Figure 25. Role of SRC kinase in restoring structure and restrictive murine BNB permeability in GDNF transgenic mice following sciatic nerve crush injury.
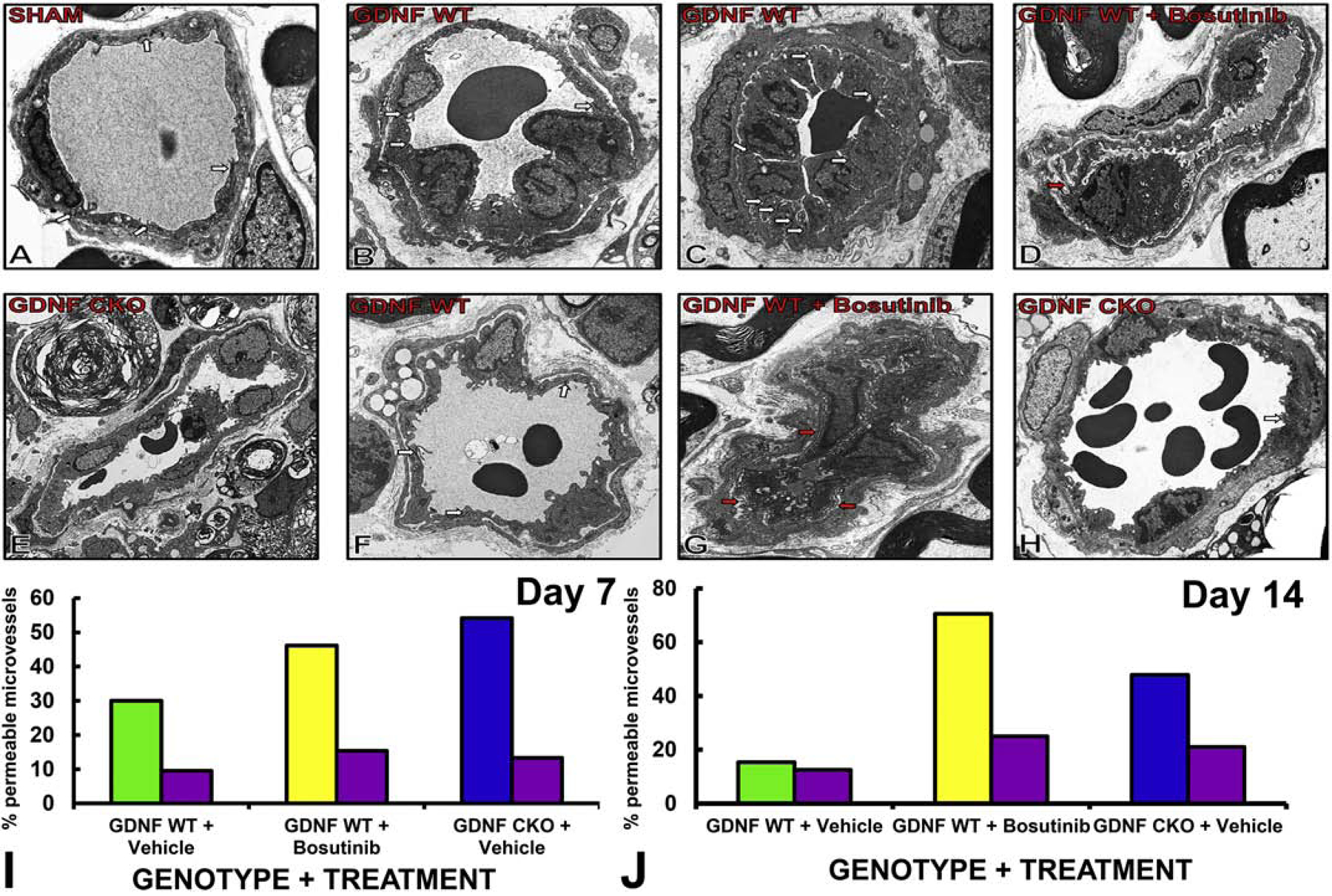
Axial digital ultramicrographs show electron-dense inter-cellular tight junctions (white arrows) in normal, horseradish peroxidase-impermeable endoneurial microvessels in Sham surgery control nerves (A). On Day 7 after crush injury, tight junctions are commonly seen in GDNF WT mice (B), even in microvessels with endothelial cell proliferation (C). Structurally disorganized permeable microvessels are commonly seen in GDNF WT mice treated with SRC kinase inhibitor, Bosutinib, with basement membrane duplication (red arrow, D). Structurally organized permeable microvessels that lack tight junctions are commonly seen in GDNF CKO mice (E). On Day 14, more intact endoneurial microvessels with tight junctions (white arrows) are seen in GDNF WT mice (F). Permeable microvessels with disorganized endothelial cells and basement membrane duplication (red arrows) are commonly seen in GDNF WT mice treated with Bosutinib (G). More permeable microvessels are seen in GDNF CKO mice, with less frequent tight junctions (white arrow, H) compared to GDNF WT mice. Original magnification 4500–7000X. Bar histograms show sciatic nerve BNB permeability to horseradish peroxidase, quantified as the % of permeable microvessels in each nerve by electron microscopy, with data compared with the uninjured contralateral Sham surgery nerve (purple) and the different experimental groups on Day 7 (I) and Day 14 (J). SRC kinase inhibitor, Bosutinib abrogated the expected GDNF-driven restoration of BNB impermeability following nerve injury on days 7 and 14, with the expected delayed in GDNF CKO mice also observed as previously published. N=1 (quantified in duplicate with a mean of 17 microvessels/ mouse evaluated).
