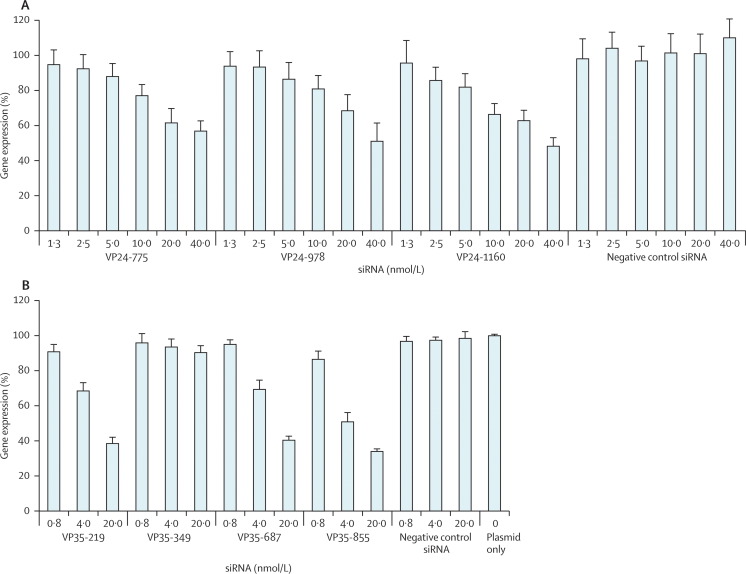
We designed siRNAs to target regions of the ZEBOV (Mayinga strain) polymerase L, VP24, and VP35 genes using a conventional siRNA design algorithm. We excluded siRNAs with sequence homology to any human reference mRNAs of 16 or more contiguous bases within the core duplex using the Basic Local Alignment Search Tool (version 2.2.13). The siRNA duplexes were synthesised by Dharmacon (Chicago, IL, USA) or Integrated DNA Technologies BVBA (Leuven, Belgium). EK-1 was previously described.11 siRNAs for targeting the VP24 and VP35 genes were identified by screening in vitro for reduction in expression of the ZEBOV VP24 or ZEBOV VP35 viral transgene inserted in the psiCHECK2 dual-luciferase plasmid system (Promega, Madison, WI, USA) under the control of the SV40 promoter in HepG2 cells. 10 μL of Lipofectamine 2000 (Invitrogen, Life Technologies, Carlsbad, CA, USA) complexes containing 0·75 μg of plasmid and 10 μL of siRNA (VP24-775, VP24-978, VP24-1160, or a non-specific negative control siRNA at 1·3 nmol/L, 2·5 nmol/L, 5·0 nmol/L, 10·0 nmol/L, 20·0 nmol/L, and 40·0 nmol/L; or VP35-219, VP35-349, VP35-687, VP35-855, or a non-specific negative control siRNA at 0·8 nmol/L, 4·0 nmol/L, and 20·0 nmol/L) were added to a 96-well plate before addition of 80 μL of HepG2 cells (15 000 cells per well). Cells were lysed 48 h after transfection. The dual-luciferase reporter assay system (Promega) and a Berthold luminometer (Berthold Detection Systems, Pforzheim, Germany) were used to measure Renilla luciferase (fused to ZEBOV VP24 or ZEBOV VP35 transgene) and firefly luciferase signals. The Renilla luciferase signal was normalised to the firefly luciferase signal and expressed as percentage gene expression relative to a plasmid-only control assigned a value of 100%. Table 1 shows the sequences of siRNAs that were used.
Table 1.
Targets and target sequences in Zaire Ebola virus (ZEBOV) of small interfering RNAs
| ZEBOV target | Sequence | |
|---|---|---|
| EK-1 mod | L polymerase | Sense 5′-GmUACGAAGCUmGUAUAmUAAAUU-3′, antisense 5′-UUUAmUAUACAGCUUCGmUACAA-3′ |
| VP24-775 | VP24 | Sense 5′-GCUGAUUGACCAGUCUUUGAU-3′, antisense 5′-CAAAGACUGGUCAAUCAGCUG-3′ |
| VP24-978 | VP24 | Sense 5′-ACGGAUUGUUGAGCAGUAUUG-3′, antisense 5′-AUACUGCUCAACAAUCCGUUG3′ |
| VP24-1160 | VP24 | Sense 5′-UCCUCGACACGAAUGCAAAGU-3′, antisense 5′-UUUGCAUUCGUGUCGAGGAUC-3′ |
| VP24-1160 mod | VP24 | Sense 5′-UCCmUCGACACGAAmUGCAAAGU-3′, antisense 5′-UUmUGCAUUCGUGUCmGAGmGAUC-3′ |
| VP35-219 | VP35 | Sense 5′-GCGACAUCUUCUGUGAUAUUG-3′, antisense 5′-AUAUCACAGAAGAUGUCGCUU-3′ |
| VP35-349 | VP35 | Sense 5′-GGAGGUAGUACAAACAUUGdTdT-3′, antisense 5′-CAAUGUUUGUACUACCUCCdTdT-3′ |
| VP35-687 | VP35 | Sense 5′-GGGAGGCAUUCAACAAUCUAG-3′, antisense 5′-AGAUUGUUGAAUGCCUCCCUA-3′ |
| VP35-855 | VP35 | Sense 5′-GCAACUCAUUGGACAUCAUUC-3′, antisense 5′-AUGAUGUCCAAUGAGUUGCUA-3′ |
| VP35-855 mod | VP35 | Sense 5′-GCAACmUCAUUGmGrArCrAmUCAUUC-3′, antisense 5′-AUGAUmGUCCAAUGAmGUmUGCUA-3′ |
| Luc | NA | Sense 5′-GAUUAUGUCCGGUUAUGUAAA-3′, antisense 5′-UACAUAACCGGACAUAAUCAU-3′ |
| Luc mod | NA | Sense 5′-GAmUmUAmUGmUCCGGmUmUAmUGmUAAA-3′, antisense 5′-UACAmUAACCGGACAmUAAmUCAU-3′ |
Sequences used in the non-human primate studies contain an m in front of the base that designates a 2′-O-methyl modification (unmodified versions do not have any 2′-O-methyl modified bases). mod=modified. Luc mod=modified luciferase. NA=not applicable.
