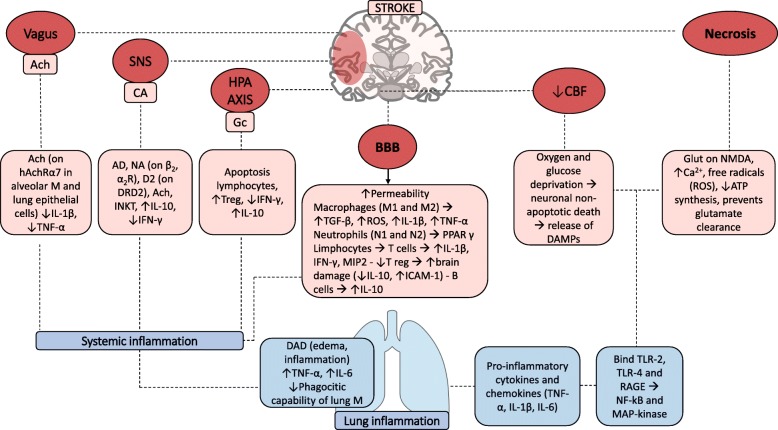
Fig. 1.
Inflammatory cascade after acute ischemic stroke. This figure represents the complex inflammatory cascade activated after acute ischemic stroke. Vagus efferences, sympathetic nervous system and hypothalamic-pituitary axis enhance immunosuppression by releasing Ach, catecholamine, and glucocorticoids, respectively. These molecules bind their specific receptors (nAchRα7 for Ach; β2, α2, and D2 for catecholamines) inducing apoptosis of lymphocytes, increasing the release of IL-10, and decreasing the release of IFN-γ, TNF-α, and IL-1β. At the same time, the reduction of cerebral blood flow caused by vessel’s ischemia determines oxygen and glucose deprivation with consequent neuronal and glial death and release of DAMPs. DAMPs include glutamate, ATP, and ROS and bind TLR-2, TLR-4, and RAGE thus inducing NF-kB and MAP kinase activation. Moreover, the blood-brain barrier damage with increased permeability yields immune cell translocation and enhanced inflammatory response. The peripheral effect on the lung includes diffuse alveolar damage with edema and inflammation and increases TNF-α and IL-6 levels, also reducing phagocytic capability of macrophages. Ach, acetylcholine; SNS, sympathetic nervous system; HPA, hypothalamic-pituitary-adrenal axis; BBB, blood-brain barrier; CBF, cerebral blood flow; M, macrophages; IL, interleukin; Gc, glucocorticoids; TNF, tumor necrosis factor; Treg, T regulator; IFN, interferon; TGF, transforming growth factor; ROS, radicals of oxygen; PPAR, peroxisome proliferator-activated receptor; MIP, macrophage inflammatory protein; ICAM, intracellular adhesion molecule; DAMPS, damage-associated molecular patterns; ATP, adenosine triphosphate; TLR, toll-like receptor; DAD, diffuse alveolar damage; RAGE, advanced glycation end products, DRD2, dopamine receptor D2; INKT, invariant natural killer