Dear Editor
Since the outbreak of Coronavirus Disease 2019 (COVID-19) in December 2019 in Wuhan, China, an increasing body of literature has discussed the radiologic manifestations, with case reports and case series describing the important radiologic features (1). Most radiologic investigations have focused on chest CT scan because of its wide availability and high resolution. It provides a thorough insight into lung parenchymal involvement, thus leading to early diagnosis and prompt patient management. CT findings can also be used to assess the disease severity and to suggest the possibility of superimposed bacterial infection (2). Although the imaging manifestations of the new corona virus pneumonia are similar to common viral pneumonia, some more specific imaging characteristics have also been described. One of the most common radiologic presentations is patchy or punctate ground glass opacity (GGO). Patchy consolidation may also be detectable, but with less frequency (3,4). Therefore, by detecting peripheral subpleural GGO in suspected cases and in appropriate clinical setting, radiologists can often make a confident diagnosis.
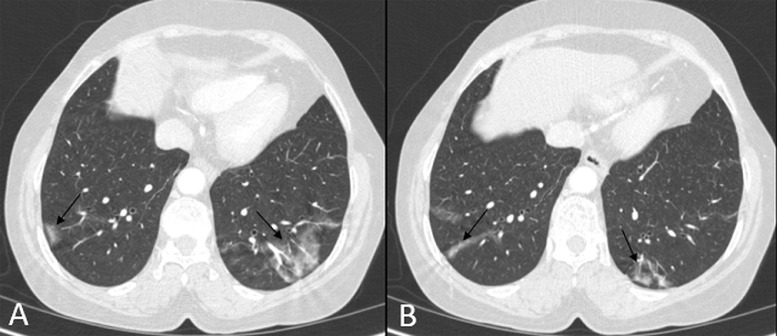
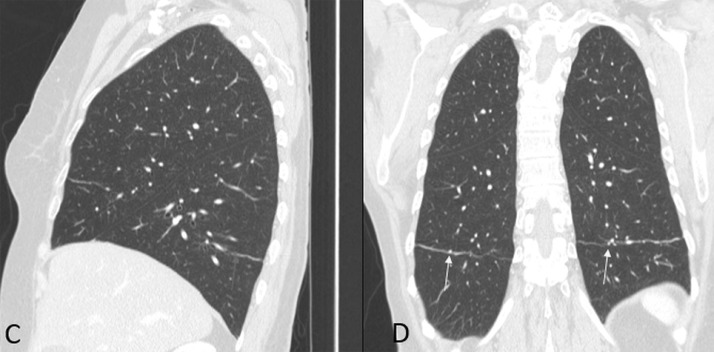
However, awareness of other diseases resulting in such a radiologic pattern is essential when interpreting the CT images. Moreover, there may be some technical issues, resulting in an artifactual ground glass pattern. Figure 1 demonstrates axial chest CT images in a suspected case of COVID-19 infection referred to our center. Irregular zones of ground glass densities are visible in both lower lobes (Fig 1). Based on this finding, the chest CT scan was initially considered consistent with the COVID-19 pneumonia; however, the sagittal and coronal reconstructed images, revealed that the apparent GGOs were in fact caused by linear atelectasis in the bases of both lower lobes in an otherwise normal lung (Fig 2 ). On all images, structures that are partially included within the imaging volume may cause partial volume averaging. The commonest example of this occurs with linear areas of atelectasis and scarring. A thickened interlobar fissure may also result in a similar appearance. When these linear or band-like structures course through the same plane as a CT slice, a ground glass opacity may artifactually form (5). The cause can usually be recognized by looking at the coronal or sagittal reformats. In most cases, the diagnosis is still evident, as the COVID infection tends to be multifocal, involving multiple segments and lobes, however, more focal lung involvement has also been reported (3). Therefore, one should be aware of the possibility of this artifact when reporting the axial CT images with limited involvement, especially those cases with focal basal GGO, where linear atelectasis is also common. In such cases correlation with reformatted planes and utilizing thin section reconstructions are recommended to avoid misinterpretation.
Figure 1.
(a, b) Axial CT images of chest demonstrate bilateral basal GGO (black arrow).
Figure 2.
(c, d) Sagittal and coronal reconstructed images reveal linear atelectasis (blue and yellow arrows). These artifactually mimic GGO in axial sections. (Color version of figure is available online.)
Footnotes
Author Contribution: SP. O. has provided the case and images and P.I. and S.H. have written the article.
Funding: SP.O., S.H. and P.I. report no funding sources.
Consent: Images are completely anonymised, however informed consent has also been obtained from the patient.
References
- 1.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim H. Outbreak of novel coronavirus (COVID-19): What is the role of radiologists? Eur Radiol. 2020 doi: 10.1007/s00330-020-06748-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;13:1–4. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan Y., (1), Guan H., (2) Imaging changes in patients with 2019-nCov. Eur Radiol. 2020:1–2. doi: 10.1007/s00330-020-06713-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lynch D.A., Newell J.D., Lee J.S. Imaging of diffuse lung disease. PMPH-USA. 2000;1:8. [Google Scholar]