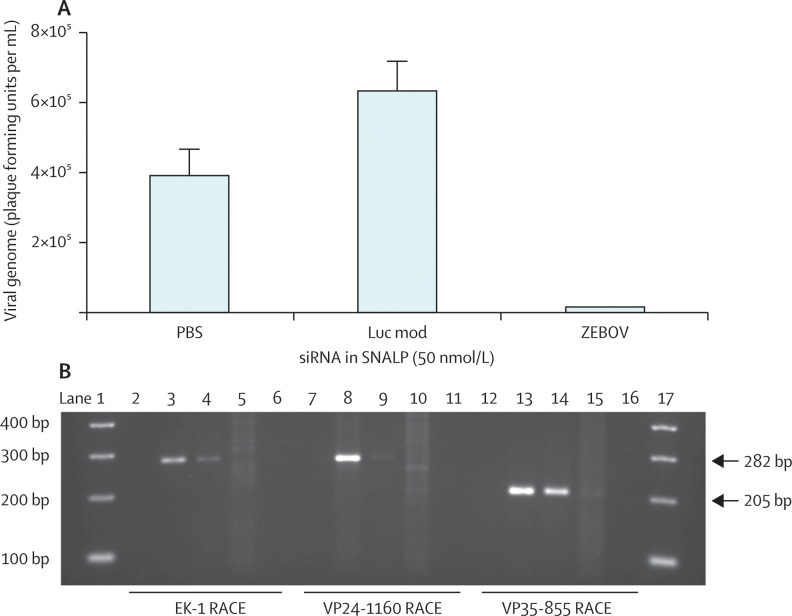
ZEBOV infection of Vero E6 cells
To assess whether mRNAs for polymerase L, VP35, and VP24 were cleaved by the specific mechanism of RNA interference, we plated Vero E6 cells at 100 000 cells per mL (2 mL per well in a six-well plate), and after 24 h treated them with stable nucleic acid-lipid particles (SNALPs; 50 nmol/L) containing siRNAs modified by substitution of 2′-O-methyl versions of guanines and uridines (EK-1-mod, VP24-1160-mod, or VP35-855-mod), ZEBOV cocktail (consisting of EK-1-mod, VP24-1160-mod, and VP35-855-mod in a 1:1:1 ratio), or luciferase siRNA (Luc mod) for 16 h before infection with ZEBOV (Kikwit strain, at 0·1 multiplicity of infection). 24 h after infection, cell supernatants were harvested for quantitative real-time RT-PCR, and cell monolayers were lysed with Trizol (Invitrogen) for isolation of total RNA and rapid amplification of cDNA ends (5′RACE; Invitrogen).
Quantitative RT-PCR
We purified viral RNA using the Qiagen QIAmp viral RNA mini kit (Qiagen, Valencia, CA, USA) according to the manufacturer's protocol. One-step quantitative real-time RT-PCR reactions were done on a LightCycler 480 (Roche, Indianapolis, IN, USA) in 20 μL volumes with 5 μL of purified RNA and the Superscript III One-Step RT-PCR System (Invitrogen). Primers (forward 5′-CGGACCTGGTTTGGTTGTG-3′; reverse 5′-GCTGCAGTGTCGCATCTGA-3′) and TaqMan probe (6-carboxyfluorescein-5′-CCCTTGCCACAATCT-minor groove binder non-fluorescent quencher-3′) from Applied Biosystems (Foster City, CA, USA) were specific for the ZEBOV glycoprotein gene. Cycling conditions were reverse transcription at 50°C for 20 min, and initial denaturation at 95°C for 5 min; followed by 45 cycles of denaturation at 95°C for 5 s, and annealing, synthesis, and single acquisition at 60°C for 20 s; and final cooling at 40°C for 30 s. Absolute quantification of viral gene expression was based on a viral RNA standard by use of the LC480 software (version 1.50).
5′ RACE assays
RNA extraction and 5′ RACE were done as described11 except we used gene-specific primers (GSP) for cDNA production: EK-1 GSP (5′-TTTGTGATTCGTCCTTTTGCAGT3-′), VP24-1160 GSP (5′-AGCAATTCTATGATGTTGTCTTGGA-3′), or VP35-855 GSP (5′-CATCACTTTTGGTTTGGGTTACTT-3′); and reverse-2 (Rev2) primers for the 5′ RACE PCR: EK-1 Rev2 (5′-TGAGATGGTTTTGGTGTGGCATCT-3′), VP24-1160 Rev2 (5′-CCTGGTTTTTGTAAGGGTGTCAACT-3′), or VP35-855 Rev2 (5′-TTTCTGGCAAGCTCGGGGAATGT-3′). Sequencing primers (seq) were EK-1 3′seq (5′-AGCCATAACATACCCTCAGT-3′), VP24-1160 3′seq (5′-ATGAAAGCAGAGATGTCAAG-3′), or VP35-855 3′seq (5′-ATTAGGGCACATTGAGGAG-3′). The predicted size of the RACE PCR product for EK-1 and VP24-1160 was 282 base pairs, and that for VP35-855 was 205 base pairs. Samples were processed from two separate transfections with similar results.
In-vitro immune stimulation assays
Peripheral blood mononuclear cells (PBMCs) were isolated from whole blood from healthy donors by use of a standard Ficoll-Hypaque density centrifugation technique. Immune stimulation assays were done as previously described.13 Native (unmodified) or 2′-O-methyl-modified siRNAs (100 nmol/L, 200 nmol/L, or 400 nmol/L) were cultured with PBMCs for 24 h. The lower limit of quantification of interferon α was 15·6 pg/mL. Mean (SD) was calculated for three separate culture wells in one representative experiment.
