Abstract
Supported by evidence‐based guidelines, custom‐made footwear is often prescribed to people with diabetes who are at risk for ulceration. However, these guidelines do not specify the footwear design features, despite available scientific evidence for these features. We aimed to develop a design protocol to support custom‐made footwear prescription for people with diabetes and peripheral neuropathy. The population of interest was people with diabetes who are at moderate‐to‐high risk of developing a foot ulcer, for whom custom‐made footwear (shoes and/or insoles) can be prescribed. A group of experts from rehabilitation medicine, orthopaedic shoe technology (pedorthics) and diabetic foot research, reviewed the scientific literature and met during 12 face‐to‐face meetings to develop a footwear design algorithm and evidence‐based pressure‐relief algorithm as parts of the protocol. Consensus was reached where evidence was not available. Fourteen domains of foot pathology in combination with loss of protective sensation were specified for the footwear design algorithm and for each domain shoe‐specific and insole (orthosis)‐specific features were defined. Most insole‐related features and some shoe‐related features were evidence based, whereas most shoe‐related features were consensus based. The pressure‐relief algorithm was evidence based using recent footwear trial data and specifically targeted patients with a healed plantar foot ulcer. These footwear design and pressure‐relief algorithms are the first of their kind and should facilitate more uniform decision making in the prescription and manufacturing of adequate shoes for moderate‐to‐high‐risk patients, reducing variation in footwear provision and improving clinical outcome in the prevention of diabetic foot ulcers.
Keywords: custom‐made shoes, design protocol, diabetic foot, footwear, peripheral neuropathy, plantar pressure
1. INTRODUCTION
Custom‐made footwear is in many settings prescribed to people with diabetes who are at moderate to high risk for ulceration, with the goal to accommodate foot deformities present, relieve peak plantar pressures, provide stability in walking and protect the foot against minor trauma. International guidelines recommend the use of custom‐made footwear to help prevent diabetic foot ulceration, with target pressures for footwear provided for those patients who healed from a plantar foot ulcer.1, 2, 3, 4, 5
While the goals for custom‐made footwear are clear and clinical decision‐making in selecting the type of footwear is often defined by the degree of foot deformity present, footwear design can be variable and is hardly supported by any published protocol, shoe concept or algorithm. Only two consensus‐based algorithms for custom‐made footwear and a pressure‐ and foot shape‐guided design algorithm for custom‐made insoles have been identified in the scientific literature.6, 7, 8 And while the international guidelines stress the need for adequate footwear, specifications for footwear design are not provided.9 Thus, a comprehensive conceptual approach to prevention of foot disease through the use of footwear is still largely lacking, which may affect efficacy in prevention.
This is unfortunate, because the biomechanical effects of shoe and insole designs and their features have been widely investigated and show to be consistent.10, 11, 12, 13, 14 Furthermore, the clinical efficacy of some of these biomechanical footwear designs in reducing risk of ulcer recurrence has been proven.15, 16, 17 Apparently, it has been difficult to translate this knowledge into clinical footwear practice, which stresses the need for a design protocol for custom‐made footwear, so to facilitate its prescription and manufacturing beyond guidelines. Such a protocol should be evidence based; where evidence is not available, consensus‐based design rules should be used.
We aimed to develop and present a design protocol for custom‐made footwear for the moderate‐to‐high‐risk patient with diabetes and peripheral neuropathy.
2. MATERIALS AND METHODS
The population of interest was people with diabetes who were at moderate to high risk of developing a foot ulcer by having at least loss of protective sensation due to peripheral neuropathy,18 and, typically, have a foot ulcer history or a foot deformity (including limited joint mobility).
The protocol consists of two parts: (1) an evidence‐ and consensus‐based design algorithm for the moderate‐to‐high risk patient and (2) an evidence‐based pressure‐relief algorithm for the high‐risk patient with plantar foot ulcer history.
The scientific literature on the biomechanical effects of footwear designs in people with diabetes was reviewed and assessed (by J.Z. and S.B.) in order to determine the evidence base for the algorithms.
