Abstract
Objective
We sought to identify factors associated with a successful trial of labor (TOL) following two cesarean deliveries (CDs) in a contemporary North American cohort.
Study Design
This is a retrospective cohort study of term, nonanomalous, singleton, vertex pregnancies attempting a vaginal birth after cesarean (VBAC) following a history of two previous CDs in the United States from 2012 to 2014. Maternal and intrapartum factors were analyzed using chi-square tests and multivariable logistic regression.
Results
A total of 22,762 women met the inclusion criteria and underwent TOL. Of these, 12,192 (53.6%) had a VBAC. Using multivariate logistic regression, previous vaginal delivery and delivery at 40 to 41 weeks’ gestation were associated with VBAC; maternal age, education, Medicaid insurance, non-Caucasian race/ethnicity, weight (overweight or obese), and gestational weight gain above the Institute of Medicine guidelines (adjusted odds ratio: 0.88; 95% confidence interval: 0.81–0.95) were associated with CD. Induction of labor did not affect the VBAC rate.
Conclusion
For those desiring a TOL after two previous CDs, prospective studies are needed to assess interventions that limit gestational weight gain as well as the safety and optimal timing of an induction of labor. The decision to attempt a TOL should be guided by counseling regarding the risks, benefits, and chances of a successful TOL.
Keywords: maternal and fetal morbidity, TOLAC, trial of labor after two cesareans, vaginal birth after cesarean, VBAC
A third of all births in the United States occur by caesarean delivery (CD), and these deliveries are a significant source of maternal and fetal morbidity.1–5 Although the peak incidence of CD was 32.9% in 2009, the frequency of CD continues to remain high at 32%in2015.2With each additional CD, there are increased maternal risks of placenta previa, accreta spectrum, unplanned hysterectomy, intraoperative injury, blood transfusion, and prolonged hospital stay.6,7 Thus, efforts to decrease the rate of CD, specifically in women with a previous history of CD, are vital. Since 1999, multiple clinical studies and cost-effectiveness analyses have addressed the safety and risks of a trial of labor after a single cesarean (TOLAC), with TOLAC as the preferred strategy compared with an elective repeat CD.8–10 Unfortunately, safety and liability concerns continue to limit access to TOLAC,11 with recent statewide surveys of TOLAC availability reporting a rate of 41 to 57%.12,13
A trial of labor (TOL) after one CD is a well-understood and accepted option, but offering a TOL to women with two prior CDs remains controversial. Thus, this highlights the need to better determine the risks and benefits of a TOL when undertaken by women who have had two prior CDs. The literature is largely limited to case reports and retrospective cohort studies underpowered to detect differences in rare outcomes, but they broadly report a rate of successful TOL after two prior CDs of 66 to 75% and a rate of uterine rupture of 0 to 3.7%.7,14–16 Based on these data, the American College of Obstetricians and Gynecologists states that “it is reasonable to consider women with two previous low transverse CD to be candidates for TOLAC” despite the limited data on the risks involved.11 Given the importance of thoroughly counseling patients eligible for a TOL after two CDs, we sought to identify predictors of a successful TOL following two CDs in a contemporary North American cohort.
Study Design
We performed a retrospective cohort study including all singleton, nonanomalous, vertex pregnancies at 36 to 43 weeks’ gestational age who attempted a vaginal delivery following a history of two previous CDs in the United States from 2012 to 2014. The data were derived from the United States Natality Public Use Files from the years of interest, including data on 11,899,735 deliveries. This dataset is a result of the Vital Statistics Cooperative Program, whereby the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) electronically receives data, from all 50 states, on all registered births to U.S. residents and nonresidents. The dataset includes information as well as birth certificate data including maternal medical information, method of delivery information (including previous number of CDs and TOLAC status), and other medical comorbidities. The dataset excluded patient privacy/identification information, and therefore no informed consent was required. This study was reviewed and considered exempt by the Institutional Review Board at the Oregon Health & Science University as it used publicly available data without patient identifiers.