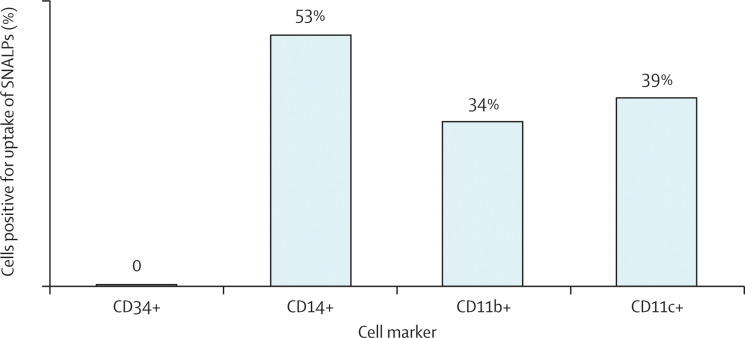
Differentiation and SNALP uptake in CD34-positive cells
Human cord blood CD34-positive stem cells (Stem Cell Technologies, Vancouver, BC, Canada) were cultured for 5 days in Iscove's modified Dulbecco's medium with Glutamax (Invitrogen), 20% BIT9500 serum substitute (Stem Cell Technologies), human LDL (40 μg/mL; Calbiochem, San Diego, CA, USA), β mercaptoethanol (55 μmol/L), human peptide deformylase-related tyrosine kinase-3 ligand (100 ng/mL), human stem-cell factor (100 ng/mL), and human thrombopoietin (10 ng/mL; all four Peprotech, Rocky Hill, NJ, USA). Cell media were replaced every 3 days. To prime cells for differentiation into those positive for CD11c, CD11b, and CD14, we supplemented them with recombinant human interleukins 3 (20 ng/mL) and 6 (20 ng/mL; both R&D Systems, Minneapolis, MN, USA) on day 6. On day 10, cells were differentiated into a mixed myeloid dendritic cell and macrophage culture by the addition of recombinant human macrophage colony-stimulating factor (50 ng/mL) and recombinant human granulocyte-macrophage colony-stimulating factor (20 ng/mL; both, Peprotech).
Cultures of differentiated cells were incubated with SNALPs containing fluorescein isothiocyanate (FITC, 150 nmol/L)-labelled Luc mod for 4 h and then harvested, washed with 2% fetal bovine serum in phosphate-buffered saline (PBS), and stained with fluorescent-labelled antibodies (BD Biosciences, San Jose, CA, USA) against cell phenotype markers (CD11c, CD11b, CD14, and CD34). Cells with uptake of SNALPs containing FITC-labelled Luc mod were separated according to phenotype and analysed on a three-laser, eight-colour LSRII flow cytometer with FACSDiva software (version 6.0).
Mouse studies
Mouse studies were completed in accordance with the Canadian Council on Animal Care guidelines following approval by the local animal care and use committee at Tekmira Pharmaceuticals. Animal research was done in compliance with the animal welfare act, and other federal statutes and regulations relating to animals and experiments involving animals, and adheres to the principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 1996. The facilities used are fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
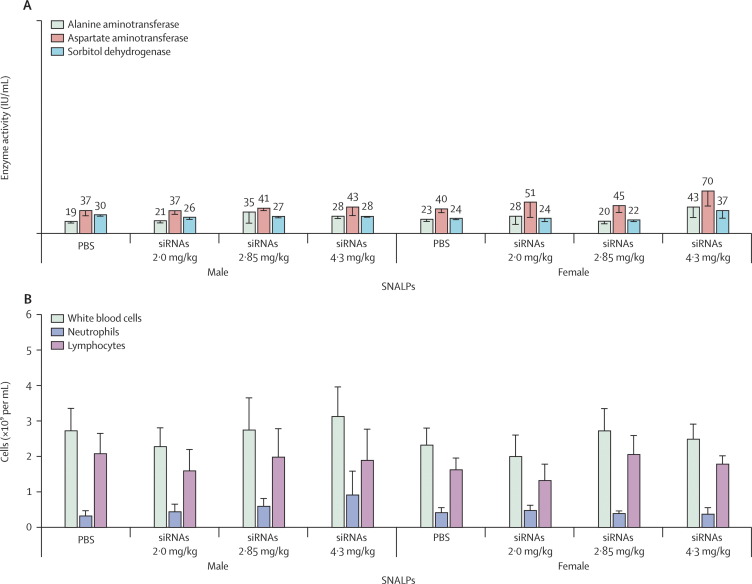
6–8-week-old female CD1 ICR mice (n=16; immunostimulation studies [four mice per group]), and 6–8-week-old male (n=20) and female B6C3F1 mice (n=20; tolerability studies [five mice per group]) were quarantined and acclimatised for 1 week before the studies. SNALPs were administered by bolus injection in the lateral tail vein in 0·2 mL PBS. In the immune stimulation studies, plasma and livers were harvested 4 h after mice were injected with SNALPs containing a cocktail of siRNAs (5 mg/kg). Analysis of concentrations of cytokines in plasma, and interferon-induced protein with tetratricopeptide repeats (IFIT1) mRNA (upregulation of this mRNA in tissues is a more sensitive measure of localised interferon production than is plasma interferon protein ELISA assay14) in liver was done as previously reported.15 The lower limit of quantification of interferon α or interleukin 6 with ELISA was 15·6 pg/mL. As an initial assessment of the tolerability in animals, we injected SNALPs into uninfected mice (2·0 mg/kg per day, 2·8 mg/kg per day, or 4·3 mg/kg per day for 7 days), and then euthanised them 48 h after the final dose. The cumulative doses (14 mg/kg, 20 mg/kg, and 30 mg/kg) equalled and exceeded the expected dosing intensity in the non-human primate efficacy model. Blood serum was analysed for clinical chemistry and activity of alanine aminotransferase, aspartate aminotransferase, and sorbitol dehydrogenase; and complete blood counts were done. Clinical signs and organ weights were monitored in all studies.
Lipid encapsulation of siRNAs
siRNAs were encapsulated in SNALPs by the process of spontaneous vesicle formation as reported by Jeffs and colleagues.16 ZEBOV siRNAs were formulated as a cocktail in the same lipid particles. SNALPs consisted of synthetic cholesterol (Sigma-Aldrich, St Louis, MO, USA), dipalmitoylphosphatidylcholine (Avanti Polar Lipids, Alabaster, AL, USA), 3-N-[(ω-methoxy poly(ethylene glycol)2000)carbamoyl]-1,2-dimyrestyloxy-propylamine,17 and cationic 1,2-dilinoleyloxy-3-N,N-dimethylaminopropane.17 The resulting SNALPs were dialysed against PBS and filter sterilised through a 0·2 μm filter before use. Particle sizes for all batches were 81–85 nm (eg, the average size of SNALPs containing ZEBOV SNALPs used in the non-human primate study 1 was 81·7 nm) with a low polydispersity value (<0·15), indicating particle homogeneity and no aggregation. Typically 90–95% of siRNAs were encapsulated within the lipid particles. The amount of endotoxin was less than 1·5 EU/mg siRNA for all batches.