2.1. Footwear design algorithm
A group of experts in the field came together on 12 occasions for 2‐hour meetings to develop the algorithm. These experts included two rehabilitation medicine physicians (R.D. and T.B.) and four senior orthopaedic shoe technicians (ie, pedorthists), all with long‐time experience in provision of custom‐made footwear for diabetic patients, and two diabetic foot researchers (S.B. and J.Z.).
The experts defined the domains of foot pathology for the footwear design algorithm; the goal here was to cover at least 80% of the feet seen in clinical footwear practice. The experts also defined the technical footwear aspects, that is, the different shoe and insole design features, which had to be included in the algorithm. Definitions for mechanisms of action of the shoe/insole, footwear construction features and materials used were carefully considered and established in order to get uniform understanding within the group of experts.
The outcomes of the literature review were discussed within the expert group and the evidence found for the different shoe and design features was included in the algorithm. The evidence found could be direct, meaning that the effect was found in persons with diabetes, or indirect, meaning the effect was found in non‐diabetic subjects. For shoe and insole design features for which no evidence was available, consensus within the group was required and obtained. Previous consensus‐based algorithms were also consulted.6, 7
A draft algorithm was assessed by each expert and discussed within the group at one of the meetings. Comments made were incorporated in a new draft. After several iterations of this process, a final version of the algorithm was written.
2.2. Pressure‐relief design algorithm
We used the outcomes from the systematic review and data from our previous footwear trial,10, 15 to develop an evidence‐based design algorithm for improved and sustained pressure relief in custom‐made footwear for high‐risk diabetic patients with plantar foot ulcer history.
3. RESULTS
3.1. Footwear design algorithm
A total of 14 domains of foot pathology were defined (Table 1). All include the presence of loss of protective sensation and per domain a specific deformity (including limited joint mobility). Specifications for the shoe and insole features for each domain are given in the text. With a patient fitting in more than one domain or with specific conditions present, contraindications may exist for one or more design features, as explained below or as judged by the prescribing physician or shoe technician.
Table 1.
The footwear design algorithm for 14 domains of foot pathology with loss of protective sensation
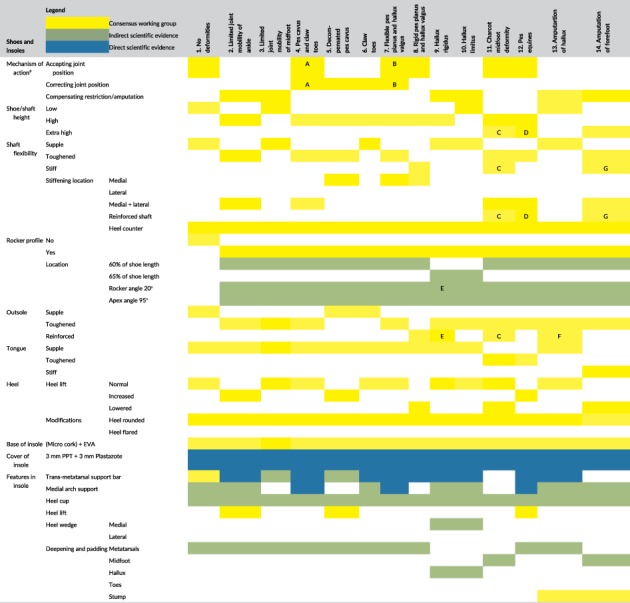
The mechanism of action of the shoe can be corrective, accepting and compensating. Corrective means that the footwear corrects deviating joint positions of the foot. Accepting means that these deviating joint positions are accepted by the footwear. Compensating means that a movement restriction or an amputation is compensated for; the shoe then takes on the function of the affected part of the foot.
Note: Explanatory letter symbols:
A. For a rigid pes cavus with rigid claw toes, the mechanism of action is accepting, for non‐rigid claw toes it is correcting.
