ABSTRACT
Background: While evidence is growing for the efficacy of trauma-focused mental health interventions in low- and middle-income countries, concerns have been raised about whether these types of interventions can be effectively delivered in contexts with ongoing conflict and violence. Cognitive Processing Therapy (CPT) has been shown to be effective in reducing sexual violence survivors’ psychological symptoms in eastern Democratic Republic of the Congo (DRC), a region with a history of chronic conflict.
Objective: The purpose of the present study is to assess the degree to which exposure to different levels of ongoing insecurity impacts effectiveness of an evidence-based trauma-focused psychotherapy for sexual violence survivors.
Method: Participants were 158 female sexual violence survivors receiving CPT in seven communities in South Kivu. Participants completed weekly assessments of their symptoms of PTSD and depression as part of CPT. Degree of site insecurity was categorized as high or low levels of ongoing insecurity based on information collected from supervisors and clinicians. Hierarchical linear modelling was used to examine change over time moderated by level of insecurity at the site.
Results: Overall, women reported a significant reduction in psychological symptoms over time (b = −2.04, p <.001). Residing in a site of greater insecurity was associated with higher initial symptoms (b = 5.91, p <.01), but similar improvement over time (b = −0.30, p =.10) compared to women living in relatively more secure sites. High rates of attendance and treatment completion were observed.
Conclusions: These results support the effectiveness of trauma-focused therapies when provided in a well-structured and well-supervised program even in contexts of ongoing conflict and violence.
KEYWORDS: Sexual assault, psychological symptoms, randomized controlled trial, sexual violence, cognitive processing therapy
Antecedentes: Mientras que existe evidencia creciente sobre la eficacia de las intervenciones en salud mental enfocadas en trauma en países de escasos y medianos ingresos, existe preocupación sobre si este tipo de intervenciones pueden ser realizadas de manera efectiva en contextos en los que aún existen conflictos y violencia. La Terapia de Procesamiento Cognitivo (CPT, por sus siglas en inglés) ha mostrado ser efectiva en reducir los síntomas psicológicos de sobrevivientes a violencia sexual en la zona oriental de la República Democrática del Congo, una región con una historia de conflicto crónico.
Objetivo: El propósito del presente estudio es evaluar el grado en el que la exposición a diferentes niveles de inseguridad en el entorno ejerce un impacto sobre la efectividad de una psicoterapia enfocada en trauma y basada en evidencias para sobrevivientes a violencia sexual.
Método: Las participantes fueron 158 sobrevivientes a violencia sexual recibiendo CPT en siete comunidades en Kivu del Sur. Las participantes completaron evaluaciones semanales sobre síntomas de trastorno de estrés postraumático y depresión como parte de la CPT. El grado de inseguridad del entorno fue categorizado en niveles de inseguridad continua altos o bajos según la información proporcionada por supervisores y terapeutas.
Resultados: Se empleó un modelo de regresión linear jerárquica para evaluar el cambio en el tiempo modulado por el nivel de inseguridad del entorno. En general, las mujeres reportaron una reducción significativa en los síntomas psicológicos en el tiempo (b = −2.04, p <.001). El vivir en un entorno de mayor inseguridad se asoció a síntomas iniciales más altos (b = 5.91, p <.01) pero a una mejoría similar en el tiempo (b = −0.30, p =.10) comparado con mujeres viviendo en entornos relativamente más seguros.
Conclusiones: Estos resultados apoyan la efectividad de las terapias enfocadas en trauma al ser brindadas en programas bien estructurados y bien supervisados incluso en contextos de conflicto y violencia en curso.
PALABRAS CLAVE: Violación, ensayo clínico aleatorizado, terapia de procesamiento cognitivo, violencia basada en género, trastorno de estrés postraumático, República Democrática del Congo
HIGHLIGHTS: • Survivors of sexual gender based violence can benefit from time-limited trauma-focused therapy even in high conflict settings.
背景:虽然越来越多的证据表明中低收入国家中聚焦创伤的心理健康干预措施的有效性, 但人们也更加担心在持续冲突和暴力的情况下, 能否有效提供这类干预措施。在具有长期冲突历史的刚果民主共和国东部地区, 认知加工疗法 (CPT) 已被证明可有效减少性暴力幸存者的心理症状。
目标:本研究旨在评估对于性暴力幸存者, 不同水平持续不安全暴露对循证的聚焦创伤心理治疗效果的影响程度。
方法:参与者是南基伍省七个社区接受CPT的158名女性性暴力幸存者。参与者每周完成作为CPT一部分的PTSD及抑郁症状的评估。根据从监管者和临床医生处收集到的信息, 将地区的不安全程度分为高水平持续不安全或低水平持续不安全。
结果:分层线性模型用于考查受地区不安全程度调节的随时间的变化。总体而言, 女性报告了随时间推移心理症状的显著减少 (b = −2.04, p<.001) 。相较于生活在相对较安全地区的妇女, 居住在较不安全地区与较高的初始症状相关 (b = 5.91, p<.01), 但随时间的改善程度相似 (b = −0.30, p=.10) 。
结论:这些结果支持了即使在持续冲突和暴力的情况下, 如果以结构合理, 监督良好的方案提供治疗, 聚焦创伤疗法具备有效性。
关键词: 性侵害, 随机临床试验, 认知加工疗法, 基于性别的性暴力, 创伤后应激障碍, 刚果民主共和国
Multiple forms of psychopathology, including depression, suicidal ideation, anxiety disorders, and posttraumatic stress disorder (PTSD), are well documented in conflict-affected populations (Johnson et al., 2008, 2010; Steel et al., 2009). Increasingly, efforts to reduce global mental health disparities have led to calls for the implementation of evidence-based treatments in settings with active war, conflict, or other security issues where needs are great (World Health Organization [WHO], 2010). However, psychological treatments with demonstrated effectiveness in high-income countries may be more challenging to deliver in populations exposed to mass conflict and displacement due to ongoing exposure to trauma and other major stressors (O’Callaghan, McMullen, Shannon, Rafferty, & Black, 2013). Beyond the basic practicality of how to deliver psychotherapy services in conflict-affected areas, it is unclear whether clients who are at ongoing risk of re-traumatization can benefit from trauma-focused psychotherapy (Wangelin & Tuerk, 2014). Little guidance exists regarding the feasibility and effectiveness of delivering treatments in these settings. To understand how insecurity stemming from ongoing conflict may impact delivery and effectiveness of a trauma-focused psychotherapy, the present study examines the degree to which ongoing insecurity impacted the implementation and effectiveness of Cognitive Processing Therapy (CPT) delivered to sexual violence survivors in conflict-affected areas of eastern Democratic Republic of the Congo (DRC).