Our population of interest was women with two prior CDs who underwent a TOL, and our primary outcome was failed TOL requiring a repeat CD. The maternal factors assessed included age (<35 years, >35 years), education, marital status, insurance carrier, cigarette use, and race/ethnicity (Caucasian, African-American, Asian, or Hispanic). Both prepregnancy maternal weight category (underweight body mass index [BMI] < 18.5, normal weight BMI 18.5–24.9, overweight BMI 25–29.9, obese > 30), and weight gain (below, within, and above the 2009 Institute of Medicine [IOM] guidelines for weight gain in pregnancy) were included, as well as a previous history of a vaginal delivery, maternal medical comorbidities (gestational diabetes, prepregnancy diabetes, gestational hypertension, chronic hypertension), induction of labor, and gestational age at delivery (by week).
Analyses were conducted using STATA (version 14, Stata-Corp, College Station, TX). Bivariate relationships between maternal/neonatal factors and the primary outcome were initially assessed using chi-square tests. Multivariable logistic regression models were used to control for confounding relationships. Adjusted odds ratios (aORs) were calculated for all outcomes of interest, and statistical significance was determined by p< 0.001 and/or 95% confidence intervals (CIs).
Results
Of the 11,899,735 deliveries included in the database, 320,809 (2.7%) women had a history of two previous CDs, and 22,762 (7%) were identified as meeting the study inclusion criteria (those with two previous CDs attempting a TOL), of whom 12,192 (53.6%) had a successful vaginal delivery following a TOL. For those undergoing a TOLAC, 5,530 (24.3%) were >35 years of age, 11,570 (51.4%) had Medicaid insurance, 6,320 (27.8%) were Caucasian, 2,802 were African-American (12.3%), 12,867 (56.5%) were Hispanic, 572 (2.5%) were Asian, and 7,185 (32.8%) were obese (►Table 1); there were 33 (0.14%) uterine ruptures in this group. In the unadjusted model, successful TOLAC rates were higher if women were married (56 vs. 49.1%; p< 0.001), had non-Medicaid insurance (56.5 vs. 50.8%; p< 0.001), were Caucasian or Hispanic (p< 0.001), were nonobese (p< 0.001), had weight gain below or within the IOM guidelines (p< 0.001), had a history of a previous vaginal delivery (58.9 vs. 47.6%; p< 0.001), were nondiabetic (53.9 vs. 49.3%; p< 0.001), and did not have gestational hypertension (53.9 vs. 44%; p< 0.001). Of note, 1,827 (9.6%) underwent an induction of labor, of whom 1,322 (57.6%) subsequently had a vaginal delivery.
Table 1.
Characteristics of women undergoing TOL after two previous cesareans (n = 22,762)
| Variable | Vaginal birth (%), n = 12,192 | Cesarean (%), n = 10,570 | p-Value |
|---|---|---|---|
| Maternal factors | |||
| Maternal age | |||
| < 35 years | 53.6 | 46.6 | 0.925 |
| > 35 years | 53.5 | 46.5 | |
| Education | |||
| No college | 52.4 | 47.6 | 0.003 |
| Some college | 54.4 | 45.6 | |
| Marital status | |||
| Not married | 49.1 | 50.9 | <0.001 |
| Married | 56 | 44 | |
| Insurance | |||
| Not Medicaid | 56.5 | 43.5 | <0.001 |
| Medicaid | 50.8 | 49.2 | |
| Cigarette smoker | |||
| No | 55 | 45 | 0.001 |
| Yes | 52.8 | 47.2 | |
| Maternal race/Ethnicity | |||
| Caucasian | 59 | 41 | <0.001 |
| African-American | 47.8 | 52.2 | |
| Hispanic | 52.5 | 47.5 | |
| Asian-American | 47.2 | 52.8 | |
| BMI | |||
| < 18.5 kg/m2 | 57.5 | 42.5 | <0.001 |
| 18.5–24.9 kg/m2 | 57.2 | 42.8 | |
| 25–29.9 kg/m2 | 52.5 | 47.5 | |
| > 30 kg/m2 | 49 | 51 | |
| Weight gain | |||
| Below IOM guidelines | 54.3 | 45.7 | <0.001 |
| Within IOM guidelines | 56.1 | 43.9 | |
| Above IOM guidelines | 51 | 49 | |
| Previous vaginal delivery | |||
| No | 47.6 | 52.4 | <0.001 |
| Yes | 58.9 | 41.1 | |
| Gestational diabetes | |||
| No | 50.8 | 49.2 | 0.149 |
| Yes | 50.1 | 49.9 | |
| Prepregnancy diabetes | |||
| No | 53.9 | 46.1 | <0.001 |
| Yes | 49.3 | 50.7 | |
| Gestational hypertension | |||
| No | 53.9 | 46.1 | <0.001 |
| Yes | 44 | 56 | |
| Chronic hypertension | |||
| No | 53.6 | 46.4 | 0.616 |
| Yes | 52.3 | 47.7 | |
| Induction of labor | |||
| No | 53.1 | 46.9 | <0.001 |
| Yes | 57.6 | 42.4 | |
| Gestational age (weeks) | <0.001 | ||
| 360/7–366/7 | 41.9 | 58.1 | |
| 370/7–376/7 | 45.6 | 54.4 | |
| 380/7–386/7 | 47.5 | 52.5 | |
| 390/7–396/7 | 50.6 | 49.4 | |
| 400/7–406/7 | 69.2 | 30.8 | |
| 410/7–416/7 | 66.4 | 33.6 | |
| 420/7–426/7 | 62.8 | 37.2 |
Abbreviations: BMI, body mass index; IOM, Institute of Medicine; TOL, trial of labor.
