Abstract
Ataxia is a neurodegenerative syndrome, which can emerge as a major element of a disease or represent a symptom of more complex multisystemic disorders. It comprises several forms with a highly variegated etiology, mainly united by motor, balance, and speech impairments and, at the tissue level, by cerebellar atrophy and Purkinje cells degeneration. For this reason, the contribution of astrocytes to this disease has been largely overlooked in the past. Nevertheless, in the last few decades, growing evidences are pointing to cerebellar astrocytes as crucial players not only in the progression but also in the onset of distinct forms of ataxia. Although the current knowledge on this topic is very fragmentary and ataxia type-specific, the present review will attempt to provide a comprehensive view of astrocytes’ involvement across the distinct forms of this pathology. Here, it will be highlighted how, through consecutive stage-specific mechanisms, astrocytes can lead to non-cell autonomous neurodegeneration and, consequently, to the behavioral impairments typical of this disease. In light of that, treating astrocytes to heal neurons will be discussed as a potential complementary therapeutic approach for ataxic patients, a crucial point provided the absence of conclusive treatments for this disease.
Keywords: cerebellum, ataxia, astrocytes, neurodegeneration, glia
1. Introduction
The role of the cerebellum in motor function is well recognized and results from an intricate circuitry through which this brain area gets connected with the basal ganglia and the cerebral cortex, as well as with peripheral motor and sensory pathways [1]. Malfunctions of any part of this circuitry result in imbalance and incoordination of posture and limbs, a disorder commonly known as ataxia and, specifically, as cerebellar ataxia in case of a cerebellar origin [2,3]. Nevertheless, besides motor alterations, ataxia has a very heterogeneous clinical presentation, comprising ocular impairments such as eye fixation deficits and nystagmus, and cognitive impairments with variable degrees of severity. This is due to the functional anatomy of the cerebellum, according to which distinct lobules in both the vermis and hemispheres are connected with distinct brain areas and are involved in diverse motor and non-motor functions [4]. Based on this functional anatomy, cerebellar ataxia is now clinically subdivided into (i) cerebellar motor syndrome, (ii) vestibulocerebellar syndrome, and (iii) cerebellar cognitive affective syndrome [5].
The ataxia syndrome can either emerge as the major element of a disease course or represent a symptom of more complex multisystemic disorders, and it can have a highly variegated etiology: this makes the proper classification and correct diagnosis of ataxic patients very challenging. Namely, ataxic disorders can be classified, according to their etiology, in acquired, hereditary, or sporadic non-hereditary degenerative forms, all comprising a huge list of diseases with distinct origins [3,6]. Acquired ataxias are due to exogenous or endogenous non-genetic causes, such as stroke, toxicity, vitamin deficiency, immune inflammation, nutritional deficiencies, and chronic central nervous system (CNS) infections [6,7]. Hereditary forms comprise several genetic disorders that are characterized by slowly progressive incoordination of movement and speech and can be inherited (i) in an autosomal recessive manner, such as Friedreich’s ataxia (FA) and Ataxia Telangiectasia (AT); (ii) in a dominant manner, like Spinocerebellar Ataxia (SCA) and Episodic Ataxia (EA); or (iii) in an X-linked manner [8]. Finally, sporadic ataxia can either be caused by random mutations in single gene or comprise those forms for which a definite genetic impairment or acquired etiology cannot be found, such as the cerebellar variant of the Multiple System Atrophy (MSA) [9] and the so-called sporadic adult-onset ataxia of unknown etiology (SAOA) [10].
Common features of most ataxias are cerebellar atrophy and Purkinje cells (PCs) degeneration. For this reason, despite back in the past gliosis was repeatedly reported in autopsies of human ataxic samples [11,12,13], researchers have focused for many years mainly on neuronal dysfunctions, largely overlooking the possible implication of non-neuronal cells, including microglia, oligodendrocytes, and astrocytes, in this disorder. Nevertheless, in the past years, this trend changed its direction. Indeed, early microglial activation was reported during post-mortem analyses in several forms and animal models of ataxia and was described to play a detrimental role by driving neuroinflammation [14]. Moreover, white matter degeneration was reported in SCA2,3,7,10 and AT [15,16,17,18,19,20,21] and often correlated with ataxia severity: although white matter changes have largely been suspected to be secondary to neuronal loss, they are also likely to result from oligodendrocytes impairments. Indeed, mutant ATXN3 expression was shown to cause cell-autonomous transcriptional changes in oligodendrocytes that may directly disrupt white matter and be, therefore, implicated in the pathogenesis of SCA3 [16]. Similar changes in oligodendrocyte genes transcription may also occur in other genetic forms of ataxia and, in general, may cause oligodendrocyte dysfunctions that could impede the correct propagation of neuronal action potentials and, in turn, promote neuronal dysfunction and degeneration. Along the same line, in MSA, alpha-synuclein expression in oligodendrocytes was suggested to perturb their ability to provide trophic support to neurons, thereby contributing to diffuse neurodegeneration in this disease [22]. Lastly, an increased number of oligodendrocytes without mitotic activity was observed in childhood ataxia with diffuse central hypomyelination (CACH) syndrome, again suggesting that defects in these cells may be implicated in the etiopathology of cerebellar dysfunctions [23].
Among glial cells, astrocytes play a plethora of roles essential for brain development, homeostasis, and function [24,25,26]. As a consequence, no wonder they are increasingly being described as implicated in several neurodevelopmental and neurodegenerative disorders, such as Rett syndrome, fragile X mental retardation, amyotrophic lateral sclerosis, and Alzheimer’s disease [27,28,29], and they may be similarly involved in the pathophysiology of ataxia.
In the cerebellum, astrocytes are generated through a tightly regulated process and can be classified according to their morphologies and layering into three main categories, comprising Bergmann glia (BG) and granular layer astrocytes in the cerebellar cortex and fibrous astrocytes in the cerebellar white matter [30,31]. In the cortical layers, different astrocyte types interact with distinct neuronal subsets (Figure 1) and, therefore, are likely to develop neuron-specific functional properties, similarly important for the correct cerebellar development and functioning. Nevertheless, provided their highly specialized morphology and tight connection with the whole dendritic tree and soma of PCs, BGs are the most extensively studied astrocytes in the cerebellum, and their functions in supporting cerebellar development, PC synaptogenesis, and synaptic activity have already been described [32]. On the other side, very little is known about the specific functions and physiology of astrocytes in the granular layer, although their close relationship with the cerebellar glomeruli (i.e., the synaptic structures composed of mossy fibers rosettes, Golgi neuron boutons, and granule cells “GC” dendrites) [33,34] suggest that they may be similarly crucial for the regulation of tissue homeostasis and cerebellar circuits functioning.
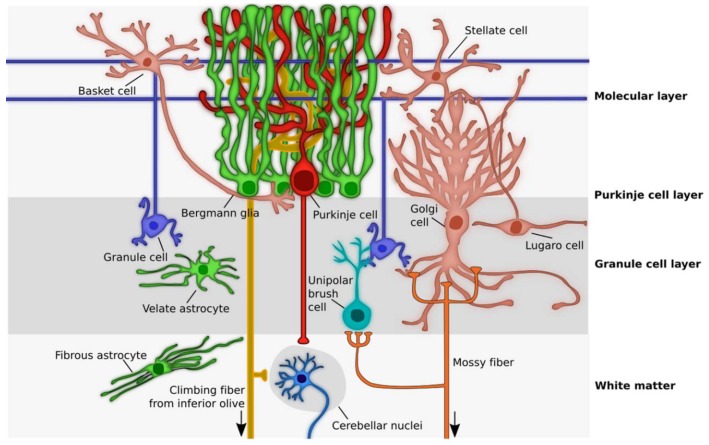
Figure 1.
Schematic picture showing cerebellar cytoarchitecture. Cerebellar cortex is composed of three layers. In the innermost layer, the Granule cell layer, excitatory granule cells are surrounded by Golgi and Lugaro cells, two kinds of inhibitory interneurons, as well as by the excitatory unipolar brush cells and velate astrocytes. Here, velate astrocytes are in close relationship with the so-called cerebellar glomeruli, composed of mossy fibers rosettes, Golgi neuron boutons, and granule cells dendrites. The Purkinje cell layers host the cell bodies of Purkinje cells and Bergmann glia, whose dendrites and fibers, respectively, span the whole length of the outermost layer of the cerebellum, the Molecular layer. Here, granule cells’ parallel fibers synapse directly onto Purkinje cells dendrites and have contact points with molecular layer interneurons, called Basket and Stellate cells. Moreover, the processes of Bergmann glia are in tight connection with the whole dendritic tree and soma of Purkinje cells. In the cerebellar white matter, fibrous astrocytes are aligned to axons, while in the deep cerebellum the cerebellar nuclei neurons receive inputs from both Purkinje cells and climbing fibers of inferior olive neurons and project either back to the inferior olive (the GABAergic neurons) or to the brainstem, midbrain, and thalamus (the glutamatergic neurons). Arrow, projections coming from outside the cerebellum.
In the last few decades, growing evidences are pointed at cerebellar astrocytes, specifically BG, as leading characters of a non-cell-autonomous neuronal degeneration in distinct forms of ataxia. Although intense work is still needed to clarify the role of astrocytes other than BG in this pathology, and despite the available knowledge is still very fragmentary and mainly ataxia type-specific, the present review will attempt to provide a comprehensive view of the mechanisms through which these cells are involved in the pathophysiology of ataxias, depicting a potential temporal cascade of events that eventually lead to the non-cell-autonomous neurodegeneration typical of this disease. A specific attention will be given to the pitfalls of the available models to study astrocytes’ contribution to the pathology, to promising new approaches to address this issue in the future and, importantly, to the potential forthcoming benefits of new therapies that specifically target astrocytes’ dysfunctions, a crucial point provided the absence of conclusive treatments for this disease.
2. Astrocytes Impairments are often Associated to Ataxic-Like Symptoms and Ataxia
A first hint of the possible involvement of astrocytes in ataxia is the evidence that their deficiency at multiple levels, from developmental impairments to the lack of their functional support to neurons, often results in motor impairments (Table 1). Indeed, astrocytes ablation from either the developing or the adult murine brain through distinct approaches was observed to result in severe ataxia, associated with PCs ectopic layering and abnormal dendritic arborization and with the degeneration of GCs [35,36]. These results provided the first in vivo evidence that astrocytes are critical for both cerebellar development and neuronal survival in the adult mouse brain. Along the same line, not only the lack of BG specification from cerebellar radial glia, due to the manipulation of several distinct genes, resulted in abnormal foliation and lamination and in locomotion defects [37,38,39,40] but also the incorrect maintenance of the BG phenotype (i.e., their ectopic location in the molecular layer and/or acquisition of a stellate morphology) during late postnatal development caused signs of ataxia in diverse mouse models [41,42]. Further, morphological defects of BG radial processes in vimentin-null mice also translated into impaired motor coordination, likely due to an aberrant structural and homeostatic support on PCs [43]. At last, the acquisition of an immature- or reactive-like state by cerebellar astrocytes in Dicer-deficient mice, as revealed by alterations in their transcriptome profiles, was shown to precede and to be likely responsible for a rapid neurologic decline, characterized by ataxia, GCs apoptosis and PCs degeneration [44]. Interestingly, this non-cell-autonomous neurodegeneration was faster in the central and posterior zones of the cerebellum and slower in the anterior and nodular areas, thereby suggesting a diverse susceptibility of neurons to astrocytes dysfunctions or an intrinsic heterogeneity of astrocytes in their response to ataxia-related mutant gene expression.
Table 1.
Astrocytes developmental or functional deficiencies result in neuronal degeneration and/or motor impairments.
| Astrocytes Alterations | Animal Model Applied | Cellular and Histological Impairments | Behavioral impairments | Reference |
|---|---|---|---|---|
| Astrocytes ablated postnatally | Herpes simplex virus- thymidine kinase expressed in mice under the control of the hGFAP gene promoter | Disordered radial glia; PCs ectopically distributed; abnormal PCs dendritic trees, depletion of GCs; reduction in cerebellar size; disruption of the cellular layers |
Severe ataxia | [35] |
| Astrocytes ablated in the adult | Targeted E. coli nitroreductase expression to the astrocytes of transgenic mice with the GFAP promoter | Abnormal PCs dendrites; GCs degeneration | Ataxic behavior | [36] |
| Absence of functional BG | Overexpression of the group C protein Sox4 in transgenic mice under the control of the hGFAP promoter | Fissures were not formed; neuronal layering was dramatically disturbed | Ataxic behavior | [37] |
| Disorganization of BG population | Knockout mouse with inactivation of the gene coding for the ubiquitin ligase Huwe1 in cerebellar GC precursors and radial glia | GCs migration defects; ectopic GC clusters; layering aberrations | Postnatal lethality | [38] |
| Radial glia fail to transform into BG | Deletion of Ptpn11 gene in the entire mouse cerebellum | Disorganized lamination and absence of cerebellar folia | Ataxic behavior | [39] |
| Deficits in BG specification | Mouse model lacking Zeb2 in cerebellar radial glia | Compromised inward migration of GCs, cortical lamination dysgenesis | Ataxic behavior | [40] |
| Ectopic positioning and aberrant stellate phenotype of BG arising postnatally | Conditional knockout mice in which the APC gene is inactivated in GFAP-expressing cells | Loss of PCs and cerebellar atrophy | Ataxic behavior | [41] |
| Decreased numbers, ectopic positioning and aberrant stellate phenotype of BG arising postnatally | Conditional Sox2 ablation in the whole mouse cerebellum or astrocytes | Cerebellar vermis hypoplasia, abnormal glutamate transport | Ataxic behavior | [42] |
| BG abnormal development | Vimentin knock-out mice | Abnormal PCs dendrites; PCs degeneration | Ataxic behavior | [43] |
| Immature/reactive-like phenotype acquisition by astrocytes | Cre-loxP conditional deletion of Dicer selectively from postnatal astroglia in mice | Cerebellar degeneration, apoptosis of GCs, degeneration of PCs | Ataxic behavior, seizures, uncontrollable movements and premature death arising late postnatally | [44] |
BG, Bergmann glia; GC, granule cells; hGFAP, human Glial Fibrillary Acidic Protein, PCs, Purkinje cells.