B. For flexible pes planus, the mechanism of action is correcting, for hallux valgus it is accepting
C. The first provision is with an externally reinforced stiff extra‐high shaft and outsole reinforcement. After >3 months, switch to a toughened high shaft with medial/lateral reinforcement between lining and outer of the shoe and a toughened outsole
D. Generally, apply a high toughened shaft with mediolateral reinforcement. Consider an extra‐high reinforced shaft with extreme equines and some ankle range of motion possible.
E. With hallux rigidus and desire to restrict movement in the first metatarsal‐phalangeal joint, use a large rocker angle (>20°) and outsole reinforcement.
F. Consider using a reinforced outsole when only the hallux is amputated, to prevent build‐up of pressure at the first metatarsal head. In case of first ray amputation, a toughened outsole can be used.
G. Consider using a reinforced stiff shaft with forefoot amputation and gait stability problems.
Several rules of thumb in footwear design apply to each of the 14 domains:
Each shoe must have sufficient interior space in length and width, with a minimum of 1 cm space in length between longest toe and inner of the shoe. The toe box must be sufficiently high to accommodate non‐correctable claw or hammer toes or a hyperextended hallux.
No seams should be present in the inner lining.
Shoes should have laces. If hand function is insufficient, Velcro straps are the best option.
The shoe should provide adequate shock absorption during loading of the foot.
With active use, attention should be paid to the durability (in the choice of materials) and the weight of the shoe.
With a clearly reduced proprioception, attention should be paid to a stable support during stance, if needed using a more distal rocker axis.
With presence of oedema or vulnerable skin in the lower leg, a low‐cut shoe is preferred. If a high‐cut shoe is indicated, the inner should be padded and top edge of the shoe should be above the vulnerable area. A 1.5‐mm‐thick flat layer of material below the insole creates the opportunity to moderate interior volume with changing oedema.
3.1.1. Shoe/shaft height
For shoe or shaft height, the following classification is used:
Low cut = below the malleolus.
High cut = at the level of malleolus.
Extra high cut = above the malleolus.
3.1.2. Shaft flexibility/reinforcement
A lateral rearfoot reinforcement should be used when a fixed varus deviation is present in the sub‐talar joint, and a medial rearfoot reinforcement when fixed valgus is present, to provide stability. Always apply the reinforcement in combination with a reinforcement on the contralateral shoe side. A 5° wedge may be applied in the rear part of the insole if varus or valgus in the sub‐talar joint is present and correctable.19
If the pathology is in combination with muscle weakness of the tibialis anterior or peroneus longus muscles (Medical Research Council ≤3), an extra high‐cut shaft reinforcement within the shoe should be chosen, to support dorsiflexion of the ankle. Another solution is to add an external orthosis, such as an ankle‐foot orthosis.
3.1.3. Rocker profile
The rocker profile of the shoe significantly reduces peak pressure under the forefoot.20, 21, 22, 23, 24, 25 For illustrations of rocker apex, axis and angle and longitudinal axes see References.21, 25
With fully custom‐made shoes, the rocker is applied in the insole, with the outsole following this insole rocker configuration one‐on‐one. With prefabricated shoes, the rocker is in the outsole.
The rocker apex is the central point on the rocker axis and should be at 60% of shoe length, measured from the rear of the shoe, to provide optimal balance for pressure relief under the different metatarsal heads.20, 21, 22 This relates to a rocker axis that is ~1.3 cm proximal to metatarsal head 1 and ~2.6 cm proximal to metatarsal head 2 for shoe size US9.5.22
The rocker apex should be at 65% of the shoe length, measured from the rear of the shoe, to provide optimal balance for pressure relief under the toes.22, 23, 24 This relates to a rocker axis that is ~0.2 cm distal to metatarsal head 1 and ~1.2 cm proximal to metatarsal head 2 for shoe size US9.5.22
The rocker angle is the angle between the ground and the bottom surface of the shoe from the rocker apex forward and should be 20° in each shoe, independent of shoe size.21
The apex angle is the angle between the rocker axis and the longitudinal axis of the shoe and should be 95°.21 This means that the rocker axis is medially more distal than laterally. The rocker apex should still be at 60%/65% of the shoe length (see earlier). With an exorotation position of the foot, the rocker axis must be corrected to give an apex angle of 95° on the direction of walking.
