Figure 1.
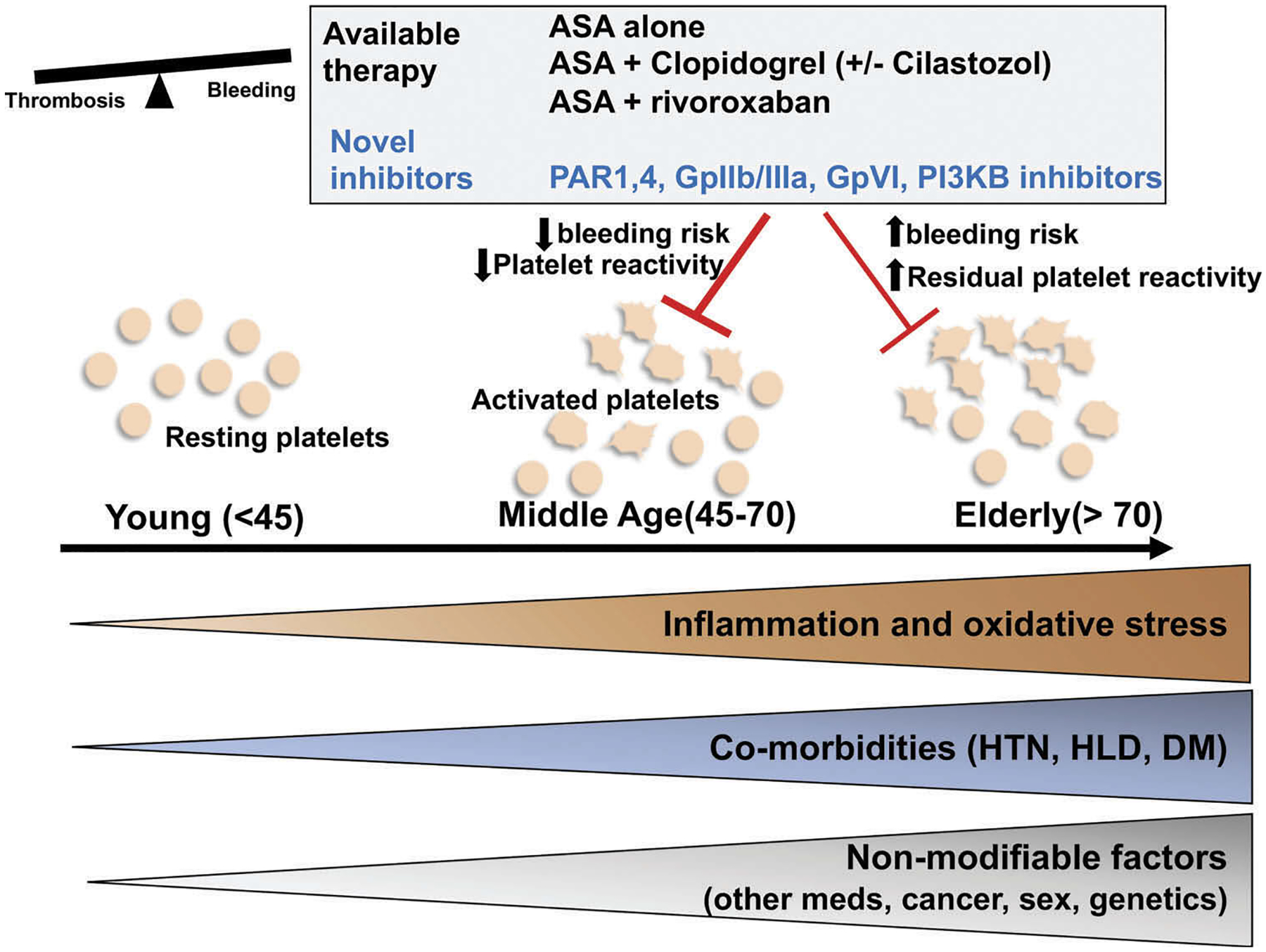
Risk factors associated with aging driving platelet activation and increased thrombotic susceptibility: therapeutic alternatives. Aging is associated with increased inflammation and oxidative stress that can affect platelet activation and aggregation. Other age-associated co-morbidities, such as hypertension, diabetes, and hypercholesterolemia can affect platelet metabolism and can heighten the inflammatory micro-environment. Less modifiable risk factors, such as sex, presence of malignancy, genetics, and multiple medication use for age-associated comorbidities can affect platelets through yet undescribed mechanisms. This can culminate in a reduced threshold for platelet activation. The use of antiplatelet medications requires balancing the risk of bleeding with the risk of thrombosis. Current therapies, such as aspirin (ASA) and clopidogrel target the COX-2/thromboxane and ADP-mediated pathways, respectively. These may be ineffective in the elderly population as platelets become more sensitive to agonists and have a higher bleeding risk. Other approved but less studied treatments include combination of ASA and cilostazol or factor Xa inhibitors (rivaroxaban). Other novel inhibitors targeting other platelet activation pathways that focus on inflammatory and hemostatic signaling are in clinical trials and may offer more beneficial therapy options to the aging population. Future trials should focus on the elderly population where the risks of bleeding and anti-thrombotic benefits need careful assessment (HTN = hypertension, HLD = hyperlipidemia, DM = diabetes mellitus, PAR = protease-activating receptor, PI3KB = phosphoinositide 3 kinase, ASA = aspirin).