Evidence showing that cerebellar astrocytes may be involved in the pathophysiology of ataxia also came from the study of distinct animal models of this and other pathologies. Reactive astrocytosis and BG proliferation were indeed associated with PCs degeneration in the first mouse model of SCA1 (a polyglutamine spinocerebellar ataxia due to the expansion of a CAG trinucleotide repeat in the ATXN1 gene), in which the human mutant gene was expressed under the control of a PC-specific promoter [45]. On the other side, BG appeared to decrease before PCs degeneration in a different, non-PC-specific, mouse model of the same disease [46]. Moreover, the first three weeks of postnatal development were reported to be a critical period for the mutant ATXN1 gene expression to permanently influence the symptoms observed in the adult [31,47]. It is interesting to note that this developmental stage corresponds to the peak of astrocytes proliferation and differentiation, thereby suggesting that altered astrocytes development due to mutant ATXN1 expression may significantly contribute to disease progression. Increased expression of the glial fibrillary acidic protein (GFAP), astrogliosis, and thickening of BG processes were also observed in regions with extensive PC loss in a PC-specific Tmem30a KO mouse model that displays early-onset ataxia. In this case, astrocytic reactivity resulted from neuronal impairments and/or degeneration and likely further exacerbated neuronal loss contributing to disease progression, as will be discussed later [48]. A prominent astroglial activation and an impaired functioning of the glutamate-aspartate transporter GLAST, mediated by the proinflammatory cytokine interleukin-1β (IL-1β), were observed in the cerebella of experimental autoimmune encephalomyelitis (EAE) mice. These data hint that cerebellar astrocytes may also be involved in the cerebellar deficits and motor impairments typical of Multiple Sclerosis [49].
Interestingly, cerebellar astrocytes are also likely to be involved in the pathogenesis of those acquired ataxias due to alcohol abuse. Indeed, they were shown in vitro to be capable of synthesizing high levels of retinoic acid (RA) when exposed to ethanol [50]. RA, ligand for a group of ligand-activated transcription factors known as the RA receptors, is necessary for the development of many organs including the CNS but, when too much concentrated, can have teratogenic effects. Specifically, RA exposure was shown to cause abnormalities similar to those observed in the fetal alcohol syndrome (FAS), many of which are associated with cerebellar deficits: the aforementioned evidence thereby suggests that the cerebellar pathology exerted by ethanol may occur, at least in part, through an increased production of RA by cerebellar astrocytes. Although a direct in vivo demonstration of this hypothesis is still missing, the same authors showed that cerebellar RA levels were increased also in rat pups after ethanol administration [50]. Besides the dramatic effects of ethanol exposure on cerebellar development, alcohol abuse in adult life also causes cerebellar dysfunctions [51]. In this frame, astrocytes are again likely to play a crucial role. Indeed, even a brief ethanol exposure was shown to be sufficient to cause long-lasting changes in the gene expression, proliferation, and activity of mature astrocytes of distinct brain regions, with dramatic effects on the surrounding neurons [52]. Overall, these results indicate that astrocytes may contribute to cerebellar dysfunctions resulting from alcohol exposure both during fetal/postnatal and adult life.
3. Astrocytes Involvement in Ataxia as Revealed by Astrocyte-Specific Mutant Animal Models
In light of the aforementioned evidence and of those implying astrocytes as involved in the pathogenesis of several neurologic disorders, over the last fifteen years, scientists have begun to shift gradually their focus from neurons to astrocytes in the investigation of the cellular mechanisms underlying ataxia. Due to the genetic nature of many forms of this disease, the creation of animal models in which the mutant genes were selectively expressed or deleted in glial cells or, specifically, in astrocytes has been the most common approach to tackle this issue.
A first example is represented by SCAs that mostly belong to the category of polyglutamine diseases and comprise distinct forms characterized by CAG expansions on specific genes. The glial expression of SCA-related polyglutamine proteins has been shown several times to cause non-cell autonomous neurological symptoms, pointing to glial cells as anything but passive bystanders in the pathogenesis of this disease. Drosophila models expressing in glial cells the mutant ATXN1 and ATXN3 genes, associated with SCA1 and SCA3, respectively, showed accumulation of the protein fragments in glial intranuclear inclusions, accompanied by progressive degeneration of glial and neuronal cells, severe behavioral defects, and lethality [53,54]. Similar pieces of evidence of non-cell autonomous neurodegeneration were also obtained in a SCA7 mouse model where the expression of the mutant ATXN7 gene in all cells but not in PCs led to ataxia and PCs degeneration [55]. Nevertheless, the demonstration that astrocytes were the main actors in this process only came some years later, when the conditional expression in BG of the mutant gene through a Gfa2 promoter (version of the GFAP promoter with restricted expression in BG) was sufficient to cause motor incoordination and PCs pathology [56]. Later, the same authors developed an elegant animal model to better investigate the contribution of BG to the disease pathogenesis, by removing the mutant gene, in a context of ubiquitous expression, in a temporally and cell type-regulated fashion. Although the deletion of the mutant ATXN7 gene solely in BG was not sufficient per se to prevent the development of ataxia and neurodegeneration, its excision from BG in combination with PCs and inferior olivary (IO) neurons yielded a synergistic effect on the delay of symptoms onset [57]. Altogether, these results support a significant role of BG in SCA7 pathogenesis where both cell-autonomous and non-cell autonomous mechanisms are likely to contribute to neurodegeneration in a tightly interconnected network between neurons and BG. Similarly, neurodegeneration in SCA17 was reported to depend on the concomitant expression of the mutant TATA-binding protein (TBP) gene in both neurons and astrocytes, while the mutant gene expressed in either of the two cell populations only caused a mild PCs degeneration [58]. A synergistic effect of defective neurons and astrocytes holds true also for other forms of ataxia, as addressed later in this review.
Another genetic form of ataxia is Friedreich ataxia (FA), caused by an unstable GAA expansion in the first intron of the FXN gene, which results in decreased levels of a protein called frataxin. To mimic frataxin deficiency, animal models were developed in which the wild-type FXN gene was ubiquitously silenced, resulting in neuronal degeneration, motor impairments, and reduced lifespan. Interestingly, specific deletion of this gene in glial cells in Drosophila generated FA-like symptoms comparable to those of the whole-body knockout flies [59], and its ablation in developing mice from GFAP-expressing neuronal and astrocyte precursors resulted in severe ataxia and early death, associated with growth and survival impairments in cerebellar astrocytes [60]. Although, in this mouse model, the contribution of mutant neuronal and astrocyte precursors could not be discriminated, the evidence that the alterations observed were specific for cerebellar astrocytes and absent in forebrain astrocytes suggests that a greater vulnerability of developing cerebellar astrocytes to frataxin depletion may contribute to the highly specific cerebellar disturbances typical of FA. On the other side, in one of the very few studies exploiting cultured human astrocytes, cortical astrocytes with frataxin deficiency (obtained through an shRNA knockdown approach) also showed detrimental effects, with signs of reduced proliferation and survival. This hints that the cerebellar-specific phenotype of this disease may also result from minor sensitivity to frataxin-deficient astrocytes of some neuronal populations in regions other than the cerebellum [61].
Ataxia Telangiectasia is a rare inherited disorder caused by mutations in the Ataxia Telangiectasia Mutated (ATM) gene, coding for the homonym protein involved in cell division and DNA repair. The first evidence of a glial-mediated non-cell autonomous mechanism of neurodegeneration in AT came from the specific ATM knockdown in glial cells in Drosophila, shown to be sufficient to activate an inflammatory response mediated by glial cells that drove the degeneration of both neurons and glia and resulted in reduced mobility and decreased lifespan [62]. Nevertheless, the aberrant effects of ATM deficiency in mouse cerebellar astrocytes were unveiled with an in vitro chimeric system and confirmed in vivo only very recently [63]. Indeed, while chimeric cultures composed of normal astrocytes and ATM-deficient neurons did not show any structural or functional anomalies, ATM-deficient astrocytes co-cultured with normal neurons not only showed a reduced length and number of processes but also led to altered numbers of pre- and postsynaptic puncta, to impaired neuronal synchronization, and to significant neuronal death. Adult cerebella from ATM-depleted mice similarly showed a disrupted morphology of both BG and GL astrocytes, with increased expression of synaptic markers at GABAergic synapses [63]. Although the neuronal population in the chimeric primary cultures was mostly represented by GCs and therefore no evidences are available on the effect of ATM-deficient astrocytes on PCs, on the whole, these results suggest that the neurodegeneration and impaired network dynamics in AT may at least in part due to a malfunctioning of cerebellar astrocytes, resulting in aberrant structural connections among neurons.
Niemann–Pick disease type C (NPC) is a rare autosomal recessive multisystemic disorder with early-onset ataxia as a cardinal feature, due to a progressive loss of cerebellar PCs [64]. The gene underlying 95% of the cases of this disorder is NPC1, involved in late endosomal lipid sorting and trafficking and, therefore, exploited as the main target for mutations or deletion in animal models intended to mimic this pathology. The available evidences on the role of glial cells and/or astrocytes in the coordination problems and progressive cerebellar degeneration typical of NPC have been controversial but eventually pointed to astrocytes as crucial contributors to this disease. Exploiting a chimeric mouse model with functional NPC1 only in some cells with a mosaic-like pattern, Ko and colleagues [65] first concluded that degeneration of PCs was cell-autonomous, similarly to Lopez et al. [66] who, some years later, observed that NPC1 rescue solely in astrocytes was not capable of preventing neurodegeneration and motor incoordination in NPC1-null mice. Nevertheless, these evidences have some points of criticism and are not sufficient at all to rule out astrocytes’ contribution to NPC pathology. Indeed, provided the tight connection of individual PCs with up to eight BG, in a mosaic context the lack of rescue of mutant neurons by some surrounding wild type astrocytes and, vice versa, the absence of detrimental effects exerted by some mutant astrocytes on healthy PCs [65] may be due to compensatory effects by other mutant or normal astrocytes, respectively. To clarify this point, animal models in which the NPC1 gene is conditionally mutated in all astrocytes are needed. On the other side, although NPC1 reintroduction in neurons of NPC1-deficient mice prevented neuron degeneration, this resulted in an only temporarily improved motor coordination, eventually not sufficient to block disease progression and mouse death [66]. Although the authors did not comment on this, this temporary rescue is likely to be due to surrounding mutant astrocytes that eventually contribute to the progression of the ataxic phenotype. Along this line, if neither astrocyte- nor neuron-specific NPC1 rescues are per se sufficient for an efficient recovery, it is likely that both neurons and astrocytes are involved in the pathogenesis of this disease. Indeed, an analogous study, in which the astrocyte-targeted re-expression of NPC1 in NPC1-null mice was obtained through a GFAP promoter-driven transgene, reported an enhanced survival of mice, decreased astrocytes reactivity, and delayed degeneration of PCs [67], thereby indicating that astrocytes contribute to disease progression. The same authors successively confirmed the co-operation of dysfunctional astrocytes and neurons in NPC by re-expressing the normal gene in both cell types, that translated into a nearly normal phenotype with neurodegeneration, motor symptoms, and death all delayed of several months compared to the neuron-only re-expression [68].
Further positive evidences came also from in vitro studies. First, in mouse neuron–astrocyte cocultures, NPC1-null astrocytes were shown to cause a decreased neurite growth of wild-type neurons due to a reduced estradiol release [69]. Moreover, simultaneous absence of the gene in co-cultured neurons and glial cells, but not in neurons solely, resulted in impaired presynaptic development, as revealed by reduced synaptophysin-positive puncta on PC dendrites [70]. Although it is not clear whether this altered presynaptic input on PCs may contribute to the progressive degeneration of these cells and the behavioral impairments typical of NPC, these results indicate that both neuronal and glial NPC1 are required for proper presynaptic development and, added to the previous observations, confirm that neurons and astrocytes may cooperate in NPC disease progression. To further confirm this point, the investigation of the in vivo effects of an astrocyte-and/or neuron-specific deletion of the gene is still missing and is needed in future studies.
Overall, these results confirm that the complex interplay between neurons and astrocytes is necessary for the proper development and functioning of the cerebellar circuitries; at least in genetic forms of ataxias, where astrocyte-specific contribution was so far investigated, impairments in neurons and astrocytes both contribute to disease progression. Some of the mechanisms underlying this process have already been clarified and will be hereafter addressed.
4. How do Astrocytes Contribute to Ataxias? A Multi-Step Hypothesis
4.1. Cell-Autonomous Effects of Mutant Gene Expression in Astrocytes
Mutant ataxia-related genes are ubiquitously expressed and, therefore, are unlikely to cause developmental and/or functional impairments in neurons solely. Rather, their expression in astrocytes is likely to act as a first hit with distinct pathogenetic ripple effects.