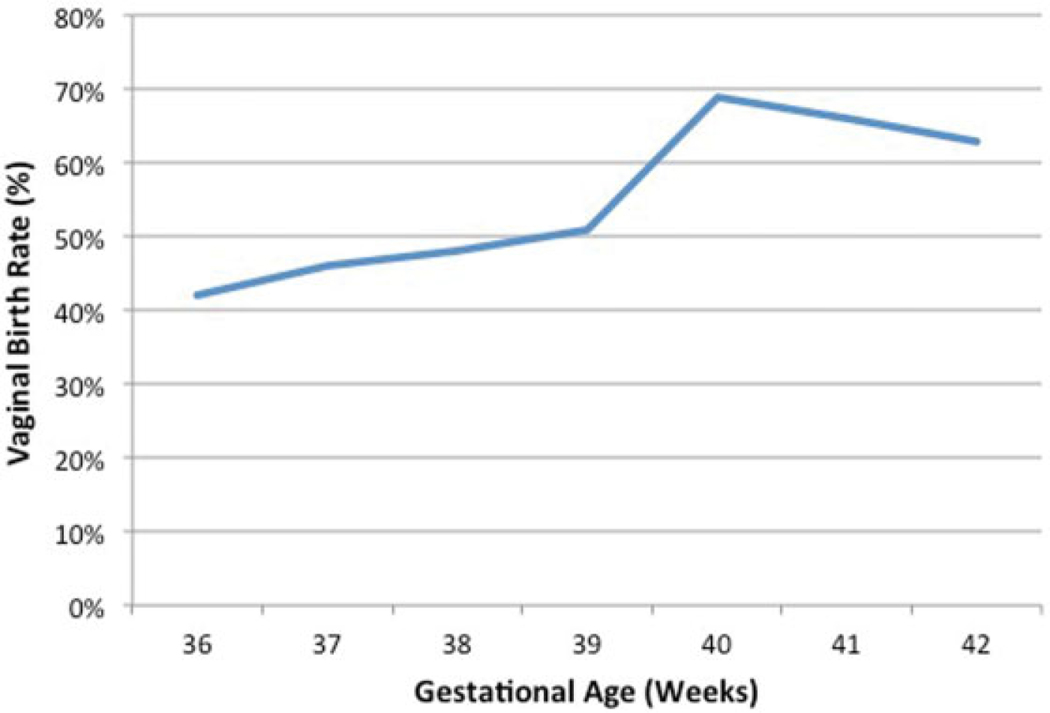
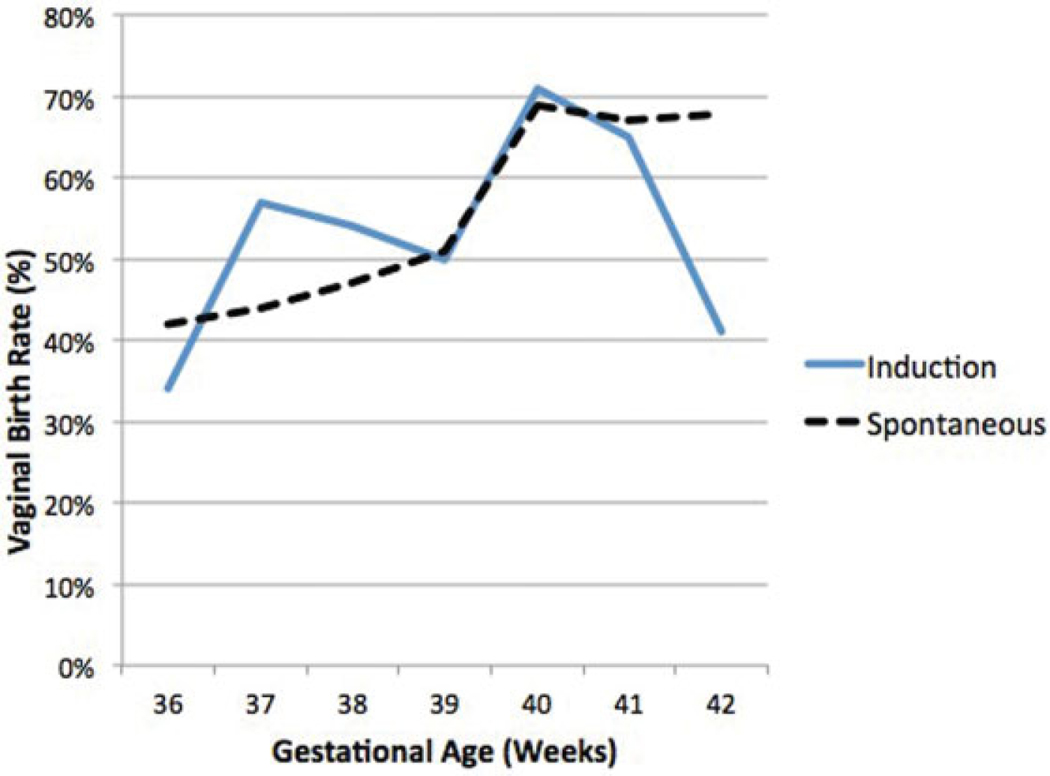
When examining rates of vaginal birth by gestational age (►Fig. 1), the rate of vaginal birth increased steadily after 36 weeks, peaked at 40 weeks (69.2%), and decreased thereafter. When the vaginal delivery rates by gestational age were divided between those with induced and those with spontaneous labor, there was a sharp decrease in the rate of vaginal birth after 41 weeks’ gestation in the induction group but not in the spontaneous labor group (►Fig. 2).
Fig. 1.
Vaginal birth rates by gestational age in women following a trial of labor after two previous cesarean deliveries.
Fig. 2.
Comparison of spontaneous versus induced labor vaginal birth rates by gestational age in women following a trial of labor after two previous cesarean deliveries.
When controlling for potential confounders using multivariable logistic regression, marital status, previous vaginal delivery, and delivery at 40 to 41 weeks’ gestation were associated with a successful vaginal birth (►Table 2). For example, prior vaginal delivery significantly increased the chances of vaginal birth after cesarean (VBAC) success with an aOR of 1.58 and a 95% CI of 1.47 to 1.70. Alternatively, maternal age, education, Medicaid insurance, non-Caucasian race/ethnicity, maternal weight (overweight or obese), gestational weight gain above the IOM guidelines (aOR: 0.88; 95% CI: 0.81–0.95), and delivery at less than 39 weeks’ gestational age were associated with CD.
Table 2.