3.1.4. Shoe outsole
The shoe outsole should provide cushioning and can be made supple or toughened, or can be reinforced with a carbon or metal layer over the partial or entire length of the shoe to create a stiff outsole that is not bendable. With clearly reduced proprioception, opt for a toughened and not a stiff outsole. Pay attention to sufficient traction of the outsole in these patients with peripheral neuropathy.
3.1.5. Tongue
The tongue of the shoe can be made supple, toughened, or stiff and is always padded. A stiff tongue is used mainly with forefoot amputation.
3.1.6. Heel of the shoe
The heel of the shoe can take several configurations. Normal heel height for men is 1.5‐2 cm and for women 2.5‐3 cm. An increased heel lift is provided in fully custom‐made shoes via heel lift in the shoe, in prefabricated shoes via heel lift in the insole (maximum 1 cm). Increased heel lift in pes equines is dependent on the available ankle range of motion. Lateral or medical heel flare can be given if there is varus or valgus tilting of the calcaneus, in order to normalize the centre of pressure.
3.1.7. Insole base
The base of the insole in a fully custom‐made shoe should be of 5‐mm‐thick micro cork (shore 55) with on top 5‐mm‐thick Ethylene Vinyl Acetate (EVA) (shore 35‐40). With prefabricated shoes the base should consist of 6‐mm‐thick EVA (shore 35‐40). The use of materials with proven similar properties in mainly compressibility and durability is also possible.26
3.1.8. Insole top layer
The top layer of the insole should be a combination of 3‐mm‐thick closed‐cell foam (eg, Plastazote type LD45) on top of 3‐mm‐thick open‐cell cushioning foam (eg, Professional Protective Technology (PPT)), over its entire length. The combination of Plastazote and PPT has shown to be effective in pressure relief,10 but the use of materials with similar properties is also possible. A leather top layer has proven ineffective in pressure relief and should not be used.10
3.1.9. Metatarsal support
A metatarsal support significantly improves peak pressure reduction at the metatarsal heads.10, 19, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38
Use a transmetatarsal bar that covers all metatarsal heads as support.30 A metatarsal pad or dome can be used if only one metatarsal region shows (signs of) high pressure, or is a previous ulcer site.
The material of the metatarsal support should be of EVA, cork, or a similar material (shore 55).31 The support is covered by the insole top layer.
The height of the support should be 9‐10 mm.29
The location of the support should be 6‐11 mm proximal to the metatarsal head, in static position.32, 37, 38 This means that with a support with an apex 10 mm from its distal edge, the distal edge is 6‐11 mm proximal to the center of the metatarsal head.31 Thus, the apex of the metatarsal support is 16‐21 mm from the center of the metatarsal head. Take into account that the insole top layer affects the effective location of the metatarsal support in the shoe, moving it more distally.
With a tightly tensioned plantar fascia, or nodules in the fascia (eg, in patients with morbus Ledderhose [or plantar fibromatosis]), support should be limited and these nodules should be adequately offloaded.
3.1.10. Medial arch support
A medial foot arch support also significantly reduces peak pressure in the forefoot.7, 10, 12, 19, 27, 39, 40 Add 3‐5 mm height to the existing foot arch support obtained from total contact through semi‐weight‐bearing fitting with plaster, foam box, or scan.10, 19 Pressure relief under the hallux can be improved by combining a medial arch support with a full length varus wedge.19
With a tightly tensioned plantar fascia, or nodules in the fascia (eg, in patients with morbus Ledderhose [plantar fibromatosis]), the medial foot arch support should be customized; an alternative would be a support at the sustentaculum tali.