The DRC is the site of the deadliest conflict since World War II and has undergone continued violence and civil war for decades (Coghan et al., 2007). As a result, more than 4.5 million Congolese were internally displaced as of 2017, and more than 811,300 had fled to neighbouring countries as of 2018 (UNHCR, 2019). Sexual violence, mainly targeted at women and girls, has been commonly used as a tool and experienced as an effect of armed conflict in Eastern DRC (Duroch, McRae, & Grais, 2011; Steiner et al., 2009). One estimate from a large population-based survey in Eastern DRC found roughly 40% of women in these conflict-affected areas reported experiencing sexual violence (Johnson et al., 2010). Sexual violence is a well-documented risk factor for many mental disorders, including PTSD and depression (Dworkin, 2018; Dworkin, Menon, Bystrynski, & Allen, 2017). In the same large population-based survey, 50% of the population met symptom criteria for PTSD and 41% for major depressive disorder (Johnson et al., 2010).
For these types of mental health conditions, The Mental Health Gap Action Programme (mhGAP) recommends individual and group Cognitive Behavioural Therapy (CBT) with a trauma focus or with eye movement desensitization reprocessing (Tol, Barbui, & van Ommeren, 2013; World Health Organisation, 2013) for treatment of PTSD in global settings where trained and supervised therapists are available. However, the mhGAP recommendations state that these interventions ‘should be considered when the person is within a safe environment, i.e. there are no ongoing traumatic events and the person is not at imminent risk of further exposure to traumatic events’ (WHO, 2013, p. 10). The guidelines point out that uncertainty remains among experts regarding to what extent these types of trauma-focused treatments can be delivered appropriately in settings of ongoing armed violence (Murray et al., 2014). Feasibility challenges include having to cancel therapy or supervision sessions for safety reasons, exposure of providers to unsafe conditions that could precipitate or exacerbate their own mental health problems and interfere with their ability to provide efficacious treatment, and session time being reallocated to safety planning. Continuous trauma exposure may also impose logistical barriers to patients’ ability to attend sessions, pay attention in sessions, and complete between session practice.
It is also unclear how beneficial therapy may be to patients even when optimally delivered if they are living in contexts of ongoing trauma. Although a common goal of PTSD treatment is to reduce ‘false alarm’ responses conditioned by a threat that is no longer present, people at risk of ongoing trauma exposure may, by necessity, experience a consistently elevated state of arousal in response to true threats (Eagle & Kaminer, 2013; Nuttman-Shwartz & Shoval-Zuckerman, 2016). Despite these concerns, there is increasing interest in delivering evidence-based psychotherapies for trauma-related mental health problems to people at risk of ongoing trauma exposure, including soldiers deployed in a combat setting (McLay, McBrien, Wiederhold, & Wiederhold, 2010; Wangelin & Tuerk, 2014), women in abusive relationships (Iverson, Resick, Suvak, & Taft, 2012), people in settings affected by natural disaster where threat of harm continues (Hobfoll et al., 2007), and children exposed to ongoing community (Stein et al., 2003) or family violence (Bryant et al., 2017; Cohen, Mannarino, & Iyengar, 2011; Murray, Cohen, & Mannarino, 2013).
Researchers have examined the feasibility and effectiveness of mental health and psychosocial support interventions in settings with elevated risk for trauma exposure, but there is a paucity of rigorous studies on how ongoing conflict affects outcomes, and little research has addressed trauma-focused psychotherapy specifically (Asgary, Emery, & Wong, 2013). A review of the feasibility of psychotherapy for sexual trauma in the context of armed violence noted the lack of research in this area, although results of the studies reviewed suggested that symptom improvement was possible even in the context of ongoing conflict (Tol et al., 2013). In one of the few studies of trauma-focused psychotherapy in an active conflict setting, 91 patients with PTSD resulting from a car bomb received cognitive therapy, and improvements were observed even though more than 60 hoax or false alarm bomb threats were received and publicized during the course of the study (Gillespie, Duffy, Hackmann, & Clark, 2002). A subsequent randomized controlled trial in this setting found a drop-out rate of 20%, which the authors attributed in part to ongoing conflict (Duffy, Gillespie, & Clark, 2007). More recent rigorous controlled trials investigating trauma-based psychotherapy in areas of ongoing conflict have been published and have found that these therapies are both well tolerated and effective (O’Callaghan et al., 2013; Weiss et al., 2015). Given heterogeneity in exposure and the dynamic nature of conflict, it remains unclear how different levels of exposure to ongoing trauma affect patients’ outcomes in trauma-focused psychotherapy within these settings. Testing this question could help to inform decision-making about the appropriate timing of trauma-focused treatment.