As a first example, in a human astrocyte cell culture model of SCA7, the mutant ATXN7 gene was shown to downregulate the expression of RELN, gene intimately involved in the development and maintenance of the whole cerebellum and, specifically, of PCs [71]. Its downregulation in mutant SCA7 astrocytes was suggested to cause a non-cell autonomous, astrocytes-mediated, selective degeneration of PCS, thereby likely explaining the tissue specificity of SCA7. Nevertheless, these results still need to be confirmed in vivo in both the developing and mature cerebellum. Similarly, a SCA1 mouse model allowed to identify MAXER, coding for a novel multiple α-helix protein located at endoplasmic reticulum (ER), as an ATXN1 target gene. MAXER reduction in BG was shown to mediate their functional deficiency, inhibiting their proliferation, and reducing GLAST expression. The reduced levels of GLAST, both due to a decreased total number of BG and to a reduced expression on the spared cells, in turn, translated in glutamate-mediated neurotoxicity on PCs that could be rescued by MAXER overexpression [46]. Reduced numbers of BG, due to their massive death, were also very recently described in a SCA28 mouse model, in which the mutated gene AFG3L2 was selectively expressed in astrocytes [72]. Here, BG death was only the endpoint of a progressive degenerative process, characterized by their ectopic position, aberrant morphology, decreased expression of the calcium-binding protein S100 and the glutamate transporter GLT-1, upregulation of GFAP, abnormal mitochondrial network, and activated metabolic stress response. Altogether, these alterations may result in the lack of metabolic support on PCs, in glutamate-mediated PCs excitotoxicity and in the acquisition of a “reactive” phenotype by BG, and may, therefore, not only magnify but even cause PCs degeneration in SCA28. The acquisition of a reactive phenotype by astrocytes following their expression of mutant genes is indeed a common feature of distinct forms of ataxia. In the first humanized ATXN3 knock-in mouse model (Ki91 mice), expression of the mutant ATXN3 in astrocytes was reported to cause astrogliosis in the cerebellar white matter (one of the hallmarks of SCA3 in humans) due to the expression of Serpina3n [73]. Interestingly, Serpina3n expression was evident already in newborn mice, long before the onset of PCs degeneration and behavioral deficits in motor coordination, that appeared much later in one-year-old cerebella. Similarly, activated inflammatory pathways such as NF-kB were uncovered in mutant astrocytes in a cell culture model of SCA17 and their blocking was shown to ameliorate neurodegeneration [58].
Altogether, these evidences indicate that the expression of mutant ataxia-related genes in astrocytes may act as an intrinsic factor that, in turn, causes their developmental and/or functional impairments and ultimately contributes, or causes, degeneration of the nearby neurons.
One of the first and most common impairments appears to be the acquisition of a reactive phenotype by astrocytes whose detrimental effects in distinct forms of ataxia will be addressed in the next section.
4.2. Astrogliosis: An Early Point Of No Return?
Cerebellar astrogliosis is not only among the first cell-intrinsic effects of the expression of ataxia-related genes in cerebellar astrocytes [58,72,73] but it is also probably one of the astrocytes’ earliest responses to the abnormal behaviors of mutant neurons.
Early astrocyte activation was indeed observed in both the cerebellar nuclei (CN) and cortex in a SCA21 mouse model in which the mutated gene TMEM240 was expressed only in neurons [74]. Here, neuronal lysosomal impairments likely led to an active release of Damage-associated molecular patterns (DAMPs) or other factors that in turn triggered astrogliosis, resulting in motor dysfunctions without signs of neurodegeneration. Similarly, cerebellar astroglia was reported in several SCA1 mouse models to exhibit early signs of reactivity, recognized through increased GFAP expression, hypertrophy of cell bodies and processes, and expression of pro-inflammatory mediators [75]. Interestingly, this occurred well before the first signs of neurodegeneration and motor impairments and correlated with the disease in a spatio-temporal pattern, with most of the activated cells found in the most severely affected cerebellar regions. Again, this astrocyte activation was not caused by neurodegeneration, rather, it was shown to be triggered by signals originating from mutant PCs and could be arrested by preventing neuronal expression of the mutant ATXN1 gene. Successively, the same authors demonstrated that cerebellar astrogliosis contributes to SCA1 in a biphasic manner. By modulating astrocytes reactivity through the inhibition of the astroglial NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) signaling, they showed that when this pathway was inhibited during an early stage of disease (i.e., before the onset of motor deficits), the disease severity was exacerbated, whereas its inhibition during a later phase ameliorated the motor impairments without, however, saving PCs from death [76]. These results are suggestive of the first neuroprotective role played by astrocytes in SCA1 pathogenesis, which becomes harmful later on. Very recently, an early increase in the expression of brain-derived neurotrophic factor (BDNF) was identified as a key mediator of the initial neuroprotective role of astrocytes: an early delivery of this factor is indeed capable of delaying motor impairments and PCs pathology in a SCA1 mouse model [77]. Whether a biphasic role of astrogliosis in the disease onset also holds true for other kinds of ataxia is still needs to be elucidated.
The crucial role of astrogliosis in the pathogenesis of ataxia has been recently further demonstrated in conditional mouse models of cerebellar neuroinflammation, where the IκB kinase 2 (IKK2), activator of the NF-κB pathway, was expressed in astrocytes or selectively in BG [78]. IKK2 expression for a limited time was indeed sufficient to cause neuroinflammation, astrogliosis, and subsequent ataxic features due to selective degeneration of PCs. On the other side, the inactivation of Myd88, a crucial factor for the activation of the IKK/NF-κB pathway, was shown to mitigate neuroinflammation and PCs death in a SCA6 mouse model [79].
Overall, these evidences demonstrated that astrocytes’ activation, induced either cell- or non-cell-autonomously, can exacerbate or even cause neuronal dysfunctions, which in turn trigger a further amplification of astrogliosis in a detrimental vicious circle. This astrogliosis-like astrocytes activation was shown to be irreversible in some instances [78], determining a very early and time-restricted “point of no return” that points to early intervention as a crucial approach for the development of new therapeutic strategies. Importantly, this pathogenetic mechanism is likely to be crucial not only for the genetic forms of ataxia so far described but also for the inflammatory cerebellar ataxias, occurring in various autoimmune/inflammatory conditions in which inflammatory insults cause selective cerebellar neurodegeneration.
4.3. Astrogliosis Detrimental Effects on the Surrounding Neurons
After brain injury, astrocytes were reported to undergo a dramatic morphological and transcriptional transformation and acquire two possible reactive phenotypes, named “A1” and “A2” based on their inductive cue and effects on neurons and other surrounding cells [80,81]. Specifically, while A2 astrocytes are induced by ischemia and strongly promote neuronal survival and tissue repair by secreting neurotrophic factors, A1 are induced after acute brain injury by microglia and, by secreting neurotoxins, are lethal to both neurons and oligodendrocytes. Moreover, A1 astrocytes fail in promoting neuronal survival, synapse formation, and function, and are unable to phagocyte synapses and myelin debris. These impaired mechanisms all result in neurodegeneration and often contribute to disease progression [82]. Although a direct evidence that reactive astrocytes in cerebellar ataxia acquire an A1 phenotype is still missing, several impairments were described to occur in these cells that may cause non-cell-autonomous neurodegenerative effects. These impairments, which will be addressed hereafter, comprise a deficient glutamate uptake, the loss of structural and functional support for neurons, and the production of toxic substances or their impaired clearance from the extracellular space.
4.3.1. Neurotoxicity Caused by Impaired Glutamate Uptake
One of the main consequences of the morphological changes in reactive astrocytes is an altered allocation of GLAST, astrocytic glutamate transporter necessary to maintain extracellular glutamate concentrations and avoid neuronal excitotoxicity. GLAST mispositioning may either be due to its spatial redistribution following astrogliosis, like its cluster-like appearance reported to occur in a SCA1 transgenic mouse model [83] or from the activation-related retraction of astrocytes processes, both resulting in its dislocation from PCs synapses. Furthermore, astrogliosis induced by the activation in astrocytes of IKK2, enzymatic complex involved in propagating the cellular response to inflammation, resulted in a strong downregulation of both GLAST and GLT-1, indicating that IKK2 per se may be a negative regulator of their expression in vivo and may directly mediate the local imbalance of glutamate homeostasis and neuronal excitotoxicity, at least in inflammatory cerebellar ataxias [78]. A progressive loss of GLAST was also reported in a mouse model of SCA5, leading to PCs degeneration and the worsening of the ataxic phenotype [84]. Here, PCs death was the result of a synergistic loss first of the neuronal glutamate transporter Excitatory amino-acid transporter 4 (EAAT4) in PCs and then of GLAST in astrocytes, with PCs in the posterior cerebellum showing a higher susceptibility due to the differential patterns of expression of EAAT4 across parasagittal bands [85,86]. Although the molecular mechanisms leading to the progressive loss of GLAST in these mice still need to be elucidated, it is tempting to speculate that this may result from the induction of an astrocyte reactive phenotype by surrounding sick PCs.
The significant contribution of glutamate-associated pathways to the pathogenesis of ataxia was very recently confirmed through innovative disease models based on SCA2 or SCA3 patients-derived induced pluripotent stem cells (iPSCs) [87]. Indeed, the treatment of iPSCs-derived neurons with glutamate resulted in altered composition of glutamate receptors, intracellular Ca2+ imbalance and, eventually, cytotoxicity and degeneration.
It is important to note that, besides resulting from astrocytes reactivity, impairments in glutamate uptake may also be caused by cell-autonomous mechanisms. Indeed, the ablation in mice of the SLC1A3 gene, coding for the GLAST transporter, results in severe motor impairments and several missense mutations, either inherited or de novo, in the GLAST gene were shown to cause distinct forms of episodic ataxia (EA), whose symptoms severity appeared sometimes correlated with the extent of glutamate transporter dysfunction (Table 2) [88,89,90,91,92,93]. Moreover, reduced expressions of GLAST and/or GLT-1 were reported in models of SCA1, SCA7, and SCA28 in which the mutant genes were selectively expressed in astrocytes [46,56,72], indicating that the genetic alterations underlying some forms of ataxia may directly interfere with the astrocytes-mediated glutamate uptake.
Table 2.
Mutations in the SLC1A3 (Solute Carrier Family 1 Member 3) gene cause episodic ataxia 6 (EA6). Distinct missense mutations, either inherited or sporadic, were identified in the SLC1A3 gene in patients with EA. This syndrome was designated as episodic ataxia 6 (EA6), although it shared many overlapping clinical features with EA2, identified by the presence of heterozygous pathogenic variants in the CACNA1A (calcium voltage-gated channel subunit alpha1) gene.
| Mutation in The SLC1A3 Gene | Functional Implications | Clinical Features | Family History | Reference |
|---|---|---|---|---|
| Heterozygous de novo Pro290Arg missense mutation | Decreased expression of GLAST and reduced capacity of glutamate uptake; increased anion currents through GLAST | Episodic and progressive ataxia, seizures, alternating hemiplegia, and migraine headache | Sporadic | [89,95] |
| Cys186Ser missense mutation | Modest but significant reduction of glutamate uptake | Milder manifestations of EA without seizures or alternating hemiplegia; overall similar to EA2 | + | [90] |
| Heterozygous Val393Ile missense mutation | May influence glutamate binding and anion conductance | EA2 like symptoms; recurrent ataxia, slurred speech, interictal nystagmus with late-onset age of sixth decade | + | [91] |
| Arg454Gln (Arg499Gln) missense mutation | n.a. | Progressive ataxia, dysarthria, dysphagia, in some cases with adult-onset | + | [96] |
| Missense Ala329Thr mutation (concomitant with a mutation in the CACNA1A gene) |
n.a. | Ataxia, dizziness, gaze-evoked nystagmus, seizures | + | [92] |
| De novo Thr318Ala missense mutation | n.a. | Typical EA2-like symptoms: recurrent ataxia, slurred speech; interictal nystagmus, mild cognitive impairment. Late-onset in the fourth or sixth decades | Sporadic | [92] |
| De novo Met128Arg missense mutation | May perturb the hydrophobic status of the membrane and affect glutamate uptake | Repeated episodes of ataxia: truncal ataxia, intentional tremor, slurred speech | Sporadic | [93] |
+, presence of family history; EA, episodic ataxia, GLAST, glutamate/aspartate transporter; n.a., not available.
Interestingly, a defective expression of GLT-1 in BG, associated with PCs hyperexcitation and motor impairments, was also reported in a mouse model of myotonic dystrophy type 1 (DM1), a multisystemic disorder in which cerebellar abnormalities are implicated [94]. This evidence suggests that an imbalance in glutamate uptake by cerebellar astrocytes may also contribute to a broad spectrum of disorders in which the cerebellum is involved through the altered motor and/or non-motor functions.
4.3.2. Neurotoxicity Caused by S100beta Release
Another mechanism through which reactive astrocytes contribute to PCs degeneration is the production and release of toxic substances, and the calcium-binding protein S100B turned out to be one of them. Indeed, the presence in PCs of S100B-containing vacuoles, well before the onset of motor impairments, was reported in a SCA1 mouse model [97] and was later on traced back to autophagic mechanisms and associated with alterations in the morphology of PCs dendritic spines [98]. The same authors further demonstrated, both in vitro and in vivo, that the presence of S100B-loaded vacuoles in PCs correlated with the absence of ATXN1 nuclear inclusions, thereby suggesting that glial S100B may modulate the solubility of the mutant ATXN1 protein and, in turn, mediate its toxicity in PCs [99]. Although the underlying signaling pathways are still not fully known, the authors speculated that the sustained supply of S100B by reactive astrocytes may activate in PCs some factors, such as the NDR2 kinase, which destabilize BG-PC contact sites and neurite growth and result in PCs degeneration. Moreover, S100B Ca2+-chelating properties may modulate sodium channels in neurons and cause their Ca2+ overload, contributing to both aberrant synaptic transmission and neurotoxicity [100,101]. It is also worth noting that an excessive extracellular content of S100B was reported to cause alterations in BG cortical organization and morphology, thereby further contributing to the weakening of PC-BG contacts and the redistribution of glutamate transporters, in another, detrimental, vicious circle [100].