3.1.11. Heel cup
A heel cup more effectively maintains the sub‐cutaneous fat tissue underneath the calcaneus and can distribute pressure to the midfoot and to the walls of the insole, thereby relieving pressure on the heel.19, 27
3.1.12. Local removal and padding
The removal of material (a local cut‐out) at the former ulcer location or a high‐pressure location and padding thereof with a different material reduces local peak pressure.10, 12 The cut‐out should be circular or slightly oval in shape in the walking direction and be minimally larger than the region of interest. The cut‐out should be 5 mm deep and padded with a 3‐mm durable material up to shore 30.
3.2. Pressure‐relief design algorithm
Table 2 shows the pressure‐relief design algorithm, consisting of 10 required steps for the design of custom‐made footwear that effectively reduces peak plantar pressure in the high‐risk patient with plantar foot ulcer history.
Table 2.
The evidence‐based pressure‐relief design algorithm for patients with plantar foot ulcer history
| Step 1 | Shoe | Rigid outsole that permits a maximum of 10° bending |
| Step 2 | Shoe | Rocker outsole with 20° angle and axis at 60% of shoe length |
| Step 3 | Insole | Base: Fully custom‐made shoes: 5‐mm‐thick micro corka + 5‐mm‐thick EVA; extra‐depth prefabricated shoes: 6‐mm‐thick EVA |
| Step 4 | Insole | Total contact insole with 3‐5‐mm‐thick medial arch support added |
| Step 5 | Insole | Transmetatarsal bar of 9‐10 mm height and located 6‐11 mm proximal of metatarsal head (see manuscript text for details) |
| Step 6 | Insole | 5‐mm‐depth removal and 3‐mm‐thick padding at high‐pressure regions |
| Step 7 | Insole | Insole top cover of 3‐mm‐thick closed‐cell foam (eg, Plastazote) on top of 3‐mm‐thick open‐cell cushioning foam (eg, PPT)b |
| Step 8 | Assessment | In‐shoe plantar pressure measurement |
| Step 9 | Modification | Footwear modification if midfoot/forefoot peak pressure >200 kPac |
| Step 10 | Assessment | Reassessment of in‐shoe plantar pressures at 6 months |
Note: With specific conditions, contraindications may exist for one or more design features in this algorithm, as explained in the results or judged by the prescribing physician or shoe technician.
Or multiform
Or materials with similar characteristics
A maximum two rounds of modifications of shoe and/or insole with subsequent pressure assessment are considered, to provide a reasonable cost‐benefit. Any further modification after two rounds should be considered with respect to pressure outcome achieved and time and effort invested.
4. DISCUSSION AND CONCLUSIONS
The footwear design algorithm covers the majority of foot types and deformities seen in diabetic foot care. As Table 1 shows, most of the features of the insole are evidence based for pressure relief, either directly from studies on diabetic subjects or indirectly from non‐diabetic subjects. Few aspects are not evidence based such as the insole base. Most of the shoe features are consensus based. Only regarding the rocker profile, sufficient evidence is available in the literature. Our algorithm is quite different from previous footwear design algorithms, which are mainly consensus based.6, 7 This demonstrates that footwear design and provision is moving from an experience and skills‐based approach to a more scientific data‐driven approach, while more research is needed to support mainly the design of the shoe for the diabetic patients at risk.
The pressure‐relief design algorithm is a 10‐step approach to provide improved and sustained pressure relief in custom‐made footwear for high‐risk diabetic patients with plantar foot ulcer history. The steps are evidence and scientific based and data driven. It uses in‐shoe plantar pressure measurements for the evaluation of the footwear and, if needed, to guide modification of the insole or shoe to further improve pressure relief to a target level that is recommended in international guidelines and based on previous research from the authors and others.12, 15, 41, 42 This algorithm leads to substantially lower in‐shoe peak plantar pressures in high‐risk patients and fewer modifications needed to reach the target pressure when compared to other design methods.43
In conclusion, the footwear design and pressure‐relief algorithms are the first of their kind and state of the art and should facilitate more uniform decision making in the prescription and manufacturing of adequate shoes for high‐risk patients. This should reduce variation in footwear provision andimprove clinical outcome in the prevention of diabetic foot ulcers.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
GLOSSARY
- footwear
the shoe and the removable insole
- insole
synonym for insert or in‐shoe orthosis
- custom‐made footwear
fully custom‐made shoes and insoles or custom‐made insoles worn in diabetes‐specific prefabricated (extra‐depth) shoes.