The purpose of the present study is to assess the degree to which exposure to different levels of ongoing insecurity impacts effectiveness of an evidence-based trauma-focused psychotherapy for sexual violence survivors. Specifically, we examine whether women receiving treatment in sites categorized as being in areas of relative high-insecurity experienced differential impacts of the CPT program compared to women in sites categorized as being in areas of relative low insecurity. We hypothesized higher levels of insecurity would be associated with higher initial symptom presentations. We also hypothesized both groups would improve over time, but improvements would be more pronounced among women living in relatively more secure areas.
1. Methods
This study uses data from the CPT arm of a larger randomized-controlled trial implemented to evaluate the effectiveness of CPT compared with individual support for sexual violence survivors in eastern DRC (Bass et al., 2013).
1.1. Participants
Fifteen rural sites in South Kivu province, eastern DRC (hereafter referred to as ‘sites’) were included in the original trial. Selection of study sites was based on accessibility and availability of a psychosocial assistant (PSA) to provide services for the duration of the trial. Seven sites were randomized to the CPT condition and were included in the current analysis. All PSAs had experience providing basic individual support and case management services for sexual violence survivors prior to receiving training in CPT.
Study recruitment occurred in December 2010, 3 months prior to the initiation of CPT. The PSAs identified potentially eligible women through a review of current and prior client files from their ongoing psychosocial program for survivors. Study eligibility included being age 18 years or older and report of: (a) having personally experienced and/or witnessed sexual violence; (b) having significant psychological symptoms, defined as a score of at least 55 on a combined measure of trauma, depression and anxiety (see measure section below); and, having (c) some impairment in daily functioning, defined as a score of at least 10 (i.e. dysfunction on at least half the activities) on a locally developed measure (Bass et al., 2013). Of the women included in the CPT groups who had personally experienced sexual violence, 12 said the assault was perpetrated by someone they knew (8%). Although not formally assessed, participants’ physical safety was monitored throughout the treatment and addressed as a clinical issue in cases of intimate partner violence.
Women were excluded from the trial if they reported suicidality that was judged by clinical staff to require immediate treatment. Eligible women were invited to an NGO-sponsored ‘listening centre’ where Congolese research assistants implemented the consent process and administered the study questionnaire. Interviews continued until 28–30 eligible women were identified at each site.
1.2. Procedures
PSAs at each study site provided 12 sessions of CPT to 3 concurrent groups of 6–8 women over a 4-month period. The Johns Hopkins Bloomberg School of Public Health and the Kinshasa School of Public Health Institutional Review Boards provided ethical approval. All study participants provided oral informed consent.
1.2.1. Cognitive Processing Therapy
CPT is a structured, manualized therapy with evidence of effectiveness for treating depression, anxiety, and PTSD among survivors of sexual violence (Resick et al., 2008; Vickerman & Margolin, 2009). Originally developed as a group intervention, CPT provides participants with skills to recognize maladaptive beliefs they have related to the trauma and learn to challenge those beliefs, thereby reducing negative emotions. Through discussing the trauma and these maladaptive beliefs, participants are thought to process emotions regarding the traumatic event, reduce avoidance of trauma-related cues and reminders, reformulate feelings and thoughts about the event, and cope better with daily challenges (Resnick & Schnicke, 1992).
For this study, CPT was comprised of one individual session lasting 1 h and eleven weekly 2-h sessions with 6–8 women per treatment group. The standard CPT treatment model was modified in several ways to better fit the Congolese culture, treatment delivery by paraprofessionals (psychosocial assistants), and high levels of client illiteracy. For example, an individual meeting was included at the beginning of treatment to provide the client with more information about what talk therapy is and explaining the intervention process in general. Specific content adaptations how to address beliefs about sexual assault’s impact on women’s social status, including providing locally relevant examples of stuck points (‘Since the rape, I don’t have a voice in my house’). We also provided more basic skills to the psychosocial assistants on how to conduct group psychotherapy. To address high rates of illiteracy, we changed language around ‘homework,’ reducing psychological jargon and simplifying CPT skills so that the steps could be memorized. Efforts to increase accessibility for low literacy participants also included reducing the number of ‘challenging questions’ from 10 to 4 to facilitate memorization of skills, and removing one CPT skill (patterns of problematic thinking). A detailed description of adaptations made and the adaptation process in available as a supplement to the original clinical trial (Bass et al., 2013, https://tinyurl.com/vt72en4).
The psychosocial assistants received 2 weeks of in-person training with US-based CPT trainers using the materials adapted for the eastern DRC context and translated into French. After training, supervision was provided through a two-tiered structure. Tier 1 was comprised of Congolese psychosocial supervisors provided direct supervision through weekly phone/in person meetings with the PSAs. In Tier 2, a US-trained clinical social worker (bilingual in English and French) provided on-site clinical oversight and supervision to the supervisors while maintaining weekly phone contact with the US-based trainers who provided additional support and quality assurance.
1.3. Providers
The PSAs trained to provide CPT were all women who were residents of the communities they were serving. Each had at least 4 years of post-primary-school education. They also had between 1 and 9 years of experience providing case management and individual supportive counselling to survivors of sexual violence and had undergone a 5–6 day training session conducted by the International Rescue Committee (our implementing partner) in case management, prior to participating in the CPT training. The case management training included information on counselling, family mediation, stress management, and clinical care of survivors.
1.4. Baseline measures
The study questionnaire was translated into five local languages (Kibembe, Kifuliro, Kihavu, Mashi, and Swahili) and included sections on demographics, trauma exposure, daily functioning, and psychosocial and mental health problems.
1.4.1. Demographics
Participants self-reported their age, language, marital status, the total number of people living in their household, and whether they had lived in the same village for 10 years or more.