Non-human primate studies
We investigated the protective efficacy of our lead anti-ZEBOV siRNAs in an established rhesus macaque model of ZEBOV-induced haemorrhagic fever.18 A combination of modified siRNAs that targeted the ZEBOV genes for polymerase L (EK-1 mod), VP24 (VP24-1160 mod), and VP35 (VP35-855 mod; table 1) were formulated in SNALPs. The studies were done in biosafety-level-4 biocontainment at the US Army Medical Research Institute of Infectious Diseases and were approved by the US Army Medical Research Institute of Infectious Diseases laboratory animal care and use committee.
Nine healthy, filovirus-seronegative Chinese rhesus macaques (Macaca mulatta; 5–8 kg) were used for the non-human primate studies. Hickman, Leonard, Broviac central venous catheters (BARD Access Systems, Salt Lake City, UT) were inserted into the macaques as previously described.19 The monkeys were then placed in primate jackets (Lomir Biomedical, Malone, NY, USA), returned to their cages, and tethered. A continuous intravenous infusion of saline (2 mL/h) was provided to all animals during the entire study with a basic single syringe KDS100 infusion pump (KDS Scientific, Holliston, MA, USA). After 7 days, the animals were inoculated intramuscularly with a target dose of 1000 plaque-forming units (pfu) of ZEBOV (Kikwit strain; actual dose 1100 pfu in study 1 and 1325 pfu in study 2).
In the first study, the pool of anti-ZEBOV siRNAs formulated in SNALPs (2 mg/kg total siRNA per dose, bolus intravenous infusion) was administered to three of four macaques 30 min after the ZEBOV challenge, and the control animal was not given any treatment. The three treated animals were given additional treatments of the SNALP-formulated anti-ZEBOV siRNAs at the same dose on days 1, 3, and 5 after the ZEBOV challenge, while the control animal was not given any treatment.
In the second study, we investigated whether increasing the frequency of treatments could improve outcome. The pool of SNALP-formulated anti-ZEBOV siRNAs (2 mg/kg per dose, bolus intravenous infusion) was administered to four of five macaques 30 min after the ZEBOV challenge, while the control animal was given an equal dose of SNALP-formulated non-specific modified siRNAs (Luc mod) 30 min after the ZEBOV challenge. The animals were given additional treatments of the SNALP-formulated anti-ZEBOV siRNAs or the SNALP-formulated non-specific siRNA (control) on days 1, 2, 3, 4, 5, and 6 after the ZEBOV challenge. Animals were given physical examinations, and blood was collected in tubes containing EDTA at the time of challenge and on days 3, 6, 10, 14, 22, and 40–43 after filovirus challenge.
Haematology and serum biochemistry
In the non-human primate studies, we used a laser-based haematological analyser (Coulter Electronics, Hialeah, FL, USA) to obtain total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, haematocrit values, total haemoglobin, mean cell volume, mean corpuscular volume, and mean corpuscular haemoglobin concentration. We used a Piccolo point-of-care blood analyser (Abaxis, Sunnyvale, CA, USA) to measure concentrations of albumin, amylase, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, γ glutamyltransferase, glucose, cholesterol, total protein, total bilirubin, blood urea nitrogen, and creatinine in serum samples.
Virus detection by plaque assay
For virus titration, we used a conventional plaque assay on Vero E6 cells from cell culture fluids of blood samples collected from rhesus monkeys as previously described.20
Role of the funding source
The sponsor provided financial support for the study but had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had access to the primary data, take responsibility for accuracy and completeness of data reporting, and had final responsibility for the decision to submit for publication.
Results
VP24-1160 was the most efficacious siRNA at silencing ZEBOV VP24 gene in HepG2 cells, and VP35-855 was most efficacious at silencing ZEBOV VP35 gene (figure 1 ). These sequences, and EK-1,11 were selected as the siRNAs of the ZEBOV SNALP cocktail. Since non-selective chemical modification might attenuate the potency of the siRNA, we selectively modified lead siRNAs by substituting 2′-O-methyl guanosine or uridines in both strands to eliminate the immune stimulatory capacity of the siRNA duplex,13, 14, 15 and confirmed the gene silencing activity of the modified versions using the in-vitro plasmid-based ZEBOV gene expression system (data not shown).
Figure 1.
Effect of small interfering RNAs (siRNAs) targeting virion protein genes VP24 (A) and VP35 (B) of Zaire Ebola virus (ZEBOV) expressed in a non-viral plasmid-based system in HepG2 cells
Error bars represent SD of triplicate tissue culture wells.
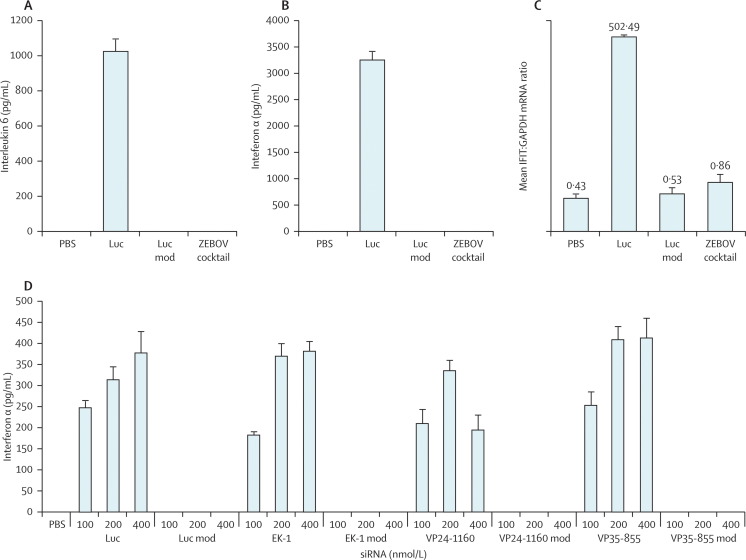
SNALPs containing modified ZEBOV siRNAs did not induce interferon α or interleukin 6 in the plasma of mice, whereas SNALPs containing chemically unmodified Luc siRNA induced high concentrations of both plasma cytokines (figure 2A and B ). Analysis of liver IFIT1 mRNA showed no differences between SNALPs containing PBS (negative control) and those containing the 2′-O-methyl-modified Luc or ZEBOV siRNA cocktail, whereas the SNALPs containing unmodified Luc induced high levels of IFIT1 mRNA (1169-fold greater than the PBS control; figure 2). No differences were noted in clinical signs and organ weights of mice treated with SNALPs containing siRNAs or PBS. Native (chemically unmodified) versions of Luc, EK-1, VP24-1160, and VP35-855 siRNAs also induced high levels of interferon α in cultures of human PBMCs, whereas the 2′-O-methyl-modified versions of siRNAs at up to 400 nmol/L did not induce any interferon α (figure 2).