AUTHOR CONTRIBUTIONS
All authors were involved in developing the footwear design algorithm. S.A.B. developed the pressure‐relief algorithm. S.A.B. wrote the manuscript. J.B.Z., T.B.W. and R.D. critically reviewed the manuscript for content and suggested modifications. All authors have read and approved the final manuscript.
ACKNOWLEDGEMENTS
The authors acknowledge the valuable contributions of orthopedic shoe technicians Arun Ahmadi, Ronald Lever, Corstiaan Noels, Jan Pulles and Carlijn Renee, and manager Esther Mik, all from Livit Orthopedie in the Netherlands, a company in the manufacturing and provision on custom‐made footwear. The project was funded through a grant from Livit Orthopedie, mainly to cover salary costs of J.B.Z., who was the PhD student on the project.
Bus SA, Zwaferink JB, Dahmen R, Busch‐Westbroek T. State of the art design protocol for custom made footwear for people with diabetes and peripheral neuropathy. Diabetes Metab Res Rev. 2020;36(S1):e3237 10.1002/dmrr.3237
Invited paper for special issue on the diabetic foot, DMRR.
REFERENCES
- 1. Bus SA, Armstrong DG, Gooday C, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):e3274. [DOI] [PubMed] [Google Scholar]
- 2. Lazzarini PA, Jarl G, Gooday C, et al. Effectiveness of offloading interventions to heal foot ulcers in persons with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(S1):e3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bus SA, Lavery LA, Monteiro‐Soares M, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):e3269. [DOI] [PubMed] [Google Scholar]
- 4. van Netten JJ, Raspovic A, Lavery LA, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(S1):e3270. [DOI] [PubMed] [Google Scholar]
- 5. van Netten JJ, Lazzarini PA, Armstrong DG, et al. Diabetic Foot Australia guideline on footwear for people with diabetes. J Foot Ankle Res. 2018;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dahmen R, Haspels R, Koomen B, Hoeksma AF. Therapeutic footwear for the neuropathic foot: An algorithm. Diabetes Care. 2001;24(4):705‐709. [DOI] [PubMed] [Google Scholar]
- 7. Dahmen R, van der Wilden GJ, Lankhorst GJ, Boers M. Delphi process yielded consensus on terminology and research agenda for therapeutic footwear for neuropathic foot. J Clin Epidemiol. 2008;61(8):819‐826. [DOI] [PubMed] [Google Scholar]
- 8. Owings TM, Woerner JL, Frampton JD, Cavanagh PR, Botek G. Custom therapeutic insoles on both foot shape and plantar pressure measurement provide enhanced pressure relief. Diabetes Care. 2008;31(5):839‐844. [DOI] [PubMed] [Google Scholar]
- 9. Bus SA, van Netten JJ, Lavery LA, et al. IWGDF guidance on the prevention of foot ulcers in at‐risk patients with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):16‐24. [DOI] [PubMed] [Google Scholar]
- 10. Arts ML, de Haart M, Waaijman R, et al. Data‐driven directions for effective footwear provision for the high‐risk diabetic foot. Diabet Med. 2015;32(6):790‐797. [DOI] [PubMed] [Google Scholar]
- 11. Arts ML, Waaijman R, de HM, Keukenkamp R, Nollet F, Bus SA. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet Med. 2012;29(12):1534‐1541. [DOI] [PubMed] [Google Scholar]
- 12. Waaijman R, Arts ML, Haspels R, Busch‐Westbroek TE, Nollet F, Bus SA. Pressure‐reduction and preservation in custom‐made footwear of patients with diabetes and a history of plantar ulceration. Diabet Med. 2012;29(12):1542‐1549. [DOI] [PubMed] [Google Scholar]
- 13. Paton J, Bruce G, Jones R, Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: A systematic review. J Diabetes Complications. 2011;25(1):52‐62. [DOI] [PubMed] [Google Scholar]