1.4.2. Daily functioning
Assessment of functional impairment was based on the degree of difficulty in performing 20 important tasks of daily living identified based on qualitative data from the study sites (Applied Mental Health Research Group, 2013a, 2013b). Participants were asked to rate the degree of difficulty in performing each task on a 5-point Likert scale (0 = no difficulty, 1 = little difficulty, 2 = a moderate amount of difficulty, 3 = a lot of difficulty, and 4 = often unable to perform the task). An average per-item score was generated for each participant, with scores ranging from 0 to 4 and higher scores indicating greater impairment.
1.4.3. Mental health
The Hopkins Symptom Checklist (HSCL-25) (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974) and the Harvard Trauma Questionnaire (HTQ) (Mollica et al., 1992) were adapted to assess for depression, anxiety, and PTSD symptoms based on a mixed-methods approach to fit the local context (Bass et al., 2013). Both the HSCL-25 and the HTQ have been used internationally and have strong psychometric properties. Participants were asked to rate how often they experienced each symptom in the prior 4 weeks using a Likert scale ranging from 0 (not at all) to 3 (a lot). The mental health section of the study questionnaire was comprised of a total of 55 symptoms that included the HSCL-25, HTQ, and 15 additional locally relevant symptoms identified during the qualitative instrument development phase of the study.
1.5. Session monitoring questionnaire: mental health symptoms
An 11-item scale of the mental health symptoms drawn from published instruments (Table 1) was used by PSAs to track changes in key symptoms from session-to-session. The 11 items were chosen as a subset of the larger 55-item measure based on the following guiding principles: (1) frequency of mention in prior qualitative interviews on problems faced by sexual violence survivors in Eastern DRC; (2) representation of key aspects of depression, anxiety, and PTSD; and (3) clinical management needs (e.g. tracking suicidality). Participants were asked to indicate the extent to which symptoms bothered them in the past week: 0 = ‘not a problem’, 1 = ‘a little problem’, 2 = ‘a medium problem’, or 3 = ‘a big problem’.
Table 1.
Mental health symptom scale.
| Item | Source |
|---|---|
| Feeling sad | HSCL depression subscale |
| Feeling lonely | HSCL depression subscale |
| Thoughts of ending your life | HSCL depression subscale |
| Worrying too much or feeling fearful | HSCL anxiety subscale |
| Spells of terror or panic | HSCL anxiety subscale |
| Recurrent thoughts/memories of the worst trauma | HTQ |
| Feeling on guard | HTQ |
| Avoiding activities that remind you of the traumatic or hurtful event | HTQ |
| Nightmares about the worst trauma | HTQ |
| Avoiding thoughts or memories about the traumatic or hurtful event | HTQ |
| Feeling guilty or ashamed | HTQ |
1.6. Site insecurity
Degree of site insecurity was categorized as high or low levels of ongoing insecurity. The coding of the level of insecurity at each of the seven study sites was based on information collected from the Congolese psychosocial supervisors and the PSAs. For each site, the supervisors were asked to report on the following information for the 4-month intervention period: 1) degree of ongoing presence or threat of presence of armed groups and 2) incidents of violence at the site. Insecurity was coded on the basis of these events, rather than on clients’ perceptions of insecurity (which might have been affected by symptoms of PTSD).
The degree to which armed groups occupied a given site or were able to easily access a site contributed heavily to the ratings of high insecurity, more so than distinct incidents of violence in the site. For example, two intervention sites neighboured an uninhabited national park where armed groups retreated for concealment. The easy access armed groups had to these sites caused frequent displacement of the local population, and even during periods of relative calm, served as a constant threat to residents. This led supervisors to rank these two sites as having high levels of insecurity. Conversely, at one site near a larger city, the presence and threat of an armed group were sporadic rather than constant and thus the supervisors ranked this site as having a low level of insecurity.
All sites reported at least one incident of violence during the 4-month intervention period. The nature of these events ranged in type and frequency and included site-wide attacks and looting, outbursts of fighting between armed groups that displaced populations into the forest, specific looting of individual homes or businesses, and kidnapping and attacks by armed groups on specific individuals leading to injury or death. During the study, four children living in the sites and one CPT group member were murdered. Supervisors indicated that site-wide attacks were the most impactful to women’s health and wellbeing due to the number of people affected, the fact that rape, murder and robberies would all take place at once, and the likelihood of displacement. Supervisors cited targeted murder and kidnapping as the next most serious incidents, as they caused general fear and grief among the site. These types of events were weighted more heavily in determining the overall level of insecurity.
Coding was completed prior to the initiation of data analyses. The supervisors agreed on the coding of insecurity for each site. Ultimately, three sites were identified as being relatively higher insecurity and four were identified as being relatively lower insecurity.
1.7. Analysis plan
To examine the influence of the site-level insecurity on participants’ symptom change over the course of the CPT intervention, we conducted multilevel-mixed effects linear regressions (i.e. hierarchical linear models; Raudenbush & Bryk, 2002) with all available data using maximum likelihood estimation. To account for the clustered nature of the data, four levels were specified with repeated weekly measures of mental health symptoms at each week of therapy at level 1, participants at level 2, and treatment groups at level 3, and site at level 4. Because there was only one PSA per site in this study, the fourth level also reflected the PSA in addition to the site.
We used a model-building approach in which we sequentially examined models that included random intercepts, then random slopes, and then alternative covariance structures (Singer & Willett, 2003). We compared each successive model to the one before using likelihood-ratio tests (Singer & Willett, 2003). Based on these tests, we determined that the best fitting model had random intercepts specified at each level; included a random slope for time (i.e. session) at the client level; and, used an unstructured covariance structure at the client level.