Importantly, elevated S100B concentrations were found in the serum of SCA3 patients, although uncorrelated to the disease duration or severity [102]. These results suggest that S100B overload may be a common pathogenetic mechanism of distinct forms of ataxia and, importantly, point to the application of this protein as a peripheral marker of disease in ataxia.
Overall, these evidences indicate that much more than a neuronal issue lags behind neurodegeneration in ataxias. Conversely, astrocytes actively participate in the neurodegenerative process, causing and/or exacerbating neuronal dysfunctions. Although most of the pathogenetic mechanisms described above can derive from cell-autonomous astrocytes dysfunctions and individually contribute to disease onset or progression, here a temporal cascade of events was proposed in which astrocytes are active and crucial players in distinct phases of the ataxia course (Figure 2). If true, this multi-step hypothesis of astrocytes involvement in ataxia should be taken into account in view of developing new astrocytes-targeted and, ideally, stage-specific therapeutic approaches, as will be discussed later.
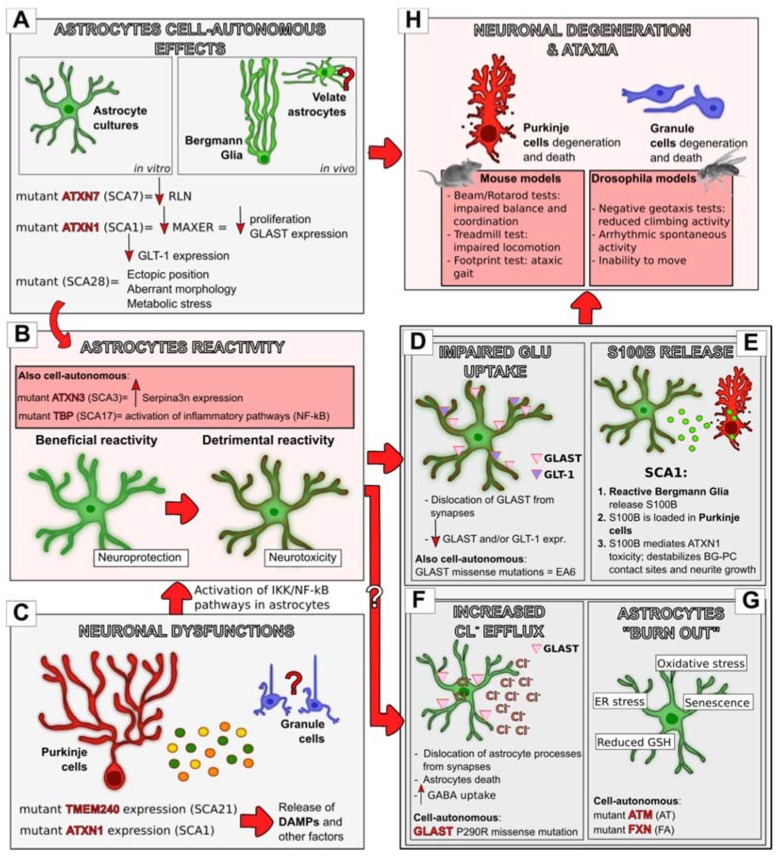
Figure 2.
The multi-step hypothesis of astrocytes’ involvement in ataxia. Astrocytes contribute to neuronal degeneration and motor impairments in distinct phases of the disease course. The expression of ataxia-related mutant genes in astrocytes can cause cell-autonomous impairments (A) that can contribute to neurodegeneration either directly (H) or indirectly through the acquisition of a reactive phenotype (B). This was demonstrated to occur in distinct in vitro models, and, in vivo, in BG, while whether this happens also in the other cerebellar cortical astrocytes still needs to be clarified. Astrocytes’ reactivity can also result from neuronal impairments ((C); demonstrated for PCs, likely to occur also in GCs), through the release from damaged neurons of DAMPs and other factors that can activate IκB kinase (IKK)/NF-kB inflammatory pathways in astrocytes that, in turn, become reactive (B). Interestingly, astrocytes’ reactivity was shown to play a dual function in Spinocerebellar Ataxia (SCA1) progression, first beneficial and later detrimental. Whether this holds true also for other forms of ataxia still needs to be elucidated. Reactive astrocytes, in turn, trigger neurodegeneration through distinct mechanisms, like the impairment of glutamate uptake (D) and the release of the calcium-binding protein S100B (E). Other neurotoxic mechanisms were shown to be an increase in the chloride efflux from astrocytes (F) and their accumulation of stress responses (G). Both these mechanisms were described to result from cell-autonomous impairments in astrocytes but may also result indirectly from their acquisition of a reactive phenotype. Glu, Glutamate, Big red arrows, successive step; small arrows, increase (facing up) or decrease (facing down). White question mark, hypothetical successive step; red question mark, hypothetical cellular involvement.
5. Other Pathogenetic Mechanisms of Astrocytes Involvement in Ataxia
5.1. Well beyond Glutamate Uptake: The Role Of Glast As Ion Channel And Its Implication In The Pathogenesis Of Ataxia
Besides the mechanisms so far described, which may be involved at distinct levels in a putatively multi-step progression of the disease, another way in which astrocytes have been recently associated to the pathogenesis of ataxia is through an abnormal anion conductance of GLAST that, although mostly known for glutamate transport, also plays an ancillary function as a chloride channel [103] (Figure 2). Specifically, the episodic ataxia 6 (EA6)-related point mutation P290R in the SLC1A3 gene (encoding GLAST) was shown not only to reduce the number of GLAST transporters on the surface of mammalian cells and impair their glutamate uptake but also to cause the appearance of larger anion currents with or without the administration of external glutamate [95]. Moreover, this mutation caused episodic paralysis of Drosophila larvae when expressed in glial cells [104]. A very similar behavior, with paralysis and astroglial aberrant morphologies, was induced after the expression in Drosophila of a chloride-extruding K+-Cl− cotransporter and was rescued by the expression of a Na+-K+-Cl− cotransporter, which normally allows chloride to enter into cells [104]. These results suggested for the first time that, although a reduced glutamate uptake was thought the be the main pathophysiological process underlying episodic ataxia, the P290R mutation in the SLC1A3 gene also causes abnormal chloride flow from astrocytes, contributing in this way to disease progression. These evidences were indeed very recently confirmed by the development of a transgenic mouse line, in which the mutation was carried by GLAST-expressing astrocytes solely (Slc1a3P290R/+ mice). This animal model was shown to suffer from epilepsy, ataxia, and showed cerebellar atrophy, thereby closely resembling the features of EA6 [105]. Specifically, these degenerative effects were unveiled to be triggered by an increased chloride efflux from BG, resulting in BG apoptosis and, subsequently, in a secondary loss of glutamate clearance and cerebellar atrophy.
The maintenance of a certain chloride concentration inside BG and, likely, inside astrocytes in general appears, therefore, to be a crucial point that had been so far underestimated. Not only chloride efflux from astrocytes may reduce their volume and dislocate their processes from synapses but it may also cause their death, therefore impairing their supportive role in neuronal functions and survival. Moreover, a reduced astrocytic chloride concentration may increase the driving force for GABA uptake of those transporters on astrocytes that cotransport both GABA and chloride, therefore attenuating GABA-mediated synaptic transmission.
Astrocytes were shown in the past to actively accumulate chloride upon activation. It will be fascinating to clarify whether any kind of alteration in chloride homeostasis may result also from the acquisition of a reactive phenotype by astrocytes in ataxia, and be therefore part of the multi-step progression of the disease proposed in the previous section. Similarly, whether an impaired GLAST chloride conductance is also involved in ataxias other than EA6 still needs to be elucidated.
5.2. When Astrocytes “Burn Out”: Stressed Astrocytes Cause Accumulation Of Oxidative Stress And Neurodegeneration
The role of astrocytes as antioxidant supporters for neurons is well accepted [106,107,108], and the loss of this support was often shown to lead to neuronal death in diverse neurodegenerative diseases [109,110]. Oxidative stress, associated with the activation of both mitochondrial and endoplasmic reticulum (ER) stress responses in astrocytes, was indeed shown to be involved in the pathophysiology of distinct ataxias (Figure 2).
First, in distinct in vitro models of Ataxia Telangiectasia, ATM-deficient astrocytes were shown to activate their oxidative and ER stress responses, which in turn translated in a senescence-like growth arrest through multiple Extracellular signal-regulated kinases 1/2 (ERK1/2)-dependent mechanisms, as demonstrated by the fact that treatments with the antioxidant N-acetyl-L-cysteine (NAC) not only restored their defective proliferation but also suppressed ERK phosphorylation/activation [111,112,113]. Stressed and senescent astrocytes, in turn, failed in providing their antioxidant support on neurons that eventually degenerated. Recently, the mechanism underlying this suboptimal antioxidant support of astrocytes was found in their impaired ability to import l-cystine and produce reduced glutathione (GSH), which is normally secreted by healthy astroglia in response to oxidative stress to provide additional support to neurons [114]. Specifically, stressed cerebellar astrocytes isolated from ATM-mutant mice showed decreased expression of the cystine/glutamate exchanger subunit xCT and of GSH reductase, which translated into reduced levels of both intracellular and secreted GSH. Consequently, when co-cultured with healthy neurons, these astrocytes provided insufficient GSH levels to support neuronal survival [114]. Nevertheless, the absence of neurodegeneration in AT experimental models did not allow so far to clarify whether this mechanism also holds true for astrocytes in vivo.
A similar involvement of oxidative stress in neurodegeneration was also proposed for Friedreich ataxia, in light of the abnormal levels of antioxidant enzymes found in the cerebella of frataxin-depleted mice [60]. In a Drosophila model of this disease, the expression of the mutant frataxin protein in glial cells was indeed shown to increase lipid peroxidation, inducing mitochondrial dysfunction and, in turn, accumulation of fatty acids and cell degeneration, which translated in a shortened lifespan and impaired locomotor performances [59]. Interestingly, co-expression in the glia of frataxin-deficient flies of Glaz, one of the Drosophila homologs of apolipoprotein D (ApoD), was sufficient to increase the lifespan and improve locomotor activity, likely due to its modulation of lipid composition and oxidation. The same authors later demonstrated that also an enhanced iron transport inside mitochondria was involved in the degenerative phenotype induced by frataxin depletion, as demonstrated by the fact that a reduction of mitoferrin, a mitochondrial iron transporter, significantly improved the motor impairments, while its overexpression enhanced them [115]. Further, Loria and colleagues [61] reported that frataxin-depleted cultured human astrocytes had altered mitochondrial morphology and suffered great oxidative stress, therefore supporting the idea that an increased mitochondrial iron content favors astrocytes oxidative stress.
Besides mitochondrial dysfunction, endoplasmic reticulum (ER) stress was recently reported as a novel and crucial player in the progression and etiology of FA. Indeed, in a Drosophila model of this disease, the downregulation in glial cells of Marf, a protein known to play crucial roles in mitochondrial fusion, mitochondrial degradation, and in the interface between ER and mitochondria, improved motor functions, neuronal degeneration, and lipid homeostasis through the suppression of ER stress [116]. Very similar results were obtained through ER stress reduction by means of two different chemical compounds, allowing the authors to conclude that the advantages conferred by Marf downregulation in glia were mainly due to its role in the mitochondrial-ER tethering.
Overall, these evidences support the role of astrocytes in both AT and FA, which is mediated by a progressive accumulation of either mitochondrial or ER stress, or both. Stressed astrocytes, in turn, fail to support and protect from oxidative stress their surrounding neurons, which eventually degenerate. Besides that, the analysis of the secretome from cultured human frataxin-deficient astrocytes also supported the hypothesis that stressed astrocytes may directly mediate neuroinflammation and, in turn, neurodegeneration through the release of specific cytokines involved in these processes [61].
6. Treating Astrocytes to Heal Neurons: New Promising Approaches For Ataxia Therapy
Provided the complex and extremely heterogeneous scenario of ataxias, no curative and confirmed pharmacological treatments are still available, neither for those forms with unknown etiology nor for those whose causes have already been clarified. The available treatments are supposed to ease symptoms and overall improve the quality of life of ataxia patients, comprising (i) physical and speech therapies to mitigate tremors, stiffness, and speech problems, (ii) globulines injections to boost the immune system in case of immune-mediated ataxias, and (iii) counseling or medications to alleviate the associated depression, anxiety, and sleep disorders. The only exceptions are played by those ataxias caused by nutritional deficiencies, such as a lack of vitamin E or coenzyme Q10, which respond well to supplements, and by some subtypes of episodic ataxia, which can often be successfully treated with the drug Acetazolamide, a carbonic anhydrase inhibitor supposed to prevent ataxic attacks by normalizing regional pH in the cerebellum and, in turn, by inducing physiologic changes in several types of ion channels [117]. In view of developing new therapies aimed at eradicating the disease from its roots, it is reasonable to think that targeting astrocytes’ dysfunctions, besides neuronal impairments, maybe a very promising approach, provided their critical involvement in the onset and/or progression of this disease. These putative astrocyte-targeted treatments should strictly depend on the nature of the disease and, ideally, should be stage-specific, provided the variegated mechanisms through which astrocytes have been reported to be involved in distinct forms and phases of ataxia.