- 14. Paton JS, Stenhouse EA, Bruce G, Zahra D, Jones RB. A comparison of customised and prefabricated insoles to reduce risk factors for neuropathic diabetic foot ulceration: A participant‐blinded randomised controlled trial. J Foot Ankle Res. 2012;5(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bus SA, Waaijman R, Arts M, et al. Effect of custom‐made footwear on foot ulcer recurrence in diabetes: A multicenter randomized controlled trial. Diabetes Care. 2013;36(12):4109‐4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR. Prevention of recurrent foot ulcers with plantar pressure‐based in‐shoe orthoses: The careful prevention multicenter randomized controlled trial. Diabetes Care. 2014;37(7):1982‐1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lopez‐Moral M, Lazaro‐Martinez JL, Garcia‐Morales E, Garcia‐Alvarez Y, Alvaro‐Afonso FJ, Molines‐Barroso RJ. Clinical efficacy of therapeutic footwear with a rigid rocker sole in the prevention of recurrence in patients with diabetes mellitus and diabetic polineuropathy: A randomized clinical trial. PLoS One. 2019;14(7):e0219537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schaper NC, Van Netten JJ, Apelqvist J, Lipsky BA, Bakker K, International Working Group on the Diabetic Foot , Prevention and management of foot problems in diabetes: A summary guidance for daily practice 2015, based on the IWGDF guidance documents. Diabetes Res Clin Pract. 2017;124:84‐92. [DOI] [PubMed] [Google Scholar]
- 19. Guldemond NA, Leffers P, Schaper NC, et al. The effects of insole configurations on forefoot plantar pressure and walking convenience in diabetic patients with neuropathic feet. Clin Biomech. 2007;22(1):81‐87. [DOI] [PubMed] [Google Scholar]
- 20. Brown D, Wertsch JJ, Harris GF, Klein J, Janisse D. Effect of rocker soles on plantar pressures. Arch Phys Med Rehabil. 2004;85(1):81‐86. [DOI] [PubMed] [Google Scholar]
- 21. Chapman JD, Preece S, Braunstein B, et al. Effect of rocker shoe design features on forefoot plantar pressures in people with and without diabetes. Clinical Biomech. 2013;28(6):679‐685. [DOI] [PubMed] [Google Scholar]
- 22. van Schie C, Ulbrecht JS, Becker MB, Cavanagh PR. Design criteria for rigid rocker shoes. Foot Ankle Int. 2000;21(10):833‐844. [DOI] [PubMed] [Google Scholar]
- 23. Hsi W, Chai H, Lai J. Evaluation of rocker sole by pressure‐time curves in insensate forefoot during gait. Am J Phys Med Rehab. 2004;83(7):500‐506. [DOI] [PubMed] [Google Scholar]
- 24. Prael SFE, Louwerens JK. The influence of shoe design on plantar pressures in neuropathic feet. Diabetes Care. 2003;26(2):441‐445. [DOI] [PubMed] [Google Scholar]
- 25. Hijmans J, Reints R, van Kouwenhove L. Rocker profiles In: Postema K, Schott KH, Janisse D, Rommers GM, eds. Pedorthic Footwear, Assessment and Treatment; 2018:225‐231. [Google Scholar]
- 26. Sonderkamp T, Holtkamp FC. Materials in pedorthic footwear In: Postema K, Schott KH, Janisse D, Rommers GM, eds. Pedorthic Footwear, Assessment and Treatment; 2018:173‐186. [Google Scholar]
- 27. Bus SA, Ulbrecht JS, Cavanagh PR. Pressure relief and load redistribution by custom‐made insoles in diabetic patients with neuropathy and foot deformity. Clin Biomech. 2004;19(6):629‐638. [DOI] [PubMed] [Google Scholar]
- 28. Chen WM, Lee SJ, Lee PV. Plantar pressure relief under the metatarsal heads—Herapeutic insole design using three‐dimensional finite element model of the foot. J Biomech. 2015;48(4):659‐665. [DOI] [PubMed] [Google Scholar]