To examine our hypothesis that high levels of site insecurity would be associated with higher initial mental health symptoms, we first ran a model that included only the fixed effects of session and site insecurity. To examine our hypothesis that women in lower insecurity sites would improve more, we then ran a model that included an interaction between site insecurity level and session that allowed us to examine change over time as a function of site insecurity. Given the variability in PSA level of prior mental health experience and the potential for that to impact client outcomes, we included PSA’s number of years of experience as a fixed effect in all models. All analyses were conducted using Stata version 13 (StataCorp, 2013).
2. Results
A total of 1,646 level 1 observations were included in analyses from 158 participants living in the 7 sites randomized to receive CPT. Treatment completion was defined a priori as completion of 9 or more sessions (Bass et al., 2013). Based on that criteria, 141 participants (90%) were considered treatment completers. Participants completed the session monitoring questionnaire at an average of 10.4 (SD = 2.5) sessions,1 74 (46.8%) completed monitoring questionnaires at all 12 sessions, and 138 (87.3%) had completed monitoring questionnaires from at least 9 sessions. As shown in Tables 2, 3 sites (43%) were considered to have a high level of insecurity. Participants attended more sessions at these sites (M = 11.4, SD = 1.3) than at sites with low levels of insecurity (M = 9.7, SD = 3.0), t(156) = −4.43, p <.001.
Table 2.
Degree of insecurity by site.
| Site | PSA years experience | Level of insecurity | Exemplar security incidents during CPT |
|---|---|---|---|
| 1 | 9 | High | Over 40 people kidnapped and taken into the forest. One woman from group murdered. |
| 2 | 9 | High | One attack on site. People fled to the forest for safety. |
| 3 | 2 | High | Bullets fired in the centre of town by military. |
| 4 | 2 | Low | 6 murders by bandits or military over 2 months in the area. |
| 5 | 1 | Low | 2 outbursts of fighting causing displacement. |
| 6 | 6 | Low | Bandits attacked and robbed health centre. |
| 7 | 3 | Low | Attack and pillage of the parish and clinic. |
Table 3.
Results of the multilevel mixed effects model examining the impact of site insecurity on mental health symptom change across the 12 sessions of CPT.
| Fixed effects | Coefficient (95% CI) |
|---|---|
| Psychosocial counsellor experience | 3.13 (−0.75, 7.02) |
| Session | −1.93 (−2.02, −1.82) |
| Site insecurity | 1.90 (−1.99, 5.78) |
| Session x insecurity |
−0.25 (−0.40, −0.11) |
| Random effects |
Variance (95% CI) |
| Site | 5.48 (1.89, 15.90) |
| Treatment group | 0.04 (0.00, 2.88) |
| Participant | 0.56 (0.08, 0.19) |
SE = standard error; CI = confidence interval.
The average mental health symptom score at the first session of CPT was 20.8 (SD = 5.5), whereas at the last CPT session, the average symptom score was 1.6 (SD = 1.8). There was a non-significant trend for mental health symptoms to be greater at the first CPT session at sites with high (M = 21.7, SD = 4.5) compared to low (M = 20.1, SD = 6.0) levels of insecurity, t(156) = −1.83, p =.07. Symptom scores were significantly greater at the final CPT session at sites with high levels of insecurity (M = 2.5, SD = 2.0) compared to sites with low levels of insecurity (M = 0.8, SD = 1.1), t(131) = −6.02, p <.001.
In the first model, we examined only the main effects of session and site insecurity after accounting for the PSA’s level of experience. This model was significant (Wald χ2(3) = 2737.16; p <.001) and estimated a significant reduction in mental health symptoms over time (β = −2.04, 95% CI: −2.11, −1.96, p <.001). The effect of site insecurity was not statistically significant (β = 1.60, 95% CI: −2.30, 5.49, p =.42).
Next, we examined the impact of site-level insecurity on mental health symptom change across the CPT sessions (Table 3). The overall model was significant, Wald χ2(4) = 2937.98; p <.001. After accounting for the PSA’s level of experience, there was a significant interaction between site insecurity and session, such that sites with a high level of insecurity had a steeper slope (i.e. had a faster rate of mental health symptom reduction) compared to sites with a low level of insecurity. Visual examination of session-by-session change in high versus low insecurity sites (Figure 1) indicates that high-insecurity sites experienced an initial increase in symptom severity. The variation associated with site-, therapy group-, and participant-level clusters were significant.
Figure 1.
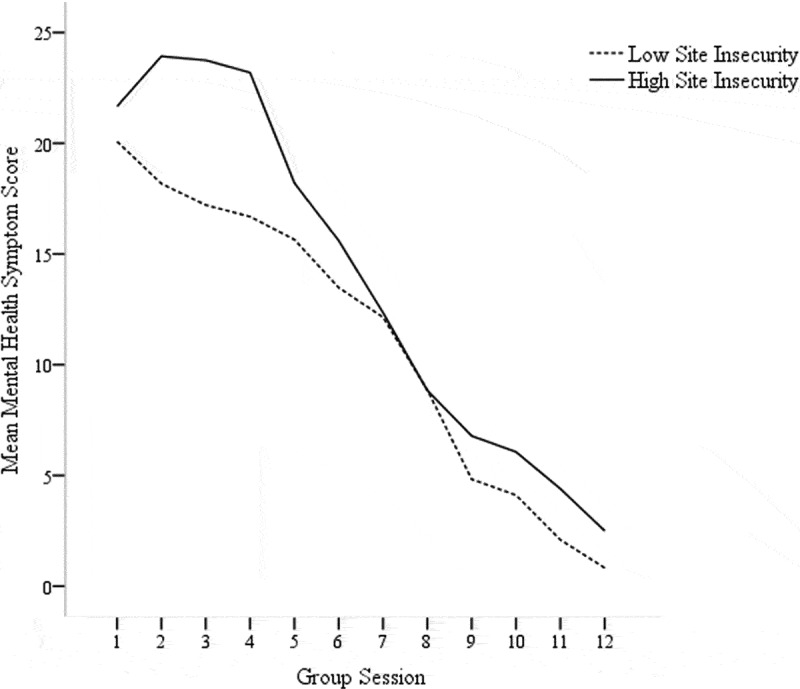
Impact of site insecurity on treatment outcomes over time.