The beneficial effects of treatments limiting astrocytes impairments were reported in distinct ataxia animal models and, in some instances, also in ataxic patients. As an example, treatments with estradiol were shown to delay the onset of neurological symptoms and increase PCs survival in Niemann Pick disease, counteracting its decreased secretion by NPC1-deficient astrocytes [69]. Similarly, in SCA7 patients, treatment with the histone deacetylase inhibitor trichostatin A could, at least in part, restore the defective reelin transcription in mutant astrocytes, promoting the accumulation of the mutant ATXN7 protein into nuclear inclusions and, therefore, slowing disease progression by reducing PCs neurotoxicity [71].
Inflammation and astrogliosis also appear as crucial players in disease progression. In this context, anti-inflammatory astroglia-based therapeutic approaches have been proposed for both SCA1 and SCA17 [58,76]. Yet, the evidence that intracerebroventricular injections of IL-1 receptor antagonist (IL-1ra) in EAE mice reduced motor deficits are very promising in view of responsiveness to anti-inflammatory treatments also in other forms of ataxia [49]. Importantly, although a bi-phasic role of astrogliosis in ataxia pathophysiology has been so far suggested only for SCA1, these treatments may need to consider the stage of disease progression to achieve therapeutic efficacy. In a first phase of the disease, when astrocytes’ reactivity may be protective [76], the inhibition of astroglial NF-κB signaling, likely effective at later stages [58], may indeed result detrimental, while BDNF delivery may delay disease onset fostering astrocytes’ defensive role against neurotoxicity, at least in SCA1 [77]. Similarly, even stimulating BG/astrocytes proliferation at this stage could be a viable therapeutic intervention [118].
The release of S100B by reactive astrocytes is one of the mechanisms through which these cells mediate the non-cell autonomous neurodegeneration of the surrounding PCs. In this context, the construction of substances that attenuate the activity of myo-inositol monophosphatase 1 (IMPA1), target of S100B whose activation is involved in the spines and dendrites abnormalities in PCs, has been suggested as potential therapeutic approach for SCA1 [98]. Similarly, treatment with the S100B inhibitory peptide TRTK12 was shown to improve motor performances in a model of SCA1 [99]. Importantly, both the activity of myo-inositol and the presence of S100B were proposed as glial-based biomarkers that could serve as indicators of disease progression and severity [75].
Besides S100B secretion, the impairment in glutamate uptake is the other main mechanism through which astrocytes contribute to neuronal toxicity and death. In this frame, in a mouse model of SCA28, increased expression of the glutamate receptor EAAT2 in astrocytes, promoting glutamate clearance, was obtained with the administration of the antibiotic ceftriaxone and ameliorated the ataxic phenotype [119]. Similarly, the cerebellar phenotype of myotonic dystrophy mice, due to spontaneous hyperactivity of PCs resulting in motor incoordination, was also ameliorated by ceftriaxone treatment [94], thereby suggesting that this kind of approach may be beneficial in distinct ataxic patients. Along the same line, anti-glutamate drugs were shown to reduce the death of SCA2- and SCA3-iPSCs-derived neurons [87], further indicating that glutamate-associated pathways are very promising drug targets across the variegated spectrum of ataxias.
Antioxidant therapies likely represent another valid approach to effectively ameliorate at least AT and FA, by reducing oxidative stress and supporting astrocytes’ functions in neuronal survival. Indeed, in AT in vitro models, NAC treatments were able not only to suppress the activation of stress and senescence pathways in mutant astrocytes [112] but also to restore normal GSH levels by circumventing the defects in l-cystine import in these cells, which were, therefore, again capable of supporting neuronal survival and neurite outgrowth [114]. Another approach to normalize GSH levels and overcome neuronal death in AT may be the drug-induced activation of the cystine/glutamate exchanger subunit xCT, already suggested for Parkinson’s disease and amyotrophic lateral sclerosis [120,121]. This kind of therapy would be, however, highly problematic, since it could result in overaccumulation of glutamate in the extracellular space causing neuronal toxicity. The direct delivery of NAC or other cysteine precursors, therefore, likely represents the safest solution among the antioxidant approaches. Along the same line, apolipoprotein D may provide an important therapeutic target, due to its modulation of lipid composition and lipid oxidation, as hinted by evidences obtained in a Drosophila model of FA [59]. On the other side, counteracting iron transport inside mitochondria may be another promising option to slow down neuronal degeneration in FA, and this could be achieved through mitoferrin depletion or iron chelation therapies [115,122]. Last, insulin-like growth factor I (IGF-I) injections were shown to protect neurons from frataxin deficiency in a non-cell autonomous fashion, both enhancing frataxin levels in astrocytes and potentiating their neuroprotective properties through the stimulation of the Akt/mTOR pathway [123].
Of particular relevance, gene therapy in the shape of antisense oligonucleotides (ASO) has been recently shown to attenuate the disease in a SCA3 mouse model by targeting not only neurons but also astrocytes [124]. Along the same line, a novel kind of synthetic antisense long non-coding RNAs capable of upregulating the expression of specific genes of interest, called SINEUPS, has been very recently shown to rescue defective frataxin expression and activity in a human cellular model of Friedreich’s Ataxia [125]: it will be interesting to evaluate in the future whether this approach can target both neuronal and non-neuronal cells. Gene therapy undoubtedly represents the new frontier for genetic diseases, and the precise targeting of cells of interest without side effects is one of the main goals of this innovative therapeutic approach: in view of its application in the genetic forms of ataxia, these cellular targets should be not only neurons but also astrocytes.
Importantly, in case cerebellar astrocytes are healthy because not primarily affected in ataxia etiology, they are likely to take a crucial part in the so-called “cerebellar reserve” [126]. The cerebellar reserve is indeed defined as the capacity of the cerebellum to compensate and restore function in response to pathology, and cerebellar astrocytes, with their endogenous neuroprotective effects, are likely to counteract neuronal damage and loss as described to occur in several other kinds of brain injury. This aspect is particularly relevant in view of planning new treatment strategies that could boost the astrocytes’ neuroprotective activity, at least in the initial phase of the disease when they maintain their structural and functional integrity. Astrocytes were indeed described to be able to (i) remove the excessive glutamate released by damaged or dying neurons and, therefore, protect other cells from excitotoxicity and neurodegeneration; (ii) take damaged mitochondria up from sick neurons defending them against mitochondrial dysfunctions; (iii) help attracting robust inflammation to sites of tissue damage in order to neutralize pathogens, clear debris, and promote tissue repair; (iv) express high levels of GSH in response to oxidative stress, which often results from an overproduction of reactive oxygen species (ROS) following injury [127]. These same mechanisms are likely to occur also in ataxia. Indeed, astrocytes astrogliosis was proposed to be neuroprotective in the first phases of SCA1 [76] and distinct treatments boosting specific astrocytes’ neuroprotective mechanisms were described to ameliorate the cerebellar phenotype of distinct forms of ataxia. Among them, the aforementioned drugs targeting glutamate-associated pathways may be beneficial in ataxic patients not only by counteracting astrocytes’ impairment in glutamate uptake but also by supporting healthy astrocytes in their neuroprotective activity. Similarly, the antioxidant therapies described before may facilitate astrocytes’ response to oxidative stress. Besides their neuroprotective effects, cerebellar astrocytes are likely to contribute to the “cerebellar reserve” also by sustaining compensatory responses in neural circuits, restoring lost connectivity in dysfunctional cerebellar networks. This was indeed described to occur in chimeric culture models of AT in which both structural and functional anomalies of ATM-deficient neurons were completely rescued by the presence of healthy astrocytes [63]. Moreover, in the wake of the recent evidence indicating that differentiated astrocytes can be triggered to change their fate and reprogram into neurons in the injured mouse cerebral cortex [128], if properly boosted, cerebellar astrocytes may represent a very promising source of new neurons in ataxic contexts, thereby incrementing the cerebellar reserve. This may be true specifically for BG. Indeed, evidence suggests that they belong to the same lineage of PCs, with whom they share the same origin in the embryonic ventricular zone and partially overlapping developmental trajectories [31]. Moreover, BG postnatal progenitors share striking similarities, both under the molecular and morphological point of view, with the embryonic outer radial glia (oRG) responsible for the generation of the majority of cortical neurons, are capable in vitro of producing neurospheres, and were shown to be capable of reprogramming into granule cells (GCs) following a postnatal depletion of GC precursors [129]. For these reasons, BG may represent a novel and abundant stem cell population in the adult cerebellum and appear to be the best cerebellar candidates to be triggered toward the PC fate, particularly promising in view treating cerebellar disorders.
7. Conclusions and Future Perspectives
The evidences summarized here indicate that astrocytes play pivotal roles in the pathogenesis of ataxias. Specifically, although the available knowledge is still fragmentary and mostly disease-specific, it looks evident that numerous mechanisms of astrocytes involvement in neurodegeneration are shared by diverse forms of ataxias and likely contribute to disease progression in a phase-specific fashion, of particular relevance in view of developing new astrocytes-targeted therapeutic approaches. Nevertheless, most of this knowledge relies on experimental models that mostly fail to faithfully recapitulate the human disease. For instance, the available animal models for AT do not show robust neurodegeneration or cerebellar atrophy, hallmarks of the human disease [130], while a mouse model of SCA1 in which the mutant ATXN1 was expressed at the endogenous level only showed mild behavioral impairments [46]. Similarly, an insufficient reduction of frataxin in FA mouse models translated into the absence of anomalies in motor coordination [60,131,132]. These effects, partially due to the short lifespan of mice that does not allow the neurons to accumulate significant damage, were often overcome by creating new animal models with transgenes expression exceeding the endogenous levels, which in turn led to dramatic and exaggerated outcomes that again did not reflect reality [56,133]. Importantly, in view of unveiling the astrocyte-specific effects of mutant protein expression/deletion, conditional experimental lines were developed in which, however, the transgene induction was often not sufficiently robust and, most importantly, depended on the kind of promoter and system (i.e., Cre-loxP, Tet-On/Off) used [60]. Lastly, many studies addressing glial involvement in ataxia [53,59,62,104,115,116] have been, still recently, based on the Drosophila model that, although very suitable to this aim due to its limited number of glial cells with well-known positions and molecular markers, may lead to an oversimplification of this issue. To overcome all these limitations, the use of patient-derived iPSCs differentiated into astrocytes or in the form of three-dimensional organoids, or of diseased human glial chimeric mice will represent, in the next future, a very promising approach to draw more solid conclusions on the cellular and molecular mechanisms underlying astrocytes involvement in ataxias and to screen drugs for treatments, as done for many other neurodegenerative disorders [134,135]. Moreover, the future identification of molecular markers specific for the distinct cerebellar astrocyte phenotypes, hopefully possible thanks to high throughput -omic approaches, will allow not only to differentiate distinct astrocyte subtypes from patient-derived cells but also to isolate distinct astrocytes populations from the available animal models and to develop new conditional ones in view of elucidating, if any, the role of cerebellar astrocytes other than BG in ataxia pathophysiology.
Acknowledgments
The author would like to thank Annalisa Buffo and Eriola Hoxha for proofreading the manuscript.
Funding
This study was supported by “Bando Ex- Post 2018” of the University of Turin and Compagnia di San Paolo, Turin and by the funds of the University of Turin and of Ministero dell’Istruzione, dell’Università e della Ricerca-MIUR project “Dipartimenti di Eccellenza 2018–2022” to the Department of Neuroscience, University of Turin.
Conflicts of Interest
The author declares no conflict of interest.
