Abstract
Intraosseous lipomas are rare primary benign bone tumors which present with highly nonspecific radiographic features that may lead to equivocal diagnoses. Advanced imaging studies such as MRI with and without contrast and, in some selected cases, tissue sample analyses are required in the diagnostic pathway. Here we describe the second case in the literature of an intraosseous lipoma of the clavicle and the first with extraosseous extension. Subsequent to histologic confirmation the lesion was monitored with clinical and radiologic evaluation.
Keywords: Intraosseous lipoma, Clavicle, Bone primary tumor
Introduction
Intraosseous lipomas are among the rarest primary bone tumors, with an incidence of 0.1% [1]. While the etiology is not clear, these tumors are considered benign and consist of mature adipose tissue within the intramedullary cavity of normal bones [2]. The most frequent age of presentation is between the 4th and 5th decade [3]. Several studies disagree regarding gender distribution, some claiming an equal gender occurrence while others state a slight male predominance [3], [4], [5]. Intraosseous lipomas more commonly occur in the metaphysis of long bones, such as the femur, tibia or fibula, and in the calcaneus [6,7]. The majority of the intraosseous lipomas are asymptomatic or present with minimal symptoms such as localized or referred mild pain, thus the diagnosis is made as an incidental finding in a patient undergoing imaging studies for other motives [4,8]. On radiographic studies these tumors have nonspecific imaging features, thus posing several differential diagnostic possibilities such as fibrous dysplasia, enchondromas, bone infarct, chondrosarcoma, among others [9,10].
We report the case of an intraosseous lipoma of the clavicle that subsequent to histological confirmation was managed with observation. To the best of our knowledge this is the second case to be described in this location in the literature and the first to describe extraosseous extension in a clavicle [11].
Case report
A 59-year-old female with a history of rheumatoid arthritis (RA) presented to our Sarcoma Clinic for a second opinion on a lesion in her left clavicle. The lesion was found incidentally on imaging studies done for evaluation of her RA. Six months prior to presentation (February 2017), the patient underwent a positron emission tomography/computed tomography (PET/CT) scan to investigate a nodule in her lung. In this exam a lack of cortex in the anteroinferior portion of the left clavicle was found, however no concerning associated soft tissue mass was observed nor was there any increased uptake in this region (Fig. 1). Four months after (June 2017), a series of radiographic studies of the left clavicle were obtained (Fig. 2). The lesion was described as lucent lesion with an IA border and with a small area protruding outside of the bone in the inferior aspect of the clavicle [12]; there was a suspicion that this could represent an area of soft tissue proliferation. A decision was made to obtain a magnetic resonance imaging (MRI) study with and without Gadolinium contrast (July 2017). The study depicted a well-defined lesion in the left clavicle extending into adjacent soft tissue with features of a benign lipoma – T1 hyperintensity, hypointense under fat suppression, and relatively small in size (2.6 × 1.4 cm). However, faint enhancement under contrast and potential nodularity within the lesion warranted further evaluation to rule out an atypical lipomatous tumor and a surgical resection was recommended (Fig. 3). The patient opted for a second opinion at our center regarding treatment alternatives (August 2017). At presentation to our clinic the patient stated that she had no recent history of fever, chills, night sweats, weight loss, or other constitutional symptoms. Although she complained of swelling and pain in her hands and feet during the morning, this was thought to be associated to her RA history. She denied pain in her left clavicle and had no history of trauma to the area. No masses were appreciated over the left clavicle and the remainder of the physical exam was within normal limits.
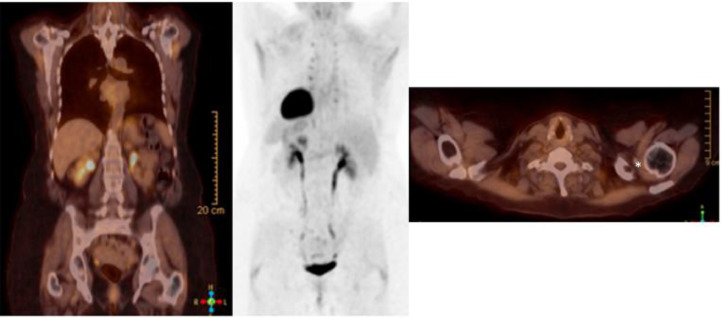
Fig. 1.