3. Discussion
The purpose of the present study was to assess the extent to which degree of ongoing insecurity was associated with differences in the effectiveness of a psychotherapy intervention provided to female survivors of sexual violence. Our findings suggest that CPT can be delivered in high-insecurity settings without reductions in efficacy. Specifically, we found that, even in settings where there were armed groups in the area and ongoing violence while CPT treatment groups were being conducted, women improved and, contrary to our hypothesis, had comparable outcomes with women in lower insecurity sites. This is consistent with a growing body of literature suggesting that symptom improvement can occur when treating trauma in the context of ongoing conflict (Bass et al., 2013; Gillespie et al., 2002; Murray et al., 2013; Robjant, Roberts, & Katona, 2017; Tol et al., 2013), but expands this work to suggest that the degree of safety risk posed by a setting does not appear to affect outcomes. Notably, in higher-insecurity settings, treatment was provided effectively despite logistical challenges (e.g. not being able to use roads to travel to appointments during times of risk) and an ongoing risk of trauma to both clients and therapists. Indeed, high rates of treatment completion were observed across sites (i.e. 90% completed at least 9 sessions) relative to other trials of cognitive therapy in conflict settings (e.g. 79% completed at least 6 sessions in Duffy et al. (2007)), and participants in high-insecurity sites attended significantly more sessions. This provides important evidence in contradiction of concerns about the feasibility and efficacy of delivered trauma-focused interventions in settings where there are ongoing safety threats (Tol et al., 2013).
Contrary to our expectations, settings with higher levels of insecurity evidenced more rapid improvements in symptoms over the course of treatment. Although the mechanism of this effect is unclear, it is possible that clients in these settings were more motivated to engage in treatment or PSAs were more motivated to provide care in order to cope with ongoing threats to their safety. The PSAs in these sites also demonstrated a great deal of commitment to ensure high rates of participation in the groups, despite the level of insecurity. Specifically, these PSAs sometimes organized CPT group meetings in the forest or the fields when their communities were displaced to provide social support and to ensure group members could continue with therapy. This made sessions more accessible and may have increased group cohesion, potentially accounting for the higher rates of attendance at high-insecurity sites. The initial increase in scores experienced by women in high-insecurity areas also may account for the steeper slope, as there was more room within which to improve scores. This initial increase might also reflect exposure to emotions that were being avoided on a day to day basis as therapists encouraged non-avoidance. Our findings are also consistent with the larger PTSD treatment literature that suggests that increases in symptoms during early treatment are not ultimately harmful, as individuals still improve over time and reach good clinical outcomes by the end of treatment even if their symptoms initially increase (Nishith, Resick, & Griffin, 2002).
It is possible that beliefs generated via cognitive restructuring – a key skill in CPT – might be somewhat different in high-insecurity settings. A basic premise of CPT is that experiencing a trauma leads individuals to develop overaccommodated beliefs about themselves, others, and the world (e.g. ‘the world is completely dangerous’), which lead to distress and behavioural dysfunction. An underlying principle of CPT is that altering these beliefs to be more realistic will result in symptom reduction (Resnick & Schnicke, 1992). Although we did not collect systematic data regarding the nature of restructured cognitions in clients, what constitutes a realistic belief regarding safety (e.g. ‘this area is sometimes targeted by militants’) might differ for clients residing in an insecure setting compared to those living in relatively safer areas. If these realistic beliefs were, indeed, different across settings, the current study findings suggest that increasing realistic beliefs might be beneficial even when realistic beliefs reflect a relative lack of safety and may appear at first glance to be anxiety provoking. Future research could examine the targets and outcomes of cognitive restructuring in high-insecurity settings to better understand these processes.
To be maximally effective, efforts to disseminate and implement evidence-based practices must consider challenges raised by the context in which interventions will be implemented. However, dissemination and implementation theory have focused primarily on providers and organizations in terms of their readiness to implement new interventions. The current work poses an underexamined question relevant to dissemination and implementation theory and practice: will it be effective to implement a given intervention in a given context? Although our results suggest that CPT was effective even in high insecurity sites in eastern DRC, more work is needed in this area. Future research should continue to test how characteristics of settings alter the feasibility and effectiveness of evidence-based treatments and what the contextual limits are for when an intervention is no longer effective. Other characteristics of regions at high need for mental health treatment, such as poverty, remain largely untested as moderators of treatment impact and are additionally important targets for broader multisectoral interventions in addition to trauma-focused treatments (Purgato, Tol, & Bass, 2017). It would also be useful to explore whether instability in the lives of clients themselves – for example, continued risk of potential violence among clients in ongoing abusive relationships – affects the impact of trauma-focused therapies. This also presumes that basic client safety has been established prior to delivery of a trauma-focused therapy. Results from such studies could provide critical guidance to clinicians and policymakers.