References
- 1.Watson T.C., Apps R. Cerebro-Cerebellar Connections. In: Manto M., Gruol D., Schmahmann J., Koibuchi N., Sillitoe R., editors. Handbook of the Cerebellum and Cerebellar Disorders. Springer International Publishing; Cham, Switzerland: 2019. [(accessed on 2 January 2020)]. pp. 1–26. Available online: [DOI] [Google Scholar]
- 2.Akbar U., Ashizawa T. Ataxia. Neurol. Clin. 2015;33:225–248. doi: 10.1016/j.ncl.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manto M., Marmolino D. Cerebellar ataxias. Curr. Opin. Neurol. 2009;22:419–429. doi: 10.1097/WCO.0b013e32832b9897. [DOI] [PubMed] [Google Scholar]
- 4.Apps R., Hawkes R., Aoki S., Bengtsson F., Brown A.M., Chen G., Ebner T.J., Isope P., Jorntell H., Lackey E.P., et al. Cerebellar Modules and Their Role as Operational Cerebellar Processing Units: A Consensus paper [corrected] Cerebellum. 2018;17:654–682. doi: 10.1007/s12311-018-0952-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manto M., Gandini J., Feil K., Strupp M. Cerebellar ataxias: An update. Curr. Opin. Neurol. 2020;33:150–160. doi: 10.1097/WCO.0000000000000774. [DOI] [PubMed] [Google Scholar]
- 6.Klockgether T. Sporadic ataxia with adult onset: Classification and diagnostic criteria. Lancet Neurol. 2010;9:94–104. doi: 10.1016/S1474-4422(09)70305-9. [DOI] [PubMed] [Google Scholar]
- 7.Klockgether T. Chapter 2 Acquired Cerebellar Ataxias and Differential Diagnosis. In: Brice A., Pulst S.-M., editors. Spinocerebellar Degenerations: The Ataxias and Spastic Paraplegias. Butterworth-Heinemann; Oxford, UK: 2007. [(accessed on 2 January 2020)]. pp. 61–77. (Blue Books of Neurology; vol. 31) Available online: http://www.sciencedirect.com/science/article/pii/S1877184X09700760. [Google Scholar]
- 8.Bird T.D. In: Hereditary Ataxia Overview. Adam M.P., Ardinger H.H., Pagon R.A., Wallace S.E., Bean L.J.H., Stephens K., Amemiya A., editors. University of Washington; Seattle, WA, USA: 1993. [(accessed on 2 January 2020)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK1138/ [PubMed] [Google Scholar]
- 9.Quinn N. Multiple system atrophy--the nature of the beast. J. Neurol. Neurosurg. Psychiatry. 1989;52:78–89. doi: 10.1136/jnnp.52.Suppl.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harding A.E. “Idiopathic” late onset cerebellar ataxia. A clinical and genetic study of 36 cases. J. Neurol. Sci. 1981;51:259–271. doi: 10.1016/0022-510X(81)90104-0. [DOI] [PubMed] [Google Scholar]
- 11.Nino H.E., Noreen H.J., Dubey D.P., Resch J.A., Namboodiri K., Elston R.C., Yunis E.J. A family with hereditary ataxia: HLA typing. Neurology. 1980;30:12–20. doi: 10.1212/WNL.30.1.12. [DOI] [PubMed] [Google Scholar]
- 12.Genis D., Matilla T., Volpini V., Rosell J., Davalos A., Ferrer I., Molins A., Estivill X.v. Clinical, neuropathologic, and genetic studies of a large spinocerebellar ataxia type 1 (SCA1) kindred: (CAG)n expansion and early premonitory signs and symptoms. Neurology. 1995;45:24–30. doi: 10.1212/WNL.45.1.24. [DOI] [PubMed] [Google Scholar]
- 13.Gilman S., Sima A.A., Junck L., Kluin K.J., Koeppe R.A., Lohman M.E., Little R. Spinocerebellar ataxia type 1 with multiple system degeneration and glial cytoplasmic inclusions. Ann. Neurol. 1996;39:241–255. doi: 10.1002/ana.410390214. [DOI] [PubMed] [Google Scholar]
- 14.Ferro A., Sheeler C., Rosa J.-G., Cvetanovic M. Role of Microglia in Ataxias. J. Mol. Biol. 2019;431:1792–1804. doi: 10.1016/j.jmb.2019.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hernandez-Castillo C.R., Galvez V., Mercadillo R., Diaz R., Campos-Romo A., Fernandez-Ruiz J. Extensive White Matter Alterations and Its Correlations with Ataxia Severity in SCA 2 Patients. PLoS ONE. 2015;10:e0135449. doi: 10.1371/journal.pone.0135449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramani B., Panwar B., Moore L.R., Wang B., Huang R., Guan Y., Paulson H.L. Comparison of spinocerebellar ataxia type 3 mouse models identifies early gain-of-function, cell-autonomous transcriptional changes in oligodendrocytes. Hum. Mol. Genet. 2017;26:3362–3374. doi: 10.1093/hmg/ddx224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hernandez-Castillo C.R., Vaca-Palomares I., Barrios F., Martinez L., Boll M.-C., Fernandez-Ruiz J. Ataxia Severity Correlates with White Matter Degeneration in Spinocerebellar Ataxia Type 7. Am. J. Neuroradiol. 2016;37:2050–2054. doi: 10.3174/ajnr.A4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alcauter S., Barrios F.A., Díaz R., Fernández-Ruiz J. Gray and white matter alterations in spinocerebellar ataxia type 7: An in vivo DTI and VBM study. Neuroimage. 2011;55:1–7. doi: 10.1016/j.neuroimage.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez-Castillo C.R., Diaz R., Vaca-Palomares I., Torres D.L., Chirino A., Campos-Romo A., Ochoa A., Rasmussen A., Fernandez-Ruiz J. Extensive cerebellar and thalamic degeneration in spinocerebellar ataxia type 10. Parkinsonism Relat. Disord. 2019;66:182–188. doi: 10.1016/j.parkreldis.2019.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Sahama I., Sinclair K., Fiori S., Doecke J., Pannek K., Reid L., Lavin M., Rose S. Motor pathway degeneration in young ataxia telangiectasia patients: A diffusion tractography study. NeuroImage Clin. 2015;9:206–215. doi: 10.1016/j.nicl.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciemins J.J., Horowitz A.L. Abnormal white matter signal in ataxia telangiectasia. AJNR Am. J. Neuroradiol. 2000;21:1483–1485. [PMC free article] [PubMed] [Google Scholar]
- 22.Mot A.I., Depp C., Nave K.-A. An emerging role of dysfunctional axon-oligodendrocyte coupling in neurodegenerative diseases. Dialogues Clin. Neurosci. 2018;20:283–292. doi: 10.31887/DCNS.2018.20.4/knave. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodriguez D., Gelot A., della Gaspera B., Robain O., Ponsot G., Sarliève L.L., Ghandour S., Pompidou A., Dautigny A., Aubourg P., et al. Increased density of oligodendrocytes in childhood ataxia with diffuse central hypomyelination (CACH) syndrome: neuropathological and biochemical study of two cases. Acta Neuropathol. 1999;97:469–480. doi: 10.1007/s004010051016. [DOI] [PubMed] [Google Scholar]
- 24.Chaboub L.S., Deneen B. Astrocyte form and function in the developing central nervous system. Semin. Pediatr. Neurol. 2013;20:230–235. doi: 10.1016/j.spen.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santello M., Toni N., Volterra A. Astrocyte function from information processing to cognition and cognitive impairment. Nat. Neurosci. 2019;22:154–166. doi: 10.1038/s41593-018-0325-8. [DOI] [PubMed] [Google Scholar]
- 26.Jha M.K., Kim J.-H., Song G.J., Lee W.-H., Lee I.-K., Lee H.-W., An S.S.A., Kim S., Suk K. Functional dissection of astrocyte-secreted proteins: Implications in brain health and diseases. Prog. Neurobiol. 2018;162:37–69. doi: 10.1016/j.pneurobio.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Molofsky A.V., Krenick R., Ullian E., Tsai H.H., Deneen B., Richardson W.D., Barres B.A., Rowitch D.H. Astrocytes and disease: A neurodevelopmental perspective. Genes Dev. 2012;26:891–907. doi: 10.1101/gad.188326.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carter S.F., Herholz K., Rosa-Neto P., Pellerin L., Nordberg A., Zimmer E.R. Astrocyte Biomarkers in Alzheimer’s Disease. Trends Mol. Med. 2019;25:77–95. doi: 10.1016/j.molmed.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 29.Yamanaka K., Komine O. The multi-dimensional roles of astrocytes in ALS. Neurosci. Res. 2018;126:31–38. doi: 10.1016/j.neures.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 30.Cerrato V., Buffo A. Handbook of the Cerebellum and Cerebellar Disorders. Springer; Berlin, Germany: 2019. [(accessed on 2 January 2020)]. Gliogenesis; pp. 1–17. Available online: http://link.springer.com/10.1007/978-3-319-97911-3_108-1. [Google Scholar]
- 31.Cerrato V., Parmigiani E., Figueres-Oñate M., Betizeau M., Aprato J., Nanavaty I., Berchialla P., Luzzati F., de’Sperati C., López-Mascaraque L., et al. Multiple origins and modularity in the spatiotemporal emergence of cerebellar astrocyte heterogeneity. PLoS Biol. 2018;1:16. doi: 10.1371/journal.pbio.2005513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buffo A., Rossi F. Origin, lineage and function of cerebellar glia. Prog. Neurobiol. 2013;109:42–63. doi: 10.1016/j.pneurobio.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Chan-Palay V., Palay S.L. High voltage electron microscopy of rapid golgi preparations. Neurons and their processes in the cerebellar cortex of monkey and rat. Z Anat. Entwicklungsgesch. 1972;137:125–153. doi: 10.1007/BF00538787. [DOI] [PubMed] [Google Scholar]
- 34.Palay S., Chan-Palay V. Cerebellar Cortex. Springer; New York, NY, USA: 1974. [Google Scholar]
- 35.Delaney C.L., Brenner M., Messing A. Conditional Ablation of Cerebellar Astrocytes in Postnatal Transgenic Mice. J. Neurosci. 1996;16:6908–6918. doi: 10.1523/JNEUROSCI.16-21-06908.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cui W., Allen N.D., Skynner M., Gusterson B., Clark A.J. Inducible ablation of astrocytes shows that these cells are required for neuronal survival in the adult brain. Glia. 2001;34:272–282. doi: 10.1002/glia.1061. [DOI] [PubMed] [Google Scholar]
- 37.Hoser M., Baader S.L., Bösl M.R., Ihmer A., Wegner M., Sock E. Prolonged glial expression of Sox4 in the CNS leads to architectural cerebellar defects and ataxia. J. Neurosci. 2007;27:5495–5505. doi: 10.1523/JNEUROSCI.1384-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D’Arca D., Zhao X., Xu W., Ramirez-Martinez N.C., Iavarone A., Lasorella A. Huwe1 ubiquitin ligase is essential to synchronize neuronal and glial differentiation in the developing cerebellum. Proc. Natl. Acad. Sci. USA. 2010;107:5875–5880. doi: 10.1073/pnas.0912874107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li K., Leung A.W., Guo Q., Yang W., Li J.Y.H. Shp2-dependent ERK signaling is essential for induction of Bergmann glia and foliation of the cerebellum. J. Neurosci. 2014;34:922–931. doi: 10.1523/JNEUROSCI.3476-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He L., Yu K., Lu F., Wang J., Wu L.N., Zhao C., Li Q., Zhou X., Liu H., Mu D., et al. Transcriptional Regulator Zeb2 is Essential for Bergmann Glia Development. J. Neurosci. 2018;38:1575–1587. doi: 10.1523/JNEUROSCI.2674-17.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang X., Imura T., Sofroniew M.V., Fushiki S. Loss of adenomatous polyposis coli in Bergmann glia disrupts their unique architecture and leads to cell nonautonomous neurodegeneration of cerebellar Purkinje neurons. Glia. 2011;59:857–868. doi: 10.1002/glia.21154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cerrato V., Mercurio S., Leto K., Fucà E., Hoxha E., Bottes S., Pagin M., Milanese M., Ngan C.-Y., Concina G., et al. Sox2 conditional mutation in mouse causes ataxic symptoms, cerebellar vermis hypoplasia, and postnatal defects of Bergmann glia. Glia. 2018;66:1929–1946. doi: 10.1002/glia.23448. [DOI] [PubMed] [Google Scholar]
- 43.Colucci-Guyon E., Gimenez YRibotta M., Maurice T., Babinet C., Privat A. Cerebellar defect and impaired motor coordination in mice lacking vimentin. Glia. 1999;25:33–43. doi: 10.1002/(SICI)1098-1136(19990101)25:1<33::AID-GLIA4>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 44.Tao J., Wu H., Lin Q., Wei W., Lu X.-H., Cantle J.P., Ao Y., Olsen R.W., Yang X.W., Mody I., et al. Deletion of astroglial Dicer causes non-cell-autonomous neuronal dysfunction and degeneration. J. Neurosci. 2011;31:8306–8319. doi: 10.1523/JNEUROSCI.0567-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burright E.N., Clark H.B., Servadio A., Matilla T., Feddersen R.M., Yunis W.S., Duvick L.A., Zoghbi H.Y., Orr H.T. SCA1 transgenic mice: A model for neurodegeneration caused by an expanded CAG trinucleotide repeat. Cell. 1995;82:937–948. doi: 10.1016/0092-8674(95)90273-2. [DOI] [PubMed] [Google Scholar]
- 46.Shiwaku H., Yoshimura N., Tamura T., Sone M., Ogishima S., Watase K., Tagawa K., Okazawa H. Suppression of the novel ER protein Maxer by mutant ataxin-1 in Bergman glia contributes to non-cell-autonomous toxicity. EMBO J. 2010;29:2446–2460. doi: 10.1038/emboj.2010.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Serra H.G., Duvick L., Zu T., Carlson K., Stevens S., Jorgensen N., Lysholm A., Burright E., Zoghbi H.Y., Clark H.B., et al. RORalpha-mediated Purkinje cell development determines disease severity in adult SCA1 mice. Cell. 2006;127:697–708. doi: 10.1016/j.cell.2006.09.036. [DOI] [PubMed] [Google Scholar]