Figure 2.
Effect of small interfering RNAs (siRNAs) on synthesis of interleukin 6 (A) and interferon α (B), induction of interferon-induced protein with tetratricopeptide repeats (IFIT1) mRNA in mice (C), and induction of interferon α in human peripheral blood mononuclear cell cultures (D)
Data are mean (SD). Error bars represent SD. Luc=luciferase. PBS=phosphate-buffered saline. Luc mod=modified luciferase. GAPDH=glyceraldehyde 3-phosphate dehydrogenase.
Figure 3A shows that SNALPs containing ZEBOV siRNAs substantially reduced ZEBOV produced in supernatants of Vero E6 cells 48 h after infection. Figure 3B shows that SNALPs containing EK-1-mod, VP35-855-mod, or VP24-1160-mod induced specific mRNA cleavage only of their target mRNA in the cells, whereas all three PCR products of the correct predicted size were present in cells treated with SNALPs containing the ZEBOV cocktail of siRNAs (figure 3B). No 5′RACE PCR products of the predicted size were noted in cells treated with SNALPs containing PBS or Luc mod (figure 3B), further showing the specificity of the assay. The sequences of the 5′RACE PCR products (data not shown) corresponded to the specific cleavage products of polymerase L protein, VP24, and VP35 mRNAs, thereby confirming the specific mechanism of RNA interference.
Figure 3.
Rapid amplification of cDNA ends (RACE)-PCR of small interfering RNA (siRNA)-mediated cleavage of Zaire Ebola virus (ZEBOV) L polymerase, virion protein (VP) 24 (VP24), and VP35 mRNAs in ZEBOV-infected Vero E6 cells
Vero E6 cells were treated with stable nucleic acid-lipid particles (SNALPs) containing ZEBOV siRNA cocktail, modified luciferase (Luc mod), or phosphate-buffered saline (PBS). (B) Vero E6 cells were treated with SNALPs containing EK-1-mod, VP24-1160-mod, VP35-855-mod, ZEBOV siRNA cocktail, Luc mod, or PBS. The order of samples for each RACE PCR shown in the gel is SNALPs containing PBS, single gene-specific siRNAs (EK-1-mod, VP24-1160-mod, or VP35-855-mod), ZEBOV cocktail, and Luc mod. Lanes 1 and 17 are the 100 base pair (bp) ladder, lanes 2–5 are EK-1 RACE PCR, lanes 7–10 are VP24-1160 RACE, and lanes 12–15 are VP35-855 RACE. Lanes 6, 11, and 16 are empty.
To show that our anti-ZEBOV siRNAs targeted populations of cells that were relevant to filovirus infection, we assessed the uptake of the SNALPs in livers of mice and in human CD34-derived myeloid cell cultures. The SNALPs enabled entry of siRNAs into cells of the reticuloendothelial system as shown by the uptake of fluorescent SNALPs into Kupffer cells in the murine liver (data not shown), and into subsets of human myeloid cells that were positive for CD14, CD11b, and CD11c (figure 4 ). These data showed that SNALPs were actively taken up by the reticuloendothelial cell populations most relevant to EBOV infection.
Figure 4.
Proportion of differentiated cells with uptake of stable nucleic acid-lipid particles (SNALPs) containing fluorescein-isothiocyanate-labelled modified luciferase small interfering RNAs
In the tolerability studies, activities of alanine aminotransferase, aspartate aminotransferase, and sorbitol dehydrogenase remained unchanged 48 h after the mice were given the final dose of SNALPs containing ZEBOV siRNAs, even at the highest cumulative dose (figure 5A ). Complete blood cell and differential counts were also unaffected at the doses tested in the mice (figure 5B).
Figure 5.
Effect of daily administration of stable nucleic acid-lipid particles (SNALPs) containing Zaire Ebola virus (ZEBOV) small interfering RNAs on activities (siRNAs) of alanine aminotransferase, aspartate aminotransferase, and sorbitol dehydrogenase (A), and blood cell counts (B) in mice
PBS=phosphate-buffered saline.
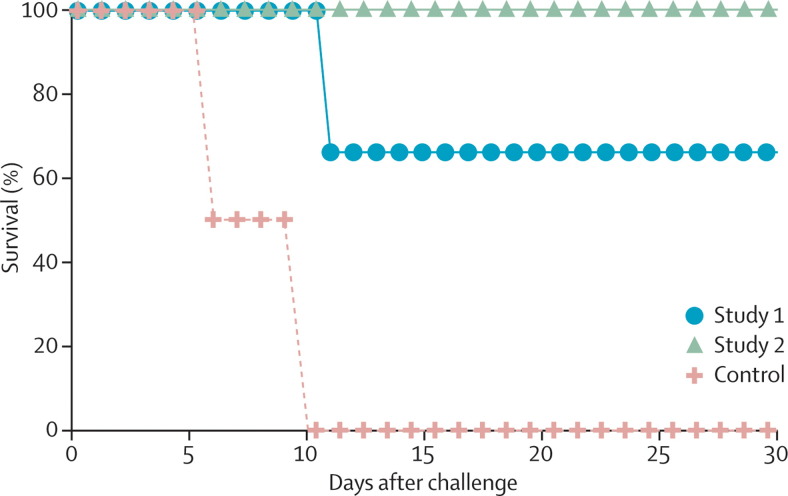
All three macaques given four treatments of SNALPs containing pooled siRNAs, and the control, developed clinical symptoms that were consistent with ZEBOV-induced haemorrhagic fever by day 6 (table 2 ). The control animal succumbed to ZEBOV infection before blood collection on day 6 (figure 6 ). One treated animal (number 3) developed a high ZEBOV viraemia on day 6 (table 3 ) and succumbed on day 10 (figure 6). ZEBOV was detected in the plasma of one of the remaining treated animals (number 2) on day 6, but we were unable to detect ZEBOV in the plasma of the other remaining treated animal (number 1; table 3). Both of these animals survived. Seven doses of SNALPs containing pooled siRNAs were more effective because clinical symptoms of ZEBOV infection in the treated macaques were less severe than in those given four doses (table 2). The control animal injected with SNALPs containing Luc mod succumbed to haemorrhagic fever on day 10, whereas all four animals given the pooled anti-ZEBOV siRNAs survived (figure 6). ZEBOV was detected in the plasma of the second control animal on days 3, 6, and 10 (table 3). Low levels of ZEBOV were detected on day 6 in the plasma of all four macaques injected with SNALPs containing ZEBOV siRNAs, and on day 10 in one of these animals (animal 6), whereas we were unable to detect ZEBOV in any of these animals on day 14 (table 3). Peak viraemia in surviving siRNA-treated macaques never exceeded 2·4 log10 pfu/mL (table 3).