Positron emission tomography/computed tomography (PET/CT) scan (February 2017) depicting a defect in the anteroinferior left clavicle lateral cortex (*) without any abnormal uptake.
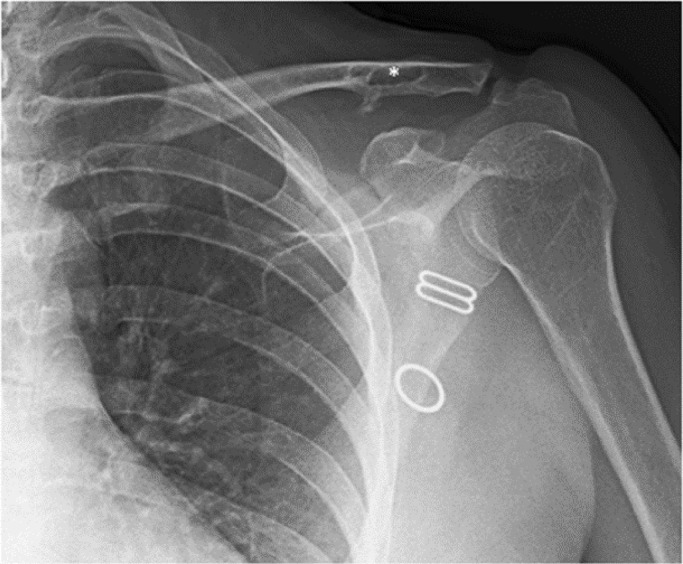
Fig. 2.
Radiographic image of the left clavicle (June 2017) showing a geographic lucent lesion (*) with a sclerotic border and extraosseous extension.
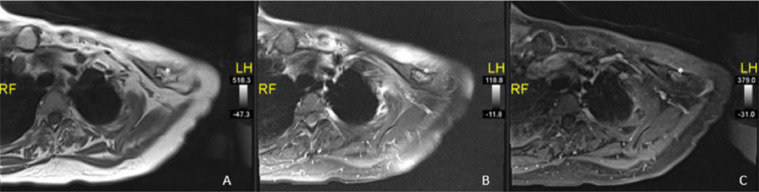
Fig. 3.
Magnetic resonance imaging (MRI) of the left clavicle (July 2017), axial plane cuts in T1-weighted sequence (A), STIR sequence (B) and T1 fat suppressed with gadolinium contrast (C), showing the intraosseous lesion (black and white arrows) in the distal end of the clavicle well demarcated, without surrounding edema and with no enhancement.
During the Sarcoma Tumor Board our team decided that, even though we believed the nodularity could likely be due to cortical bone extending from the clavicle into the lipomatous component, making a simple intraosseous lipoma with bone disruption and soft tissue expansion much more likely, the next best step was to perform a bone scintigraphy and a CT-guide core needle biopsy prior to considering definitive treatment. The bone scan failed to find any uptake in the left clavicle and the biopsy was performed without complication (Fig. 4). Histopathological analysis of the specimen revealed normal-appearing mature adipocytes set in fibrocollagenous connective tissue with normal blood and bone (Fig. 5). No evidence of malignancy was appreciated in both histology and cytology with Touch Prep. At this point we determined that the patient's clavicular lesion was a benign intraosseous lipoma of the clavicle and we recommended surveillance as the appropriate long-term course of action.
Fig. 4.
Total body bone scintigraphy with Tc99 (August 2017), depicting lack of abnormal uptake in the left clavicle's distal end.