- 48.Yang Y., Sun K., Liu W., Zhang L., Peng K., Zhang S., Li S., Yang M., Jiang Z., Lu F., et al. Disruption of Tmem30a results in cerebellar ataxia and degeneration of Purkinje cells. Cell Death Dis. 2018;9:899. doi: 10.1038/s41419-018-0938-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mandolesi G., Musella A., Gentile A., Grasselli G., Haji N., Sepman H., Fresegna D., Bullitta S., De Vito F., Musumeci G., et al. Interleukin-1beta alters glutamate transmission at purkinje cell synapses in a mouse model of multiple sclerosis. J. Neurosci. 2013;33:12105–12121. doi: 10.1523/JNEUROSCI.5369-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McCaffery P., Koul O., Smith D., Napoli J.L., Chen N., Ullman M.D. Ethanol increases retinoic acid production in cerebellar astrocytes and in cerebellum. Dev. Brain Res. 2004;153:233–241. doi: 10.1016/j.devbrainres.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 51.Luo J. Effects of Ethanol on the Cerebellum: Advances and Prospects. Cerebellum. 2015;14:383–385. doi: 10.1007/s12311-015-0674-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adermark L., Bowers M.S. Disentangling the Role of Astrocytes in Alcohol Use Disorder. Alcohol. Clin. Exp. Res. 2016;40:1802–1816. doi: 10.1111/acer.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tamura T., Sone M., Yamashita M., Wanker E.E., Okazawa H. Glial cell lineage expression of mutant ataxin-1 and huntingtin induces developmental and late-onset neuronal pathologies in Drosophila models. PLoS ONE. 2009;4:e4262. doi: 10.1371/journal.pone.0004262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kretzschmar D., Tschape J., Bettencourt Da Cruz A., Asan E., Poeck B., Strauss R., Pflugfelder G.O. Glial and neuronal expression of polyglutamine proteins induce behavioral changes and aggregate formation in Drosophila. Glia. 2005;49:59–72. doi: 10.1002/glia.20098. [DOI] [PubMed] [Google Scholar]
- 55.Garden G.A., Libby R.T., Fu Y.-H., Kinoshita Y., Huang J., Possin D.E., Smith A.C., Martinez R.A., Fine G.C., Grote S.K., et al. Polyglutamine-expanded ataxin-7 promotes non-cell-autonomous purkinje cell degeneration and displays proteolytic cleavage in ataxic transgenic mice. J. Neurosci. 2002;22:4897–4905. doi: 10.1523/JNEUROSCI.22-12-04897.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Custer S.K., Garden G.A., Gill N., Rueb U., Libby R.T., Schultz C., Guyenet S.J., Deller T., Westrum L.E., Sopher B.L., et al. Bergmann glia expression of polyglutamine-expanded ataxin-7 produces neurodegeneration by impairing glutamate transport. Nat. Neurosci. 2006;9:1302–1311. doi: 10.1038/nn1750. [DOI] [PubMed] [Google Scholar]
- 57.Furrer S.A., Mohanachandran M.S., Waldherr S.M., Chang C., Damian V.A., Sopher B.L., Garden G.A., La Spada A.R. Spinocerebellar ataxia type 7 cerebellar disease requires the coordinated action of mutant ataxin-7 in neurons and glia, and displays non-cell-autonomous bergmann glia degeneration. J. Neurosci. 2011;31:16269–16278. doi: 10.1523/JNEUROSCI.4000-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang Y., Yang S., Guo J., Cui Y., Tang B., Li X.-J., Li S. Synergistic Toxicity of Polyglutamine-Expanded TATA-Binding Protein in Glia and Neuronal Cells: Therapeutic Implications for Spinocerebellar Ataxia 17. J. Neurosci. 2017;37:9101–9115. doi: 10.1523/JNEUROSCI.0111-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Navarro J.A., Ohmann E., Sanchez D., Botella J.A., Liebisch G., Molto M.D., Ganfornina M.D., Schmitz G., Schneuwly S. Altered lipid metabolism in a Drosophila model of Friedreich’s ataxia. Hum. Mol. Genet. 2010;19:2828–2840. doi: 10.1093/hmg/ddq183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Franco C., Genis L., Navarro J.A., Perez-Domper P., Fernandez A.M., Schneuwly S., Alemán I.T. A role for astrocytes in cerebellar deficits in frataxin deficiency: Protection by insulin-like growth factor I. Mol. Cell. Neurosci. 2017;80:100–110. doi: 10.1016/j.mcn.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 61.Loria F., Diaz-Nido J. Frataxin knockdown in human astrocytes triggers cell death and the release of factors that cause neuronal toxicity. Neurobiol. Dis. 2015;76:1–12. doi: 10.1016/j.nbd.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 62.Petersen A.J., Rimkus S.A., Wassarman D.A. ATM kinase inhibition in glial cells activates the innate immune response and causes neurodegeneration in Drosophila. Proc. Natl. Acad. Sci. USA. 2012;109:E656–E664. doi: 10.1073/pnas.1110470109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kanner S., Goldin M., Galron R., Ben Jacob E., Bonifazi P., Barzilai A. Astrocytes restore connectivity and synchronization in dysfunctional cerebellar networks. Proc. Natl. Acad. Sci. USA. 2018;115:8025–8030. doi: 10.1073/pnas.1718582115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vanier M.T. Niemann-Pick disease type C. Orphanet J. Rare Dis. 2010;5:16. doi: 10.1186/1750-1172-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ko D.C., Milenkovic L., Beier S.M., Manuel H., Buchanan J., Scott M.P. Cell-Autonomous Death of Cerebellar Purkinje Neurons with Autophagy in Niemann-Pick Type C Disease. PLoS Genet. 2005;1 doi: 10.1371/journal.pgen.0010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lopez M.E., Klein A.D., Dimbil U.J., Scott M.P. Anatomically defined neuron-based rescue of neurodegenerative Niemann-Pick type C disorder. J. Neurosci. 2011;31:4367–4378. doi: 10.1523/JNEUROSCI.5981-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang M., Strnatka D., Donohue C., Hallows J.L., Vincent I., Erickson R.P. Astrocyte-only Npc1 reduces neuronal cholesterol and triples life span of Npc1–/–mice. J. Neurosci. Res. 2008;86:2848–2856. doi: 10.1002/jnr.21730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Borbon I., Totenhagen J., Fiorenza M.T., Canterini S., Ke W., Trouard T., Erickson R.P. Niemann-Pick C1 mice, a model of “juvenile Alzheimer’s disease”, with normal gene expression in neurons and fibrillary astrocytes show long term survival and delayed neurodegeneration. J. Alzheimers Dis. 2012;30:875–887. doi: 10.3233/JAD-2012-120199. [DOI] [PubMed] [Google Scholar]
- 69.Chen G., Li H.-M., Chen Y.-R., Gu X.-S., Duan S. Decreased estradiol release from astrocytes contributes to the neurodegeneration in a mouse model of Niemann-Pick disease type C. Glia. 2007;55:1509–1518. doi: 10.1002/glia.20563. [DOI] [PubMed] [Google Scholar]
- 70.Buard I., Steinmetz C.C., Claudepierre T., Pfrieger F.W. Glial cells promote dendrite formation and the reception of synaptic input in Purkinje cells from postnatal mice. Glia. 2010;58:538–545. doi: 10.1002/glia.20943. [DOI] [PubMed] [Google Scholar]
- 71.McCullough S.D., Xu X., Dent S.Y.R., Bekiranov S., Roeder R.G., Grant P.A. Reelin is a target of polyglutamine expanded ataxin-7 in human spinocerebellar ataxia type 7 (SCA7) astrocytes. Proc. Natl. Acad. Sci. USA. 2012;109:21319–21324. doi: 10.1073/pnas.1218331110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Murru S., Hess S., Barth E., Almajan E.R., Schatton D., Hermans S., Brodesser S., Langer T., Kloppenburg P., Rugarli E.I., et al. Astrocyte-specific deletion of the mitochondrial m-AAA protease reveals glial contribution to neurodegeneration. Glia. 2019;67:1526–1541. doi: 10.1002/glia.23626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Switonski P.M., Szlachcic W.J., Krzyzosiak W.J., Figiel M. A new humanized ataxin-3 knock-in mouse model combines the genetic features, pathogenesis of neurons and glia and late disease onset of SCA3/MJD. Neurobiol. Dis. 2015;73:174–188. doi: 10.1016/j.nbd.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 74.Seki T., Sato M., Kibe Y., Ohta T., Oshima M., Konno A., Hirai H., Kurauchi Y., Hisatsune A., Katsuki H., et al. Lysosomal dysfunction and early glial activation are involved in the pathogenesis of spinocerebellar ataxia type 21 caused by mutant transmembrane protein 240. Neurobiol. Dis. 2018;120:34–50. doi: 10.1016/j.nbd.2018.08.022. [DOI] [PubMed] [Google Scholar]
- 75.Cvetanovic M., Ingram M., Orr H., Opal P. Early activation of microglia and astrocytes in mouse models of spinocerebellar ataxia type 1. Neuroscience. 2015;289:289–299. doi: 10.1016/j.neuroscience.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kim J.H., Lukowicz A., Qu W., Johnson A., Cvetanovic M. Astroglia contribute to the pathogenesis of spinocerebellar ataxia Type 1 (SCA1) in a biphasic, stage-of-disease specific manner. Glia. 2018;66:1972–1987. doi: 10.1002/glia.23451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mellesmoen A., Sheeler C., Ferro A., Rainwater O., Cvetanovic M. Brain Derived Neurotrophic Factor (BDNF) Delays Onset of Pathogenesis in Transgenic Mouse Model of Spinocerebellar Ataxia Type 1 (SCA1) Front. Cell. Neurosci. 2018;12:509. doi: 10.3389/fncel.2018.00509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lattke M., Reichel S.N., Magnutzki A., Abaei A., Rasche V., Walther P., Calado D.P., Ferger B., Wirth T., Baumann B., et al. Transient IKK2 activation in astrocytes initiates selective non-cell-autonomous neurodegeneration. Mol. Neurodegener. 2017;12:16. doi: 10.1186/s13024-017-0157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Aikawa T., Mogushi K., Iijima-Tsutsui K., Ishikawa K., Sakurai M., Tanaka H., Mizusawa H., Watase K. Loss of MyD88 alters neuroinflammatory response and attenuates early Purkinje cell loss in a spinocerebellar ataxia type 6 mouse model. Hum. Mol. Genet. 2015;24:4780–4791. doi: 10.1093/hmg/ddv202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zamanian J.L., Xu L., Foo L.C., Nouri N., Zhou L., Giffard R.G., Barres B.A. Genomic analysis of reactive astrogliosis. J. Neurosci. 2012;2:6391–6410. doi: 10.1523/JNEUROSCI.6221-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liddelow S.A., Guttenplan K.A., Clarke L.E., Bennett F.C., Bohlen C.J., Schirmer L., Bennett M.L., Münch A.E., Chung W.-S., Peterson T.C., et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541:481–487. doi: 10.1038/nature21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Miller S.J. Astrocyte Heterogeneity in the Adult Central Nervous System. Front. Cell. Neurosci. 2018;12:401. doi: 10.3389/fncel.2018.00401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Giovannoni R., Maggio N., Rosaria Bianco M., Cavaliere C., Cirillo G., Lavitrano M., Papa M. Reactive astrocytosis and glial glutamate transporter clustering are early changes in a spinocerebellar ataxia type 1 transgenic mouse model. Neuron Glia Biol. 2007;3:335–351. doi: 10.1017/S1740925X08000185. [DOI] [PubMed] [Google Scholar]
- 84.Perkins E.M., Clarkson Y.L., Sabatier N., Longhurst D.M., Millward C.P., Jack J., Toraiwa J., Watanabe M., Rothstein J.D., Lyndon A.R., et al. Loss of beta-III spectrin leads to Purkinje cell dysfunction recapitulating the behavior and neuropathology of spinocerebellar ataxia type 5 in humans. J. Neurosci. 2010;30:4857–4867. doi: 10.1523/JNEUROSCI.6065-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Perkins E.M., Suminaite D., Clarkson Y.L., Lee S.K., Lyndon A.R., Rothstein J.D., Wyllie D.J.A., Tanaka K., Jackson M. Posterior cerebellar Purkinje cells in an SCA5/SPARCA1 mouse model are especially vulnerable to the synergistic effect of loss of β-III spectrin and GLAST. Hum. Mol. Genet. 2016;25:4448–4461. doi: 10.1093/hmg/ddw274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Perkins E.M., Clarkson Y.L., Suminaite D., Lyndon A.R., Tanaka K., Rothstein J.D., Skehel P.A., Wyllie D.J.A., Jackson M. Loss of cerebellar glutamate transporters EAAT4 and GLAST differentially affects the spontaneous firing pattern and survival of Purkinje cells. Hum. Mol. Genet. 2018;27:2614–2627. doi: 10.1093/hmg/ddy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chuang C.-Y., Yang C.-C., Soong B.-W., Yu C.-Y., Chen S.-H., Huang H.-P., Kuo H.-C. Modeling spinocerebellar ataxias 2 and 3 with iPSCs reveals a role for glutamate in disease pathology. Sci. Rep. 2019;9:1166. doi: 10.1038/s41598-018-37774-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Watase K., Hashimoto K., Kano M., Yamada K., Watanabe M., Inoue Y., Okuyama S., Sakagawa T., Ogawa S., Kawashima N., et al. Motor discoordination and increased susceptibility to cerebellar injury in GLAST mutant mice. Eur. J. Neurosci. 1998;10:976–988. doi: 10.1046/j.1460-9568.1998.00108.x. [DOI] [PubMed] [Google Scholar]
- 89.Jen J.C., Wan J., Palos T.P., Howard B.D., Baloh R.W. Mutation in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology. 2005;65:529–534. doi: 10.1212/01.WNL.0000172638.58172.5a. [DOI] [PubMed] [Google Scholar]
- 90.de Vries B., Mamsa H., Stam A.H., Wan J., Bakker S.L.M., Vanmolkot K.R.J., Haan J., Terwindt G.M., Boon E.M.J., Howard B.D., et al. Episodic ataxia associated with EAAT1 mutation C186S affecting glutamate reuptake. Arch. Neurol. 2009;66:97–101. doi: 10.1001/archneurol.2008.535. [DOI] [PubMed] [Google Scholar]