Table 2.
Macaques given four (study 1) or seven treatments (study 2) with stable nucleic acid-lipid particles containing Zaire Ebola virus (ZEBOV) small interfering RNAs (siRNAs) after ZEBOV challenge
| Adverse events on days 1–35 after ZEBOV challenge | Status | |
|---|---|---|
| Study 1 | ||
| Animal 1 | Anorexia (days 7–9), lymphopenia (day 6), >5-fold increase in AST (day 10) | Survived |
| Animal 2 | Fever (day 6), mild rash (days 8,11, and 12), moderate rash (days 9 and 10), depression (days 7–11), anorexia (days 7–11), diarrhoea (day 12), lymphopenia (days 6 and 14), thrombocytopenia (day 6), 2–3-fold increase in ALP (day 10), 2–3-fold increase in ALT (day 10), 2–3-fold increase in AST (day 6), >5-fold increase in AST (day 10), >5-fold increase in GGT (day 10) | Survived |
| Animal 3 | Mild rash (days 6–10), depression (days 6–-10), anorexia (days 6–10), bleeding at venepuncture site (day 10), recumbency (day 10), thrombocytopenia (day 6), 2–3-fold increase in ALP (day 6), >5-fold increase in ALP (day 10), 4–5-fold increase in ALT (day 10), 2–3-fold increase in AST (day 3), >5-fold increase in AST (days 6 and 10), >5-fold increase in BUN (day 10), >5-fold increase in creatinine (day 10), >5-fold increase in GGT (day 10) | Died on day 10 |
| Control 1* | Mild rash, anorexia, and depression on day 5 | Died day 6 |
| Study 2 | ||
| Animal 4 | Thrombocytopenia (days 6 and 10), 4–5-fold increase in AST (day 6) | Survived |
| Animal 5 | >5-fold increase in AST (day 6), 2–3-fold increase in AST (day 10) | Survived |
| Animal 6 | Fever (day 10), lymphopenia (day 6), thrombocytopenia (days 6, 10, and 14), 2–3-fold increase in AST (day 10) | Survived |
| Animal 7 | Fever (day 10), lymphopenia (day 6), thrombocytopenia (day 6), >5-fold increase in AST (day 10) | Survived |
| Control 2† | Fever (day 6), moderate rash (day 10), recumbency (day 10), thrombocytopenia (day 6) 2–3-fold increase in ALT (day 6), >5-fold increase in ALT (day 10), >5-fold increase in AST (days 6 and 10), >5-fold increase in BUN (day 10), 2–3-fold increase in creatinine (day 10) | Died on day 10 |
Fever was defined as a temperature that was 2·5° greater than baseline temperature or at least 1·5° greater than baseline temperature, and at least 103·5°F. Mild rash was defined as focal petechiae covering less than 10% of skin. Moderate rash was defined as petechiae covering between 10% and 40% of skin. Severe rash was defined as petechiae or ecchymoses covering more than 40% of skin. Lymphopenia was defined as at least a 35% reduction in numbers of lymphocytes; and thrombocytopenia was defined as at least a 35% reduction in numbers of platelets. AST=aspartate aminotransferase. ALP=alkaline phosphatase. ALT=alanine aminotransferase. GGT=γ glutamyltransferase. BUN=blood urea nitrogen.
Not given any siRNAs.
Given seven treatments with non-specific siRNAs.
Figure 6.
Survival curves for Zaire Ebola virus (ZEBOV)-infected rhesus macaques treated after challenge with stable nucleic acid-lipid particles containing ZEBOV small interfering RNAs
Study 1: four postexposure treatments. Study 2: seven post exposure treatments.
Table 3.
Plasma viral load in rhesus monkeys infected with Zaire Ebola virus (ZEBOV) and given four (study 1) and seven (study 2) postexposure treatments with anti-ZEBOV small interfering RNAs (siRNAs)
|
Plasma viral load (log10plaque-froming units) |
||||
|---|---|---|---|---|
| Day 3 | Day 6 | Day 10 | Day 14 | |
| Study 1 | ||||
| Animal 1 | 0 | 0 | 0 | 0 |
| Animal 2 | 0 | 0 | 2·2 | 0 |
| Animal 3 | 0 | 3·7 | 6·8 | NA |
| Control 1* | 0 | NA | NA | NA |
| Study 2 | ||||
| Animal 4 | 0 | 2·0 | 0 | 0 |
| Animal 5 | 0 | 2·4 | 0 | 0 |
| Animal 6 | 0 | 2·0 | 2·1 | 0 |
| Animal 7 | 0 | 2·1 | 0 | 0 |
| Control 2† | 0 | 4·1 | 6·7 | NA |
NA=not applicable.
Not given any siRNAs.
Given seven treatments with non-specific siRNAs.
Clinical assessments also showed that this aggressive SNALP treatment regimen was well tolerated in macaques with only minor changes in liver enzymes (alanine aminotransferase <2-fold increase, aspartate amino-transferase <6-fold increase), possibly related to viral infection. All six animals that survived the ZEBOV challenge in the two studies were healthy on day 40 and were euthanised on days 40–43.
Discussion
Seven treatments with anti-ZEBOV siRNAs inhibited the replication of the virus and completely protected rhesus monkeys against death from haemorrhagic fever. In previous studies, ZEBOV-infected rhesus monkeys succumbed when viraemia on days 6–10 after exposure was greater than 4·5 log10 pfu/mL, whereas animals treated therapeutically survived when the viraemia did not reach this level (Geisbert TW, unpublished).19, 21 In the current study, viraemia never exceeded 2·4 log10 pfu/mL in any surviving animal.