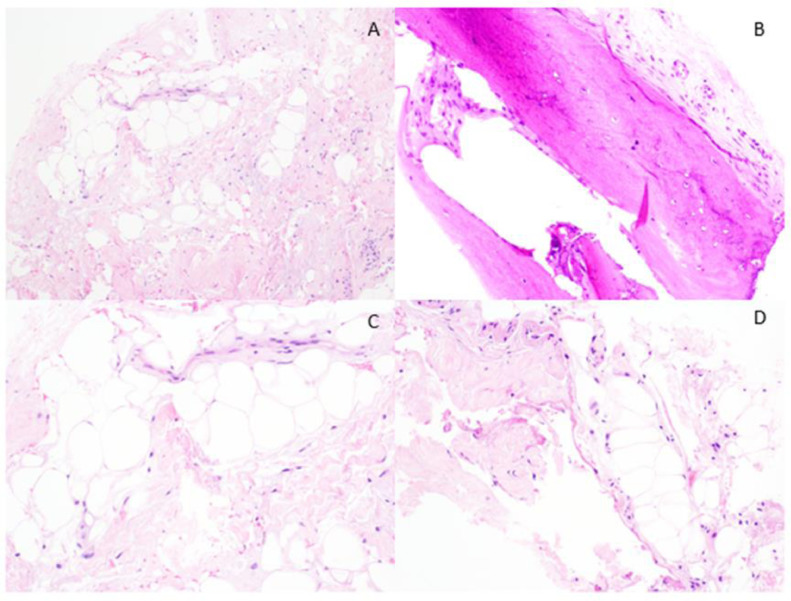
Fig. 5.
Histopathological analysis of the left distal clavicle biopsy (August 2017). (A) Low power view of normal mature adipocytes within fibrocollagenous connective tissue (H&E, 10×), (B) Normal trabecular bone with adjacent connective tissue (H&E, 10×), (C) Normal mature adipocytes within fibrocollagenous tissue (H&E, 20×), (D) Mature adipocytes and fibrocollagenous tissue (H&E, 20×).
At her 8 months follow-up after the biopsy (April 2018) a radiograph and an MRI study with and without gadolinium contrast demonstrated an unchanged lesion when compared to initial imaging studies, and the patient did not report any pain in her clavicle or any constitutional symptoms (Fig. 6).
Fig. 6.
Magnetic resonance imaging (MRI) of the left clavicle (April 2018), axial plane cuts in T1-weighted sequence (A), STIR sequence (B) and T1 fat suppressed with gadolinium contrast (C), showing the intraosseous lesion (*) has remained unchanged over time. The lesion (*) continues to be well demarcated, without surrounding edema, with no enhancement and no changes in size.
Currently, almost 2 years since the initial imaging studies showed the lesion (June 2019), radiographs continue to show an unchanged intraosseous lipoma (Fig. 7). The patient remains symptom-free.
Fig. 7.
Radiographic image of the left clavicle (June 2019), 2 years after the initial radiograph, showing a geographic lucent lesion (*) with a sclerotic border and extraosseous extension that has remained stable over time.
Discussion
In the case presented, as in the majority of intraosseous lipomas, the finding of the lesion was incidental. Most of the patients present with no or mild associated pain to the lesion itself, though many do have pain from different sources such as osteoarthritis or an underlying rheumatological condition [4,13]. In previous reports a myriad of diverse symptoms has been described such as minor aching, a palpable mass and even a pathological fracture [3,7]. In this setting it is important to determine the real source of the pain in order to determine the appropriate treatment.
On radiographic images these tumors present as a lytic lesion expanding the bone and well-defined borders, more rarely septations, calcification or ill-defined margins can be identified as well [10,[13], [14], [15]. The tumor is most often located in the metaphysis of long bones; diaphyseal extension has been described but epiphyseal involvement is infrequent [16,17]. In most cases these findings are not specific to be diagnostic; except in the calcaneus where a partially cystic lesion with sclerotic margins and a central calcification is considered pathognomonic of this tumor [16,18].
Due to the nondiagnostic radiographic features which entails numerous differential diagnoses advanced imaging studies such as CT and/or MRI with and without contrast are required for a radiologic diagnosis. In CT studies intraosseous lipomas can be visualized as lucent lesions with marked borders and with the same density as normal fat. Trabecular resorption, bone expansion and calcifications within the lesion are also common features [19]. Under MRI this tumor has the radiologic features of a benign fatty tumor, hyperintense in T1- and T2-weighted sequences [14]. In fat suppressed sequences it remains isointense to subcutaneous fat [16]. Bone expansion and trabecular resorption are also visualized on MRI studies. Areas of necrosis or cystic degeneration present within the tumor will present with high intensity in T2-weighted sequences, while calcifications within the lesion will be hypointense in T2-weighted sequences and will show no enhancement in post contrast sequences [20].