Factors associated with vaginal birth following a trial of labor after two previous cesareans (n = 22,762)
| Factor | aORa | 95% CI | |
|---|---|---|---|
| Maternal factors | |||
| Age > 35 years | 0.88 | 0.81 | 0.96 |
| Some college education | 0.85 | 0.79 | 0.92 |
| Married | 1.13 | 1.04 | 1.23 |
| Medicaid insurance | 0.91 | 0.84 | 0.99 |
| Cigarette smokerb | – | – | – |
| Maternal race/Ethnicityc | |||
| African-American | 0.68 | 0.62 | 0.76 |
| Hispanic | 0.64 | 0.58 | 0.70 |
| Asian-American | 0.59 | 0.49 | 0.71 |
| Weight categoryd | |||
| Underweight | 1.04 | 0.80 | 1.35 |
| Overweight | 0.87 | 0.79 | 0.95 |
| Obese | 0.75 | 0.68 | 0.82 |
| Weight gaine | |||
| Below IOM guidelines | 1.10 | 0.99 | 1.21 |
| Above IOM guidelines | 0.88 | 0.81 | 0.95 |
| Previous vaginal delivery | 1.58 | 1.47 | 1.70 |
| Gestational diabetesb | – | – | – |
| Pre-pregnancy diabetes | 0.98 | 0.85 | 1.12 |
| Gestational hypertension | 0.84 | 0.69 | 1.03 |
| Chronic hypertension | 1.13 | 0.84 | 1.52 |
| Induction of labor | 1.08 | 0.96 | 1.22 |
| Gestational age (weeks)f | |||
| 360/7–366/7 | 0.64 | 0.54 | 0.76 |
| 370/7–376/7 | 0.79 | 0.70 | 0.89 |
| 380/7–386/7 | 0.85 | 0.78 | 0.94 |
| 400/7–406/7 | 2.01 | 1.80 | 2.26 |
| 410/7–416/7 | 1.66 | 1.39 | 1.98 |
| > 420/7 | 1.32 | 0.87 | 1.99 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; IOM, Institute of Medicine.
Model adjusted for maternal age, college education, Medicaid insurance, cigarette smoking, gestational age, maternal race, maternal weight gain, gestational diabetes, prepregnancy diabetes, gestational hypertension, chronic hypertension, induction of labor, and previous vaginal delivery.
Omitted due to collinearity.
Comparison group: Caucasian.
Comparison group: normal weight.
Comparison group: within IOM Guidelines.
Comparison group: weeks 390/7–396/7.
In an analysis of vaginal birth rates by prepregnancy weight category stratified by weight gain during pregnancy, for overweight and obese women, there was a significant decrease in the VBAC rate, with progressive increases in weight gain through pregnancy (►Table 3). For overweight and obese women who gained less weight than the IOM recommends, the chances of successful VBAC were 56.9 and 52.7%, respectively; these rates decreased stepwise with increasing weight gain to a VBAC rate of 51.3 and 47.4%, respectively, for women who gained more weight than the IOM recommendations.
Table 3.
Chance of vaginal birth by weight category and gestational weight gain for women attempting a trial of labor after two previous cesareans (n = 22,762)
| Weight category weight gain | Vaginal birth (%), n = 12,192 | |
|---|---|---|
| Underweight | Below IOM guidelines | 62.4 |
| Within IOM guidelines | 52.1 | |
| Above IOM guidelines | 59.4 | |
| Normal weight | Below IOM guidelines | 57.8 |
| Within IOM guidelines | 58.7 | |
| Above IOM guidelines | 55 | |
| Overweight | Below IOM guidelines | 56.9 |
| Within IOM guidelines | 52.6 | |
| Above IOM guidelines | 51.3a | |
| Obese | Below IOM guidelines | 52.7 |
| Within IOM guidelines | 49 | |
| Above IOM guidelines | 47.4a | |
Abbreviation: IOM, Institute of Medicine.
Within group differences based on gestational weight gain (p < 0.01).
Conclusion
A TOLAC, when offered appropriately, remains a powerful approach to improve birth outcomes,2,9,10 but safety and liability concerns continue to limit TOLAC availability. 11–13,17 As of 2015, 18% of women with two or more children expect to become pregnant again,18 and contemporary data regarding a TOL after two CDs are necessary for providers to facilitate patient counseling regarding options for the mode of delivery. In this large retrospective national cohort, we sought to identify factors associated with a successful vaginal delivery after two prior CDs.
In our study, we found that the overall chance of a successful TOL after two prior CDs was 53.6%. Several nonmodifiable factors were found to be associated with a failed TOL, including maternal age, education, Medicaid insurance, and race/ethnicity (non-Caucasian). Interestingly, prepregnancy weight (overweight/obese) was associated with a failed TOL, suggesting the importance of preconception medical optimization. As previously described,19 a history of previous vaginal deliverywas associatedwith an increased rate of vaginal birth.We found that the modifiable factors of maternal weight gain and delivery at 40 to 41 weeks’ gestational age were associated with an increased likelihood of successful vaginal delivery. Induction of labor did not affect the rate of vaginal birth. Importantly, we noted that increasing maternal weight and excessive maternal weight gain were associated with stepwise increases in the rates of CD. Additionally, for obese and overweight women, the highest rates of vaginal birth were attained bywomenwhose weight gain was below the IOM guidelines. These findings clearly warrant future studies investigating the relationship between prepregnancy weight and gestational weight gain on TOL success.