- 29. Brodtkorb T‐H, Kogler GF, Arndt A. The influence of metatarsal support height and longitudinal axis position on plantar foot loading. Clin Biomech. 2008;23(5):640‐647. [DOI] [PubMed] [Google Scholar]
- 30. Deshaies A, Roy P, Symeonidis PD, LaRue B, Murphy N, Anctil E. Metatarsal bars more effective than metatarsal pads in reducing impulse on the second metatarsal head. Foot. 2011;21(4):172‐175. [DOI] [PubMed] [Google Scholar]
- 31. Hayda R, Tremaine MD, Tremaine K, Banco S, Teed K. Effect of metatarsal pads and their positioning: A quantitative assessment. Foot Ankle Int. 1994;15(10):561‐566. [DOI] [PubMed] [Google Scholar]
- 32. Hsi W, Kang J, Lee X. Optimum position of metatarsal pad in metatarsalgia for pressure relief. Am J Phys Med Rehab. 2005;84(7):514‐520. [DOI] [PubMed] [Google Scholar]
- 33. Lee PY, Landorf KB, Bonanno DR, Menz HB. Comparison of the pressure‐relieving properties of various types of forefoot pads in older people with forefoot pain. J Foot Ankle Res. 2014;7(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lott DJ, Hastings MK, Commean PK, Smith KE, Mueller MJ. Effect of footwear and orthotic devices on stress reduction and soft tissue strain of the neuropathic foot. Clin Biomech. 2007;22(3):352‐359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mueller MJ, Lott DJ, Hastings MK, Commean PK, Smith KE, Pilgram TK. Efficacy and mechanism of orthotic devices to unload metatarsal heads in people with diabetes and a history of plantar ulcers. Phys Ther. 2006;86(6):833‐842. [PubMed] [Google Scholar]
- 36. Nordsiden L, Van Lunen BL, Walker ML, Cortes N, Pasquale M, Onate JA. The effect of 3 foot pads on plantar pressure of pes planus foot type. J Sport Rehab. 2010;19(1):71‐85. [DOI] [PubMed] [Google Scholar]
- 37. Martinez‐Santos A, Preece S, Nester CJ. Evaluation of orthotic insoles for people with diabetes who are at‐risk of first ulceration. J Foot Ankle Res. 2019;12:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hastings MK, Mueller MJ, Pilgram TK, Lott DJ, Commean PK, Johnson JE. Effect of metatarsal pad placement on plantar pressure in people with diabetes mellitus and peripheral neuropathy. Foot Ankle Int. 2007;28(1):84‐88. [DOI] [PubMed] [Google Scholar]
- 39. Farzadi M, Safaeepour Z, Mousavi ME, Saeedi H. Effect of medial arch support foot orthosis on plantar pressure distribution in females with mild‐to‐moderate hallux valgus after one month of follow‐up. Prosthet Orthot Int. 2015;39(2):134‐139. [DOI] [PubMed] [Google Scholar]
- 40. Lin TL, Sheen HM, Chung CT, et al. The effect of removing plugs and adding arch support to foam based insoles on plantar pressures in people with diabetic peripheral neuropathy. J. 2013;6(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bus SA, Haspels R, Busch‐Westbroek TE. Evaluation and optimization of therapeutic footwear for neuropathic diabetic foot patients using in‐shoe plantar pressure analysis. Diabetes Care. 2011;34(7):1595‐1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Owings TM, Apelqvist J, Stenstrom A, et al. Plantar pressures in diabetic patients with foot ulcers which have remained healed. Diabet Med. 2009;26(11):1141‐1146. [DOI] [PubMed] [Google Scholar]
- 43. Zwaferink JB, Berendsen H, Custers W, Paardekoper I, Bus SA. Effect of orthopedic footwear concepts on plantar pressure relief in patients with diabetes mellitus In: Proceedings of the 2016 ESM Scientific Meeting, 28‐30 July 2016. Lisbon, Portugal:2016. [Google Scholar]