The development of treatments for EBOV-induced haemorrhagic fever has been slow and no previous candidate treatment has shown complete protection against ZEBOV haemorrhagic fever in non-human primates. Some success has been achieved with interventions that mitigate the coagulation disorders that characterise EBOV infection.19, 21 We protected 50% of non-human primates against ZEBOV by administering a live-attenuated recombinant vesicular stomatitis virus vaccine vector that expressed the ZEBOV glycoprotein shortly after a lethal ZEBOV challenge.22 Several new postexposure treatments based on siRNA11 and antisense oligomers23, 24 have shown promising results in rodent models, but there have been no reports of the assessment of either treatment strategy after EBOV challenge in non-human primates, which more faithfully reproduce human EBOV infections than do other animal models.1, 18 This model was rapid and uniformly lethal (death in all 21 naive rhesus macaques challenged with the same ZEBOV seed stock by the same dose and route as in the present study; Geisbert TW, unpublished) in which animals typically succumbed 6–10 days after challenge with the virus (mean time to death 8·3 days). The ZEBOV target in the siRNA postexposure treatment study in guineapigs was the L polymerase gene, and treatment initiated 1 h after ZEBOV challenge completely protected all animals.11 Targeting only VP35 completely protected mice against ZEBOV challenge when the antisense oligomers were administered 24 h after ZEBOV exposure.23 Targeting a combination of the L polymerase, VP24, and VP35 genes also completely protected mice and incompletely protected guineapigs when given 24 h after ZEBOV challenge.24
Although RNA-interference-mediated treatment strategies show potential for combating EBOV infections, systemic administration of synthetically manufactured siRNA duplexes can activate the innate immune response, inducing high levels of inflammatory cytokines such as tumour necrosis factor α, interleukin 6, and interferons, particularly interferon α which might contribute to antiviral activity in vivo.25, 26, 27 Off-target effects can be toxic to the host and also confound interpretation of preclinical data. siRNAs must therefore be modified to prevent detrimental immune activation in vivo, particularly because immunostimulation in human beings is much more toxic than in rodents.14, 25 We therefore tested immune stimulatory activity of SNALPs containing anti-ZEBOV siRNAs in mice and in human PBMC cultures. The ZEBOV cocktail was not immune stimulatory at the limit of sensitivity of the assays used. These data and the 5′RACE PCR data suggest that the antiviral effects in non-human primates are the result of specific RNA interference in reticuloendothelial cells and not due to immune stimulation or other off-target effects. Additionally, the death of the macaque given control Luc mod on day 10, which was within the normal range of expected time to death for historical untreated controls, also suggests that the ZEBOV-mediated protection was specific to the siRNAs and not related to off-target effects. When the immune toxicities associated with the siRNA component of SNALPs were abrogated through the use of selective chemical modification, the major remaining toxicity in mouse and non-human primate models was hepatotoxicity associated with the SNALP lipid components (MacLachlan I, unpublished). Preliminary tolerability studies in mice showed that seven daily doses of up to 4·3 mg/kg (30·0 mg/kg cumulative) of SNALPs containing ZEBOV siRNAs were well tolerated, corroborating the lack of hepatotoxicity (measured as increases in liver enzymes such as alanine aminotransferase and aspartate aminotransferase) in the treated macaques that survived infection.
Our investigation was designed as a proof-of-concept study. The rhesus macaque model that we used represents a worse-case scenario such as an accidental needle stick exposure of a laboratory worker or first responder to a high infectious dose of ZEBOV, which has occurred several times during the past 5 years.28, 29, 30 ZEBOV infection in human beings normally progresses slower than in macaques with case fatality rates in man ranging from 70–90%,1 suggesting that the therapeutic window could be larger than in experimentally infected macaques. Nonetheless, the focus in future studies will need to be on investigation of whether anti-ZEBOV siRNAs will be beneficial if administered at the onset of symptoms. Here, we show a substantial progress in the treatment of ZEBOV infections in non-human primates compared with previously described postexposure methods that afforded only partial protection of non-human primates against ZEBOV.19, 21, 22 To progress to license, studies will be done in guineapig and non-human primate models of ZEBOV infection in accordance with the US Food and Drug Administration's guidelines for the assessment of treatments for Centers for Disease Control and Prevention category A threats (number 21CFR314.610). Additionally, studies will need to be done to obtain data about pharmacology, dosing, and toxicology in uninfected non-human primates.
Acknowledgments
Acknowledgments
Work on filoviruses at US Army Medical Research Institute of Infectious Diseases was funded by the Defense Threat Reduction Agency (project number 04-4-7J-012). Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by Boston University or the US Army.
Contributors
TWG, ACHL, MR, AJ, LEH, and IM conceived and designed the experiments. TWG wrote the research programme plan and the animal protocol for the studies. LEH wrote modifications for the animal protocol. TWG and LEH selected the ZEBOV L polymerase as a target. TWG, ACHL, VS, MR, AJ, LEH, and IM selected ZEBOV VP24 and VP35 as targets. TWG co-designed the L polymerase siRNA, and ACHL and VS co-designed the VP24 and VP35 siRNAs. ACHL, VS, and AJ designed the modifications to the siRNAs. VS and ANH did the in vitro siRNA assays. JBG and JCJ did the Ebola challenge experiments in non-human primates and the clinical pathology assays. JBG did the Ebola virus infectivity assays. SDJ did the immunology and uptake assays. MR and IT did the 5′RACE assays. TWG, ACHL, MR, JBG, ANH, JCJ, AJ, LEH, and IM analysed the data. TWG and MR co-wrote the report. LEH and IM edited the report. All authors have seen and approved the final version of the report.
Conflicts of interest
TWG, ACHL, MR, VS, AJ, LEH, and IM claim intellectual property regarding RNA interference for the treatment of filoviral infections. ACHL, MR, VS, SDJ, IT, AJ, and IM are employees of Tekmira Pharmaceuticals. JCJ, ANH, and JBG declare that they have no conflicts of interest.