At gross examination intraosseous lipomas are bright yellow and soft in consistency with variable amounts of fat necrosis, sclerotic bone and dystrophic calcification [5]. Bone trabeculae are occasionally seen inside the lesion, which are very fragile and fracture easily when manipulated [4]. On histologic exam mature adipocytes are observed with no atypia or increased frequency of mitoses, while surrounding the lesion normal cortical bone is also visualized [3]. When the tumor undergoes involutional changes fat necrosis, calcifications and intralesional cysts can also be found [4]. Based on the presence or absence of such findings, occurring as part of the natural involution these tumors undergo, Milgram described and classified the lesion in 3 stages [4]. In the first stage the tumor consists of viable mature fat cells similar to normal subcutaneous fat. In the following stage, showing intermediate grades of involution, infarction and necrotic areas are observed within the tumor, foamy macrophages and reactive bone formations are also noted. Continuing with the involutional changes, in stage III, the tumor is completely necrotic with occasional calcifications and cystic formations [4].
Intraosseous lipomas have an excellent prognosis with no recurrences described following curettage and grafting of the lesion [6,7]. Complete involution during observation has also been reported [20,5]. These tumors are considered benign in nature and in addition patients are usually asymptomatic. These facts have prompted other authors to propose clinical and radiological observation as the only required treatment [5,21]. Four cases have been described where a malignant transformation into a malignant histiocytic fibroma occurred and even though this appears to be an extremely rare event, a rapidly increasing osseous lytic process should warrant a more aggressive approach [22].
Conclusion
Intraosseous lipomas are uncommon primary bone tumors and even though they can potentially occur in any bone, some locations such as the clavicle are particularly rare and even more rare with cortical breakthrough and extraosseous involvement. These tumors present with highly unspecific imaging features that may lead to equivocal diagnoses. In this misleading scenario advanced imaging studies such as MRI with and without contrast and potentially, in some selected cases, a tissue sample analysis is encouraged especially in the setting of extraosseous involvement.
Contributor Information
Ana C. Belzarena, Email: ceciliabel@baptisthealth.net.
Lucas Paul Paladino, Email: lpp@health.usf.edu.
Evita Henderson-Jackson, Email: evita.henderson@moffitt.org.
David M. Joyce, Email: david.joyce@moffitt.org.
References
- 1.Rosenberg AE, Bridge JA. Lipoma of bone. In: Fletcher CM, Uni KK, Mertens F, editors. WHO classification of tumors: pathology and genetics of tumors of soft tissue and bone. Lyon7 IARC Press; 2002. pp. 328–329. [Google Scholar]
- 2.Chow LT, Lee KC. Intraosseous lipoma: a clinicopathologic study of nine cases. Am J Surg Pathol. 1992;16:401–410. [PubMed] [Google Scholar]
- 3.Campbell RS, Grainger AJ, Mangham DC, Beggs I, Teh J, Davies AM. Intraosseous lipoma: report of 35 new cases and a review of the literature. Skeletal Radiol. 2003;32:209–222. doi: 10.1007/s00256-002-0616-7. [DOI] [PubMed] [Google Scholar]
- 4.Milgram JW. Intraosseous lipomas: a clinicopathologic study of 66 cases. Clin Orthop. 1988;231:277–302. [PubMed] [Google Scholar]