- 91.Choi K.-D., Jen J.C., Choi S.Y., Shin J.-H., Kim H.-S., Kim H.-J., Kim J.-S., Choi J.-H. Late-onset episodic ataxia associated with SLC1A3 mutation. J. Hum. Genet. 2017;62:443–446. doi: 10.1038/jhg.2016.137. [DOI] [PubMed] [Google Scholar]
- 92.Choi K.-D., Kim J.-S., Kim H.-J., Jung I., Jeong S.-H., Lee S.-H., Kim D.U., Kim S.-H., Choi S.Y., Shin J.-H., et al. Genetic Variants Associated with Episodic Ataxia in Korea. Sci. Rep. 2017;7:13855. doi: 10.1038/s41598-017-14254-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Iwama K., Iwata A., Shiina M., Mitsuhashi S., Miyatake S., Takata A., Miyake N., Ogata K., Ito S., Mizuguchi T., et al. A novel mutation in SLC1A3 causes episodic ataxia. J. Hum. Genet. 2018;63:207–211. doi: 10.1038/s10038-017-0365-z. [DOI] [PubMed] [Google Scholar]
- 94.Sicot G., Servais L., Dinca D.M., Leroy A., Prigogine C., Medja F., Braz S.O., Huguet-Lachon A., Chhuon C., Nicole A., et al. Downregulation of the Glial GLT1 Glutamate Transporter and Purkinje Cell Dysfunction in a Mouse Model of Myotonic Dystrophy. Cell Rep. 2017;19:2718–2729. doi: 10.1016/j.celrep.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Winter N., Kovermann P., Fahlke C. A point mutation associated with episodic ataxia 6 increases glutamate transporter anion currents. (Pt 11)Brain. 2012;135:3416–3425. doi: 10.1093/brain/aws255. [DOI] [PubMed] [Google Scholar]
- 96.Pyle A., Smertenko T., Bargiela D., Griffin H., Duff J., Appleton M., Douroudis K., Pfeffer G., Santibanez-Koref M., Eglon G., et al. Exome sequencing in undiagnosed inherited and sporadic ataxias. (Pt 2)Brain. 2015;138:276–283. doi: 10.1093/brain/awu348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vig P.J.S., Lopez M.E., Wei J., D’Souza D.R., Subramony S., Henegar J., Fratkin J.D. Glial S100B Positive Vacuoles In Purkinje Cells: Earliest Morphological Abnormality In SCA1 Transgenic Mice. J. Neurol. Sci. Turk. 2006;23:166–174. doi: 10.1901/jaba.2006.23-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vig P.J.S., Shao Q., Subramony S.H., Lopez M.E., Safaya E. Bergmann glial S100B activates myo-inositol monophosphatase 1 and Co-localizes to purkinje cell vacuoles in SCA1 transgenic mice. Cerebellum. 2009;8:231–244. doi: 10.1007/s12311-009-0125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vig P.J.S., Hearst S., Shao Q., Lopez M.E., Murphy H.A., 2nd, Safaya E. Glial S100B protein modulates mutant ataxin-1 aggregation and toxicity: TRTK12 peptide, a potential candidate for SCA1 therapy. Cerebellum. 2011;10:254–266. doi: 10.1007/s12311-011-0262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Belozor O.S., Yakovleva D.A., Potapenko I.V, Shuvaev A.N., Smolnikova M.V, Vasilev A., Pozhilenkova E.A., Shuvaev A.N. Extracellular S100β Disrupts Bergman Glia Morphology and Synaptic Transmission in Cerebellar Purkinje Cells. Brain Sci. 2019;9:80. doi: 10.3390/brainsci9040080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Morquette P., Verdier D., Kadala A., Fethiere J., Philippe A.G., Robitaille R., Kolta A. An astrocyte-dependent mechanism for neuronal rhythmogenesis. Nat. Neurosci. 2015;18:844–854. doi: 10.1038/nn.4013. [DOI] [PubMed] [Google Scholar]
- 102.Zhou J., Lei L., Shi Y., Wang J., Jiang H., Shen L., Tang B. Serum concentrations of NSE and S100B in spinocerebellar ataxia type 3/Machado-Joseph disease. J. Cent. South Univ. Med. Sci. 2011;36:504–510. doi: 10.1007/s11771-011-0724-4. [DOI] [PubMed] [Google Scholar]
- 103.Untiet V., Kovermann P., Gerkau N.J., Gensch T., Rose C.R., Fahlke C. Glutamate transporter-associated anion channels adjust intracellular chloride concentrations during glial maturation. Glia. 2017;65:388–400. doi: 10.1002/glia.23098. [DOI] [PubMed] [Google Scholar]
- 104.Parinejad N., Peco E., Ferreira T., Stacey S.M., van Meyel D.J. Disruption of an EAAT-Mediated Chloride Channel in a Drosophila Model of Ataxia. J. Neurosci. 2016;36:7640–7647. doi: 10.1523/JNEUROSCI.0197-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kovermann P., Untiet V., Kolobkova Y., Fahlke C. Increased activity of glial glutamate transporter-associated anion channels results in episodic ataxia 6. Glia. 2019;67:E216. doi: 10.1002/glia.23675. [DOI] [Google Scholar]
- 106.Desagher S., Glowinski J., Premont J. Astrocytes protect neurons from hydrogen peroxide toxicity. J. Neurosci. 1996;16:2553–2562. doi: 10.1523/JNEUROSCI.16-08-02553.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chen Y., Vartiainen N.E., Ying W., Chan P.H., Koistinaho J., Swanson R.A. Astrocytes protect neurons from nitric oxide toxicity by a glutathione-dependent mechanism. J. Neurochem. 2001;77:1601–1610. doi: 10.1046/j.1471-4159.2001.00374.x. [DOI] [PubMed] [Google Scholar]
- 108.Shih A.Y., Johnson D.A., Wong G., Kraft A.D., Jiang L., Erb H., Johnson J.A., Murphy T.H. Coordinate Regulation of Glutathione Biosynthesis and Release by Nrf2-Expressing Glia Potently Protects Neurons from Oxidative Stress. J. Neurosci. 2003;23:3394–3406. doi: 10.1523/JNEUROSCI.23-08-03394.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.González-Reyes R.E., Nava-Mesa M.O., Vargas-Sánchez K., Ariza-Salamanca D., Mora-Muñoz L. Involvement of Astrocytes in Alzheimer’s Disease from a Neuroinflammatory and Oxidative Stress Perspective. Front. Mol. Neurosci. 2017;10:427. doi: 10.3389/fnmol.2017.00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rizor A., Pajarillo E., Johnson J., Aschner M., Lee E. Astrocytic Oxidative/Nitrosative Stress Contributes to Parkinson’s Disease Pathogenesis: The Dual Role of Reactive Astrocytes. Antioxidants. 2019;8:265. doi: 10.3390/antiox8080265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen P., Peng C., Luff J., Spring K., Watters D., Bottle S., Furuya S., Lavin M.F. Oxidative Stress Is Responsible for Deficient Survival and Dendritogenesis in Purkinje Neurons from Ataxia-Telangiectasia Mutated Mutant Mice. J. Neurosci. 2003;23:11453–11460. doi: 10.1523/JNEUROSCI.23-36-11453.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu N., Stoica G., Yan M., Scofield V.L., Qiang W., Lynn W.S., Wong P.K.Y. ATM deficiency induces oxidative stress and endoplasmic reticulum stress in astrocytes. Lab. Investig. 2005;85:1471–1480. doi: 10.1038/labinvest.3700354. [DOI] [PubMed] [Google Scholar]
- 113.Kim J., Wong P.K.Y. Oxidative stress is linked to ERK1/2-p16 signaling-mediated growth defect in ATM-deficient astrocytes. J. Biol. Chem. 2009;284:14396–14404. doi: 10.1074/jbc.M808116200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Campbell A., Bushman J., Munger J., Noble M., Pröschel C., Mayer-Pröschel M. Mutation of ataxia–telangiectasia mutated is associated with dysfunctional glutathione homeostasis in cerebellar astroglia. Glia. 2016;64:227–239. doi: 10.1002/glia.22925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Navarro J.A., Botella J.A., Metzendorf C., Lind M.I., Schneuwly S. Mitoferrin modulates iron toxicity in a Drosophila model of Friedreich’s ataxia. Free Radic. Biol. Med. 2015;85:71–82. doi: 10.1016/j.freeradbiomed.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 116.Edenharter O., Schneuwly S., Navarro J.A. Mitofusin-Dependent ER Stress Triggers Glial Dysfunction and Nervous System Degeneration in a Drosophila Model of Friedreich’s Ataxia. Front. Mol. Neurosci. 2018;11:38. doi: 10.3389/fnmol.2018.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kotagal V. Acetazolamide-responsive ataxia. Semin. Neurol. 2012;32:533–537. doi: 10.1055/s-0033-1334475. [DOI] [PubMed] [Google Scholar]
- 118.Shiwaku H., Yagishita S., Eishi Y., Okazawa H. Bergmann glia are reduced in spinocerebellar ataxia type 1. Neuroreport. 2013;24:620–625. doi: 10.1097/WNR.0b013e32836347b7. [DOI] [PubMed] [Google Scholar]
- 119.Maltecca F., Baseggio E., Consolato F., Mazza D., Podini P., Young S.M.J., Drago I., Bahr B.A., Puliti A., Codazzi F., et al. Purkinje neuron Ca2+ influx reduction rescues ataxia in SCA28 model. J. Clin. Investig. 2015;125:263–274. doi: 10.1172/JCI74770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chen P.-C., Vargas M.R., Pani A.K., Smeyne R.J., Johnson D.A., Kan Y.W., Johnson J.A. Nrf2-mediated neuroprotection in the MPTP mouse model of Parkinson’s disease: Critical role for the astrocyte. Proc. Natl. Acad. Sci. USA. 2009;106:2933–2938. doi: 10.1073/pnas.0813361106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vargas M.R., Johnson D.A., Sirkis D.W., Messing A., Johnson J.A. Nrf2 activation in astrocytes protects against neurodegeneration in mouse models of familial amyotrophic lateral sclerosis. J. Neurosci. 2008;28:13574–13581. doi: 10.1523/JNEUROSCI.4099-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cabantchik Z.I., Munnich A., Youdim M.B., Devos D. Regional siderosis: A new challenge for iron chelation therapy. Front. Pharmacol. 2013;4:167. doi: 10.3389/fphar.2013.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Franco C., Fernández S., Torres-Alemán I. Frataxin deficiency unveils cell-context dependent actions of insulin-like growth factor I on neurons. Mol. Neurodegener. 2012;7:51. doi: 10.1186/1750-1326-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McLoughlin H.S., Moore L.R., Chopra R., Komlo R., McKenzie M., Blumenstein K.G., Zhao H., Kordasiewicz H.B., Shakkottai V.G., Paulson H.L., et al. Oligonucleotide therapy mitigates disease in spinocerebellar ataxia type 3 mice. Ann. Neurol. 2018;84:64–77. doi: 10.1002/ana.25264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bon C., Luffarelli R., Russo R., Fortuni S., Pierattini B., Santulli C., Fimiani C., Persichetti F., Cotella D., Mallamaci A., et al. SINEUP non-coding RNAs rescue defective frataxin expression and activity in a cellular model of Friedreich’s Ataxia. Nucleic Acids Res. 2019;47:10728–10743. doi: 10.1093/nar/gkz798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mitoma H., Buffo A., Gelfo F., Guell X., Fucà E., Kakei S., Lee J., Manto M., Petrosini L., Shaikh A.G., et al. Consensus Paper. Cerebellar Reserve: From Cerebellar Physiology to Cerebellar Disorders. Cerebellum. 2020;19:131–153. doi: 10.1007/s12311-019-01091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bylicky M.A., Mueller G.P., Day R.M. Mechanisms of Endogenous Neuroprotective Effects of Astrocytes in Brain Injury. Oxid Med. Cell Longev. 2018;2018:6501031. doi: 10.1155/2018/6501031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mattugini N., Bocchi R., Scheuss V., Russo G.L., Torper O., Lao C.L., Götz M. Inducing Different Neuronal Subtypes from Astrocytes in the Injured Mouse Cerebral Cortex. Neuron. 2019;103:1086.e5–1095.e5. doi: 10.1016/j.neuron.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wojcinski A., Lawton A.K., Bayin N.S., Lao Z., Stephen D.N., Joyner A.L. Cerebellar granule cell replenishment postinjury by adaptive reprogramming of Nestin + progenitors. Nat. Neurosci. 2017;20:1361–1370. doi: 10.1038/nn.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Quek H., Luff J., Cheung K., Kozlov S., Gatei M., Lee C.S., Bellingham M.C., Noakes P.G., Lim Y.C., Barnett N.L., et al. A rat model of ataxia-telangiectasia: Evidence for a neurodegenerative phenotype. Hum. Mol. Genet. 2016;26:109–123. doi: 10.1093/hmg/ddw371. [DOI] [PubMed] [Google Scholar]
- 131.Miranda C.J., Santos M.M., Ohshima K., Smith J., Li L., Bunting M., Cossée M., Koenig M., Sequeiros J., Kaplan J., et al. Frataxin knockin mouse. FEBS Lett. 2002;512:291–297. doi: 10.1016/S0014-5793(02)02251-2. [DOI] [PubMed] [Google Scholar]
- 132.Coppola G., Choi S.-H., Santos M.M., Miranda C.J., Tentler D., Wexler E.M., Pandolfo M., Geschwind D.H. Gene expression profiling in frataxin deficient mice: Microarray evidence for significant expression changes without detectable neurodegeneration. Neurobiol. Dis. 2006;22:302–311. doi: 10.1016/j.nbd.2005.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lorenzetti D., Watase K., Xu B., Matzuk M.M., Orr H.T., Zoghbi H.Y. Repeat instability and motor incoordination in mice with a targeted expanded CAG repeat in the Sca1 locus. Hum. Mol. Genet. 2000;9:779–785. doi: 10.1093/hmg/9.5.779. [DOI] [PubMed] [Google Scholar]
- 134.Wu Y.-Y., Chiu F.-L., Yeh C.-S., Kuo H.-C. Opportunities and challenges for the use of induced pluripotent stem cells in modelling neurodegenerative disease. Open Biol. 2019;9:180177. doi: 10.1098/rsob.180177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mariani J.N., Zou L., Goldman S.A. Human Glial Chimeric Mice to Define the Role of Glial Pathology in Human Disease. Methods Mol. Biol. 2019;1936:311–331. doi: 10.1007/978-1-4939-9072-6_18. [DOI] [PMC free article] [PubMed] [Google Scholar]