Our findings highlight the clinical dilemma of the term patient who desires a TOL after two previous CDs. Although induction of labor was not associated with an overall increase in vaginal delivery success, the rate of vaginal delivery decreased precipitously in women induced after 41 weeks’ gestation. Two recent large retrospective trials analyzed the impact of induction of labor versus expectant management for women undergoing a TOL following one previous CD20,21 and found contradictory associations between induction and successful TOLAC. While Palatnik and Grobman found that induction increased the likelihood of vaginal birth at 39 weeks’ gestation but not at 40 and 41 weeks,20 Lappen et al found induction of labor to be associated with an increase in CD from 37 to 40 weeks’ gestation.21 Given that our study compared induction with spontaneous labor (as opposed to expectant management),which possibly biased our results against induction, a finding of no difference is certainly reassuring that induction should not be specifically avoided in such patients. Future prospective studies delineating the impact of induction of labor are warranted.
The rate of successful VBAC was lower in our cohort than that previously reported. It is possible that our data include women who had initially intended on a repeat CD, subsequently underwent spontaneous labor with delivery by repeat CD, and were coded as a TOL. This misclassification would lead to lower rates of a successful TOL, potentially explaining our lower observed rate of successful TOL after two CDs (53.6%) than was previously reported (66–75%).7,11,14–16,22 Alternatively, our data includes all births in the United States, which may be more representative, as opposed to existing studies that are primarily from academic centers that may have led to lower success rates. A prospective study of the indication for failed TOL may help to elucidate this difference.
The strength of this study lies in the large, diverse contemporary population analyzed. However, as with any retrospective cohort study using administrative data, our study has potential methodological limitations. Data regarding maternal socioeconomic status and drug/alcohol use were unavailable (alcohol use has been excluded from the publically available dataset since 2007); additionally, few maternal medical comorbidities were included in the dataset, limiting our ability to risk-stratify this analysis. In this dataset, births to nonresidents of the United States are excluded from the analysis, although it is unlikely that this would impact our results or conclusions meaningfully. Importantly, information about intrapartum details, such as cervical dilation upon presentation, indications for induction of labor, duration of labor, or specific labor management protocols, was unavailable in our dataset.
In summary, in this large contemporary analysis, we found several important modifiable factors associated with a successful TOL for women with a history of two previous CDs. Prepregnancy weight control, close attention to gestational weight gain, and delivery between 40 and 41 weeks’ gestational age may be an important means to optimize a woman’s chance for a successful TOL. The decision to attempt an induction of labor must be made thoughtfully after thorough counseling and induction of labor prior to 41 weeks’ gestation may improve the chances of TOL success. It is important that clinicians identify a patient’s nonmodifiable factors and focus on improving modifiable factors such as gestational weight gain and delivery timing to improve the likelihood of a successful vaginal delivery. If a TOL after two prior CDs is attempted, it is necessary to labor at a tertiary care center with obstetric, anesthesia, and transfusion services immediately available. Prospective studies are needed to further refine proper patient selection for a TOL after two prior CDs and to define the safety and optimal timing of induction.
Footnotes
This study was presented as a poster presentation at the 37th Annual Meeting of the Society for Maternal-Fetal Medicine, Las Vegas, NV, January 27, 2017.
Conflict of Interest
None.