The current study has several strengths, including the use of longitudinal assessment of women’s symptoms over many time points, the examination of differences across multiple contexts, and the examination of a high-need but under-resourced population. However, the study also has limitations. Because the primary purpose of the trial was to test the overall effectiveness of the intervention in eastern DRC, tests of differences in insecurity reflect a relatively small number of sites (only those randomized to CPT) that were not intentionally selected for their level of security. It is thus unclear whether the results are idiosyncratic to the sites selected and generalizable to other settings. In addition, the degree to which setting-level insecurity affected individual clients or the extent to which individual’s directly experienced trauma exposures during therapy (e.g. via re-traumatization in the course of treatment) was not measured. In addition, our measure of setting-level insecurity did not take into account individual participant experiences of insecurity and was based on a subjective measure of supervisors’ perceptions of incidents of insecurity rather than a systematic gathering of incident reports. Finally, the mental health symptom scale that was used as the primary outcome was itself not a validated scale, but was derived from longer measures that were locally validated (Bass et al., 2013). Also, due to logistical challenges, only total score data were collected, rather than item-level data. This precluded us from examining how individual symptoms changed over time and precluded us from examining the psychometrics of the reduced measure, though psychometrics of the larger 55-item measure were examined. These limitations should be addressed in future research.
In sum, this work provides important evidence to support the feasibility and effectiveness of efforts to reduce global mental health disparities by implementing evidence-based treatments, even in settings with major barriers to implementation. Similar examinations of the degree to which perceived barriers to implementation in high-need settings affect treatment feasibility and effectiveness will be critical in informing global dissemination and implementation efforts.
Funding Statement
This work was supported by the U.S. Agency for International Development Victims of Torture Fund and the World Bank. Manuscript preparation for this article was supported by National Institute of Alcohol Abuse and Alcoholism (NIAAA) Grants K99AA026317(PI: Dworkin), R00AA026317 (PI: Dworkin), and K08AA021745 (PI: Stappenbeck). These agencies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Notes
Session monitoring questionnaires were sometimes not completed when participants arrived late or clinicians did not record or transmit session data.
Acknowledgments
We very much appreciate the contributions of our colleagues Laura Murray and Amani Matabaro for their time and effort on this project and Doug Zatzick for his comments and questions that inspired this paper. We greatly appreciate the time and effort of our participants, counsellors, and supervisors devoted to this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Applied Mental Health Research Group . (2013a, December 1). Design, implementation monitoring, and evaluation of mental health and psychosocial assistance programs for trauma survivors in low resource countries: A user’s manual for researchers and program implementers (Adult version). Module 1: Qualitative assessment. Retrieved from https://www.jhsph.edu/research/%0D%0Acenters-and-institutes/global-mental-health/resource-materials/%0Ddesign-implementation-monitoring-and-evaluation-dime/%0D%0A
- Applied Mental Health Research Group . (2013b, December 1). Design, implementation monitoring, and evaluation of mental health and psychosocial assistance programs for trauma survivors in low resource countries: A user’s manual for researchers and program implementers (Adult version). Module 2: Developing quantitative measures. Retrieved from https://www.jhsph.edu/research/centers-and-institutes/global-mentalhealth/%0D%0Aresource-materials/design-implementation-monitoring-and-evaluation-dime/%0D%0A
- Asgary, R., Emery, E., & Wong, M. (2013). Systematic review of prevention and management strategies for the consequences of gender-based violence in refugee settings. International Health, 5(2), 85–10. [DOI] [PubMed] [Google Scholar]
- Bass, J. K., Annan, J., McIvor Murray, S., Kaysen, D., Griffiths, S., Cetinoglu, T., … Bolton, P. A. (2013). Controlled trial of psychotherapy for Congolese survivors of sexual violence. The New England Journal of Medicine, 368, 2182–2191. [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Schafer, A., Dawson, K. S., Anjuri, D., Mulili, C., Ndogoni, L., … Hadzi-Pavlovic, D. (2017). Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: A randomised clinical trial. PLoS Medicine, 14, 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coghan, B., Ngoy, P., Muluma, F., Hardy, C., Bemo, V. N., Stewart, T., … Brennan, R. (2007). Mortality in the Democratic Republic of Congo: An ongoing crisis. New York, NY: International Rescue Committee. [Google Scholar]
- Cohen, J. A., Mannarino, A. P., & Iyengar, S. (2011). Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence. Archives of Pediatrics & Adolescent Medicine, 165, 16–21. [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., & Covi, L. (1974). The Hopkins Symptom Checklist (HSCL): A self‐report symptom inventory. Behavioral Science, 19, 1–15. [DOI] [PubMed] [Google Scholar]
- Duffy, M., Gillespie, K., & Clark, D. M. (2007). Post-traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: Randomised controlled trial. BMJ, 334(7604), 1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duroch, F., McRae, M., & Grais, R. F. (2011). Description and consequences of sexual violence in Ituri province, Democratic Republic of Congo. BMC International Health and Human Rights, 11(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin, E. R. (2018). Risk for mental disorders associated with sexual assault: A meta-analysis. Trauma, Violence, & Abuse. Advance online publication. doi: 10.1177/1524838018813198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin, E. R., Menon, S. V., Bystrynski, J., & Allen, N. E. (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagle, G., & Kaminer, D. (2013). Continuous traumatic stress: Expanding the lexicon of traumatic stress. Peace and Conflict, 19, 85–99. [Google Scholar]