- 5.Goto T, Kojima T, Iijima T, Yokokura S, Motoi T, Kawano H. Intraosseous lipoma: a clinical study of 12 patients. J Orthop Sci. 2002;7:274–280. doi: 10.1007/s007760200046. [DOI] [PubMed] [Google Scholar]
- 6.Radl R, Leithner A, Machacek F, Cetin E, Koehler W, Koppany B. Intraosseous lipoma: retrospective analysis of 29 patients. Int Orthopaed. 2004;18:374–378. doi: 10.1007/s00264-004-0586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang HS, Kim T, Oh S, Park S, Chung SH. Intraosseous lipoma: 18 years of experience at a single institution. Clin Orthoped Surg. 2018;10(2):234–239. doi: 10.4055/cios.2018.10.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palczewski P, Swiątkowski J, Gołębiowski M, Błasińska-Przerwa K. Intraosseous lipomas: a report of six cases and a review of literature. Pol J Radiol. 2011;76(4):52–59. [PMC free article] [PubMed] [Google Scholar]
- 9.Eyzaguirre E, Liqiang W, Karla GM, Rajendra K, Alberto A, Gatalica Z. Intraosseous lipoma: a clinical, radiologic, and pathologic study of 5 cases. Ann Diagn Pathol. 2007;11(5):320–325. doi: 10.1016/j.anndiagpath.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Ö Öztekin, M Argin, Oktay A, Arkun R. Intraosseous lipoma: radiological findings. Radiol Brasileira. 2008;41(2):81–86. [Google Scholar]
- 11.Read RF. Subperiosteal or intra-osseous lipoma of the clavicle. The Lancet. 1955;266(6889):564. [Google Scholar]
- 12.Caracciolo JT, Temple HT, Letson G., Kransdorf MJ. A modified Lodwick-Madewell grading system for the evaluation of lytic bone lesions. Am J Roentgenol. 2016;207(1):150–156. doi: 10.2214/AJR.15.14368. [DOI] [PubMed] [Google Scholar]
- 13.Mandl P, Mester A, Balint PV. A black hole in a bone — intraosseous lipoma. J Rheumatol. 2009;36(2):434–436. doi: 10.3899/jrheum.080731. [DOI] [PubMed] [Google Scholar]
- 14.Blacksin MF, Ende N, Benevenia J. Magnetic resonance imaging of intraosseous lipomas: a radiologic-pathologic correlation. Skeletal Radiology. 1995;24(1):37–41. doi: 10.1007/BF02425945. [DOI] [PubMed] [Google Scholar]
- 15.Czerniak B, Dorfman HD. 2nd ed. Elsevier; Philadelphia, PA: 2016. Dorfman and Czerniaks bone tumors. [Google Scholar]
- 16.Murphey MD, Kransdorf MJ. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. RadioGraphics. 2004;24(5):1433–1466. doi: 10.1148/rg.245045120. [DOI] [PubMed] [Google Scholar]
- 17.Yamamoto T, Akisue T, Marui T, Nagira K, Yoshiya S, Kurosaka M. Intraosseous lipoma of the humeral head. Clin Imaging. 2001;25(6):428–431. doi: 10.1016/s0899-7071(01)00337-0. [DOI] [PubMed] [Google Scholar]
- 18.Ramos A, Castellano J, Sartoris DJ. Osseous lipoma: CT appearance. Radiology. 1985;157:615–619. doi: 10.1148/radiology.157.3.4059548. [DOI] [PubMed] [Google Scholar]
- 19.Propeck T, Bullard MA, Lin J, Doi K, Martel W. Radiologic-pathologic correlation of intraosseous lipomas. AJR Am J Roentgenol. 2000;175(3):673–678. doi: 10.2214/ajr.175.3.1750673. [DOI] [PubMed] [Google Scholar]
- 20.Mannem RR, Mautz AP, Baynes KE, Zambrano EV, King DM. AIRP best cases in radiologic-pathologic correlation: intraosseous lipoma. RadioGraphics. 2012;32(5):1523–1528. doi: 10.1148/rg.325115031. [DOI] [PubMed] [Google Scholar]
- 21.Bagatur AE, Yalcinkaya M, Dogan A, Gur S, Mumcuoglu E, Albayrak M. Surgery is not always necessary in intraosseous lipoma. Orthopedics. 2010;33(5) doi: 10.3928/01477447-20100329-13. [DOI] [PubMed] [Google Scholar]
- 22.Milgram JW. Malignant transformation in bone lipomas. Skeletal Radiol. 1990;19(5):347–352. doi: 10.1007/BF00193088. [DOI] [PubMed] [Google Scholar]