References
- 1.Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Matthews TJ. Births: final data for 2014. Natl Vital Stat Rep 2015;64(12):1–64 [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Mathews TJ. Births: final data for 2015. Natl Vital Stat Rep 2017;66(01):1. [PubMed] [Google Scholar]
- 3.Lydon-Rochelle MT, Cahill AG, Spong CY. Birth after previous cesarean delivery: short-term maternal outcomes. Semin Perinatol 2010;34(04):249–257 [DOI] [PubMed] [Google Scholar]
- 4.Silver RM. Delivery after previous cesarean: long-term maternal outcomes. Semin Perinatol 2010;34(04):258–266 [DOI] [PubMed] [Google Scholar]
- 5.Guise J-M, Eden K, Emeis C, et al. Vaginal Birth after Cesarean: New Insights. Evidence report/technology assessment no. 191 (prepared by the Oregon Health & Science University Evidence-based Practice Center under Contract No. 290–2007–10057-I). AHRQ Publication No. 10–E003. Rockville, MD: Agency for Health-care Research and Quality; 2010 [Google Scholar]
- 6.Silver RM, Landon MB, Rouse DJ, et al. ; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006;107(06): 1226–1232 [DOI] [PubMed] [Google Scholar]
- 7.Cahill AG, Tuuli M, Odibo AO, Stamilio DM, Macones GA. Vaginal birth after caesarean for women with three or more prior caesareans: assessing safety and success. BJOG 2010;117(04):422–427 [DOI] [PubMed] [Google Scholar]
- 8.Sadan O, Leshno M, Gottreich A, Golan A, Lurie S. Once a cesarean always a cesarean? A computer-assisted decision analysis. Arch Gynecol Obstet 2007;276(05):517–521 [DOI] [PubMed] [Google Scholar]
- 9.Gilbert SA, Grobman WA, Landon MB, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Cost-effectiveness of trial of labor after previous cesarean in a minimally biased cohort. Am J Perinatol 2013;30(01):11–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wymen KM, SXhih YC, Plunkett BA. The cost-effectiveness of a trial of labor accrues with multiple subsequent vaginal deliveries. Am J Obstet Gynecol 2014;211(01):56.e1–56.e12 [DOI] [PubMed] [Google Scholar]
- 11.American College of Obstetricians and Gynecologists: Practice Bulletin 115 Vaginal Birth after Previous Cesarean Delivery. Washington, DC: ACOG; 2010. (reaffirmed 2015) [Google Scholar]
- 12.Barger MK, Dunn JT, Bearman S, DeLain M, Gates E. A survey of access to trial of labor in California hospitals in 2012. BMC Pregnancy Childbirth 2013;13:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leeman LM, Beagle M, Espey E, Ogburn T, Skipper B. Diminishing availability of trial of labor after cesarean delivery in New Mexico hospitals. Obstet Gynecol 2013;122(2 Pt 1):242–247 [DOI] [PubMed] [Google Scholar]
- 14.Tahseen S, Griffiths M. Vaginal birth after two caesarean sections (VBAC-2)-a systematic review with meta-analysis of success rate and adverse outcomes of VBAC-2 versus VBAC-1 and repeat (third) caesarean sections. BJOG 2010;117(01):5–19 [DOI] [PubMed] [Google Scholar]
- 15.Yaman Tunc S, Agacayak E, Sak S, et al. Multiple repeat caesarean deliveries: do they increase maternal and neonatal morbidity? J Matern Fetal Neonatal Med 2017;30(06):739–744 [DOI] [PubMed] [Google Scholar]
- 16.Metz TD, Allshouse AA, Faucett AM, Grobman WA. Validation of a vaginal birth after caesarean delivery prediction model in women with two prior caesarean deliveries. Obstet Gynecol 2015;125(04):948–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonanno C, Clausing M, Berkowitz R. VBAC: a medicolegal perspective. Clin Perinatol 2011;38(02):217–225 [DOI] [PubMed] [Google Scholar]
- 18.Daugherty J, Martinez G. Birth expectations of US women aged 15–44. NCHS Data Brief 2016;(260):1–8 [PubMed] [Google Scholar]
- 19.Hendler I, Bujold E. Effect of prior vaginal delivery or prior vaginal birth after cesarean delivery on obstetric outcomes in women undergoing trial of labor. Obstet Gynecol 2004;104(02):273–277 [DOI] [PubMed] [Google Scholar]
- 20.Palatnik A, Grobman WA. Induction of labor versus expectant management for women with a prior cesarean delivery. Am J Obstet Gynecol 2015;212(03):358.e1–358.e6 [DOI] [PubMed] [Google Scholar]
- 21.Lappen JR, Hackney DN, Bailit JL. Out comes of term induction in trial of labor after cesarean delivery. Obstet Gynecol 2015;126(01):115–123 [DOI] [PubMed] [Google Scholar]
- 22.Macones GA, Cahill A, Pare E, et al. Obstetric outcomes in women with two prior cesarean deliveries: is vaginal birth after cesarean delivery a viable option? Am J Obstet Gynecol 2005;192(04):1223–1228 [DOI] [PubMed] [Google Scholar]