- Gillespie, K., Duffy, M., Hackmann, A., & Clark, D. M. (2002). Community based cognitive therapy in the treatment of post-traumatic stress disorder following the Omagh bomb. Behaviour Research and Therapy, 40, 345–357. [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E., Watson, P., Bell, C. C., Bryant, R. A., Brymer, M. J., Friedman, M. J., … Maguen, S. (2007). Five essential elements of immediate and mid–term mass trauma intervention: Empirical evidence. Psychiatry: Interpersonal and Biological Processes, 70, 283–315. [DOI] [PubMed] [Google Scholar]
- Iverson, K. M., Resick, P. A., Suvak, M. K., & Taft, C. T. (2012). Engagement and outcome in Cognitive Processing Therapy. Initiate Partner Violence Exposure Predicts PTSD Treatment Engagement and Outcome in Cognitive Processing Therapy, 42, 236–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, K., Asher, J., Rosborough, S., Raja, A., Panjabi, R., Beadling, C., & Lawry, L. (2008). Association of combatant status and sexual violence with health and mental health outcomes in postconflict Liberia. JAMA, 300, 676–690. [DOI] [PubMed] [Google Scholar]
- Johnson, K., Scott, J., Kisielewski, M., Asher, J., Ong, R., & Lawry, L. (2010). Association of sexual violence and human health in territories of the eastern Democratic Republic of the Congo. JAMA, 304, 553–562. [DOI] [PubMed] [Google Scholar]
- McLay, R. N., McBrien, C., Wiederhold, M. D., & Wiederhold, B. K. (2010). Exposure therapy with and without Virtual reality to treat PTSD while in the combat theater: A parallel case series. Cyberpsychology, Behavior, and Social Networking, 13, 37–42. [DOI] [PubMed] [Google Scholar]
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. Journal of Nervous and Mental Disease., 180, 111–116. [PubMed] [Google Scholar]
- Murray, L. K., Cohen, J. A., & Mannarino, A. P. (2013). Trauma-focused cognitive behavioral therapy for youth who experience continuous traumatic exposure. Peace and Conflict, 19, 180–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, L. K., Jordans, M., Amin, A. M., Bolton, P., Cisalva, I., Valle, U., & Thornicroft, G. (2014). Dissemination and implementation of evidence based, mental health interventions in post conflict, low resource settings. Intervention, 12, 94–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishith, P., Resick, P. A., & Griffin, M. G. (2002). Pattern of change in prolonged exposure and cognitive-processing therapy for female rape victims with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 70, 880–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttman-Shwartz, O., & Shoval-Zuckerman, Y. (2016). Continuous traumatic situations in the face of ongoing political violence: The relationship between CTS and PTSD. Trauma, Violence, and Abuse, 17, 562–570. [DOI] [PubMed] [Google Scholar]
- O’Callaghan, P., McMullen, J., Shannon, C., Rafferty, H., & Black, A. (2013). A randomized controlled trial of trauma-focused cognitive behavioral therapy for sexually exploited, war-affected congolese girls. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 359–369. [DOI] [PubMed] [Google Scholar]
- Purgato, M., Tol, W. A., & Bass, J. K. (2017). An ecological model for refugee mental health: Implications for research. Epidemiology and Psychiatric Sciences, 26(2), 139–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications Inc. [Google Scholar]
- Resick, P. A., Galovski, T. E., Uhlmansiek, M. O. B., Scher, C. D., Clum, G. A., & Young-Xu, Y. (2008). A randomized clinical trial to dismantle components of Cognitive Processing Therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76, 243–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick, P. A., & Schnicke, M. K. (1992). Cognitive Processing Therapy for sexual assault victims. Journal of Consulting & Clinical Psychology, 60, 748. [DOI] [PubMed] [Google Scholar]
- Robjant, K., Roberts, J., & Katona, C. (2017). Treating posttraumatic stress disorder in female victims of trafficking using narrative exposure therapy: A retrospective audit. Frontiers in Psychiatry, 8, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press. [Google Scholar]
- StataCorp . (2013). Stata statistical software: Release 13. College Station, TX: Author. [Google Scholar]
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302, 537–549. [DOI] [PubMed] [Google Scholar]
- Stein, B. D., Jaycox, L. H., Kataoka, S. H., Wong, M., Tu, W., Elliott, M. N., & Fink, A. (2003). A mental health intervention for schoolchildren exposed to violence. JAMA, 290, 603–611. [DOI] [PubMed] [Google Scholar]
- Steiner, B., Benner, M. T., Sondorp, E., Schmitz, K. P., Mesmer, U., & Rosenberger, S. (2009). Sexual violence in the protracted conflict of DRC programming for rape survivors in South Kivu. Conflict and Health, 3(1), 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tol, W. A., Barbui, C., & van Ommeren, M. (2013). Management of acute stress, PTSD, and bereavement: WHO recommendations. JAMA, 310(5), 477–478. [DOI] [PubMed] [Google Scholar]
- Tol, W. A., Stavrou, V., Greene, M. C., Mergenthaler, C., van Ommeren, M., & Moreno, C. G. (2013). Sexual and gender-based violence in areas of armed conflict: A systematic review of mental health and psychosocial support interventions. Conflict and Health, 7(1), 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNHCR . (2019, December 1). DR Congo emergency. Retrieved fromhttps://www.unhcr.org/dr-congo-emergency.html
- Vickerman, K. A., & Margolin, G. (2009). Rape treatment outcome research: Empirical findings and state of the literature. Clinical Psychology Review, 29, 431–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wangelin, B. C., & Tuerk, P. W. (2014). PTSD in active combat soldiers: To treat or not to treat. Journal of Law, Medicine & Ethics, 143, 161–170. [DOI] [PubMed] [Google Scholar]
- Weiss, W. M., Murray, L. K., Zangana, G. A. S., Mahmooth, Z., Kaysen, D., Dorsey, S., … Bolton, P. (2015). Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: A randomized control trial. BMC Psychiatry, 15, 249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2013). Guidelines for the management of conditions specifically related to stress. Geneva, Switzerland: WHO. [PubMed] [Google Scholar]
- World Health Organization . (2010). Mental Health Gap Action Programme: MhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings: Version 1.0(pp. 86–94). Geneva: WHO. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- UNHCR . (2019, December 1). DR Congo emergency. Retrieved fromhttps://www.unhcr.org/dr-congo-emergency.html