References
- 1.Sanchez A, Geisbert TW, Feldmann H. Filoviridae: Marburg and Ebola viruses. In: Knipe DM, Howley PM, editors. Fields virology. Lippincott Williams and Wilkins; Philadelphia: 2006. pp. 1409–1448. [Google Scholar]
- 2.Towner JS, Sealy TK, Khristova ML. Newly discovered Ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog. 2008;4:e1000212. doi: 10.1371/journal.ppat.1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanchez A, Kiley MP, Holloway BP, Auperin DD. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 1993;29:215–240. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- 4.Basler CF, Mikulasova A, Martinez-Sobrido L. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J Virol. 2003;77:7945–7956. doi: 10.1128/JVI.77.14.7945-7956.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prins KC, Delpeut S, Leung DW. Mutations abrogating VP35 interaction with double stranded RNA render Ebola virus avirulent in guinea pigs. J Virol. 2010;84:3004–3015. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reid SP, Leung DW, Hartman AL. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol. 2006;80:5156–5167. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebihara H, Takada A, Kobasa D. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2006;2:e73. doi: 10.1371/journal.ppat.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volchkov VE, Chepurnov AA, Volchkova VA, Ternovoj VA, Klenk HD. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology. 2000;277:147–155. doi: 10.1006/viro.2000.0572. [DOI] [PubMed] [Google Scholar]
- 9.Yokota T, Iijima S, Kubodera T. Efficient regulation of viral replication by siRNA in a non-human primate surrogate model for hepatitis C. Biochem Biophys Res Commun. 2007;361:294–300. doi: 10.1016/j.bbrc.2007.06.182. [DOI] [PubMed] [Google Scholar]
- 10.Tang Q, Li B, Woodle M, Lu PY. Application if siRNA against SARS in the rhesus macaque model. Methods Mol Biol. 2008;442:139–158. doi: 10.1007/978-1-59745-191-8_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geisbert TW, Hensley LE, Kagan E. Postexposure protection of guinea pigs against a lethal Ebola virus challenge is conferred by RNA interference. J Infect Dis. 2006;193:1650–1657. doi: 10.1086/504267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grimm D, Kay M. Combinatorial RNAi: a winning strategy for the race against evolving targets? Mol Ther. 2007;15:878–888. doi: 10.1038/sj.mt.6300116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Judge AD, Bola G, Lee ACH, MacLachlan I. Design of noninflammatory synthetic siRNA mediating potent gene silencing in vivo. Mol Ther. 2006;13:494–505. doi: 10.1016/j.ymthe.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Robbins MA, Judge AD, MacLachlan I. siRNA and innate immunity. Oligonucleotides. 2009;19:89–101. doi: 10.1089/oli.2009.0180. [DOI] [PubMed] [Google Scholar]
- 15.Judge A, Robbins M, Tavakoli I. Confirming the RNAi-mediated mechanism of action of siRNA-based cancer therapeutics in mice. J Clin Invest. 2009;119:661–673. doi: 10.1172/JCI37515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeffs LB, Palmer LR, Ambegia EG, Giesbrecht C, Ewanick S, MacLachlan I. A scalable, extrusion-free method for efficient liposomal encapsulation of plasmid DNA. Pharm Res. 2005;22:362–372. doi: 10.1007/s11095-004-1873-z. [DOI] [PubMed] [Google Scholar]
- 17.Heyes J, Palmer L, Bremner K, MacLachlan I. Cationic lipid saturation influences intracellular delivery of encapsulated nucleic acids. J Control Release. 2005;107:276–287. doi: 10.1016/j.jconrel.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Geisbert TW, Jahrling PB, Larsen T, Davis KJ, Hensley LE. Filovirus pathogenesis in nonhuman primates. In: Klenk HD, Feldmann H, editors. Ebola and Marburg viruses: molecular and cellular biology. Horizon Bioscience; Norfolk: 2004. pp. 203–238. [Google Scholar]
- 19.Hensley LE, Stevens EL, Yan SB. Recombinant human activated protein C for the postexposure treatment of Ebola hemorrhagic fever. J Infect Dis. 2007;196(suppl 2):S390–S399. doi: 10.1086/520598. [DOI] [PubMed] [Google Scholar]
- 20.Jahrling PB, Geisbert TW, Geisbert JB. Evaluation of immune globulin and recombinant interferon α-2b for treatment of experimental Ebola virus infections. J Infect Dis. 1999;179(suppl 1):S224–S234. doi: 10.1086/514310. [DOI] [PubMed] [Google Scholar]
- 21.Geisbert TW, Hensley LE, Jahrling PB. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: a study in rhesus monkeys. Lancet. 2003;362:1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- 22.Feldmann H, Jones SM, Daddario-Dicaprio KM. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Enterlein S, Warfield KL, Swenson DL. VP35 knockdown inhibits Ebola virus amplification and protects against lethal infection in mice. Antimicrob Agents Chemother. 2006;50:984–993. doi: 10.1128/AAC.50.3.984-993.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warfield KL, Swenson DL, Olinger GG. Gene-specific countermeasures against Ebola virus based on antisense phosphorodiamidate morpholino oligomers. PLoS Pathog. 2006;2:e1. doi: 10.1371/journal.ppat.0020001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins M, Judge A, Ambegia E. Misinterpreting the therapeutic effects of siRNA caused by immune stimulation. Hum Gene Ther. 2008;19:991–999. doi: 10.1089/hum.2008.131. [DOI] [PubMed] [Google Scholar]
- 26.Hornung V, Guenthner-Biller M, Bourquin C. Sequence-specific potent induction of IFN-alpha by short interfering RNA in plasmacytoid dendritic cells through TLR7. Nat Med. 2005;11:263–270. doi: 10.1038/nm1191. [DOI] [PubMed] [Google Scholar]
- 27.Judge AD, Sood V, Shaw JR, Fang D, McClintock K, MacLachlan I. Sequence-dependent stimulation of the mammalian innate immune response by synthetic siRNA. Nat Biotechnol. 2005;23:457–462. doi: 10.1038/nbt1081. [DOI] [PubMed] [Google Scholar]
- 28.Kortepeter MG, Martin JW, Rusnak JM. Managing potential laboratory exposure to Ebola virus by using a patient biocontainment care unit. Emerg Infect Dis. 2008;14:881–887. doi: 10.3201/eid1406.071489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.International Society for Infectious Diseases Ebolavirus, needlestick injury – Germany: (Hamburg) http://www.promedmail.org/pls/apex/f?p=2400:1001:::NO::F2400_P1001_BACK_PAGE,F2400_P1001_PUB_MAIL_ID:1000%2C76634 (accessed April 29, 2010).
- 30.International Society for Infectious Diseases Ebola, lab accident death – Russia (Siberia) http://www.promedmail.org/pls/apex/f?p=2400:1001:::NO::F2400_P1001_BACK_PAGE,F2400_P1001_PUB_MAIL_ID:1000%2C25465 (accessed April 29, 2010).