Introduction
Implantable cardioverter-defibrillator (ICD) insertion is generally performed under local anesthesia and sometimes requires anesthesiologic support for analgosedation.
In particular, subcutaneous ICD (S-ICD) and subcutaneous lead implantation requires the creation of a large subcutaneous or intermuscular pocket for the insertion of the device, and a subcutaneous lead tunneling. Generally, pain control is managed using local or general anesthesia.
Given the extremely painful nature of this procedure and the frequent shortage of anesthesiologists, different anesthesiologic techniques such as serratus plane block1 or truncated plane block2 are often administered.
Recently, clinical hypnosis has been gaining popularity as an effective strategy for pain control during surgical and electrophysiological procedures.3, 4, 5 However, to the best of our knowledge, this technique has so far never been used during S-ICD implantation.
This article describes the first case of the use of hypnotic communication and its effectiveness as an adjunctive technique for analgosedation, during S-ICD insertion in a patient with Brugada syndrome and examines its impact on preoperative anxiety, perceived pain, and procedural time perception.
Hypnotic technique
Hypnosis leads to a modified state of mind (paraphysiologic) with muscle relaxation.
The hypnotic workflow may be divided into the following stages:
-
(1)
Checking confirmation of the indication; explanation of the medical care, lowering of inappropriate anxiety and definition of the aim (training)
-
(2)
Focusing patient’s attention in order to be dissociated from the surroundings
-
(3)
Suggestions
-
(4)
Validation of hypnotic status
-
(5)
Reinforcement and consolidation
-
(6)
Posthypnotic suggestions (self-hypnosis)
-
(7)
Discussion (physician-patient comparison)
The patient remains in a status characterized by a change in the external stimuli consciousness and space-time orientation. From the outside the patient seems to be asleep, but from the inside his or her mind is alert and awake and in control. In such a state the patient can be guided to imagine being in a safe and pleasant place. Throughout the procedure the physician reinforces and consolidates the status, interacting verbally with the patient (workflow stage 5). At the end of the procedure, before the patient is reoriented, the operator gives posthypnotic suggestions in order to deal with postprocedural pain and/or further ability in self-hypnosis (workflow stage 6).
The analgesic effect of hypnosis is due to an entrance block at the level of the dorsal horn of the spinal cord, named the “gate control” hypothesis: this “gate” may be opened or closed by physical, emotional, cultural, and behavioral factors, as demonstrated by Facco.6
However, an anesthetist is always present in our electrophysiology (EP) laboratory as a back-up plan in case the patient does not respond to hypnosis as expected.
Case report
A 44-year-old male patient affected by Brugada syndrome with spontaneous type 1 electrocardiography pattern and unexplained syncope was stratified and underwent a single-chamber ICD implantation for primary prevention of ventricular arrhythmias, according to the guidelines in September 2004.
Following implantation, an inappropriate ICD shock was reported owing to electromagnetic interference during an ultraviolet sunbed session. Subsequently, 2 appropriate shocks were also delivered on fast ventricular tachycardias, both in December 2014. Consequently, the patient was treated with hydroquinidine 150 mg 3 times a day, reduced then to 150 mg twice a day for QRS widening.
The device was replaced twice, in March 2010 and again in September 2018 (Medtronic Visia AF MRI XT VR SureScan DVFB2D1, Medtronic, Minneapolis, MN), owing to battery depletion.
In October 2018 the patient was admitted to the emergency room because of an ICD alarm. Investigation of the device showed high impedance both on the pacing channel (>3000 ohms) and on the shock channel (>200 ohms), indicating lead fracture. The patient was then referred to our hospital for treatment.
All options were given to the patient, including extraction and reimplantation,7 and the patient opted to abandon the lead and to carry out an intermuscular S-ICD implantation with the adjunctive use of hypnotic communication as periprocedural analgesia.
Following an evaluation of the patient’s psychological profile, he provided written informed consent, and also gave written consent for the video recording of the whole procedure, including the hypnosis phase and the procedural workflow, which are available for didactic purposes (Supplemental Video). On entering the EP laboratory, the patient was monitored on the surgical bed and before the sterile sheet was applied, a hypnotic status was induced by the implanting physician, who was certified and experienced in clinical hypnosis. It should be noted that in our EP laboratory all the health professionals, both physicians and nurses, are also trained in hypnotic communication.
The operator used, at his discretion, the internal focusing technique (focusing the patient’s attention on an inner perception such as breathing), as described by step 2 of the hypnotic workflow. Step 3 consisted in giving suggestions to the patient, aiming to lower his critical thinking, leading him to a modified state of mind (paraphysiologic) with muscle relaxation and regular breathing, guiding his mind toward a pleasant place or situation. At this point a focused analgesia was induced by means of metaphoric suggestions and hypnotic status was validated by pricking a sharp needle into different parts of the body (workflow step 4).
The patient remained in this status, characterized by a change in the external stimuli consciousness and space-time orientation. From the outside the patient seemed to be asleep but from the inside his mind was alert and awake and in control. During the procedure the operator reinforced and consolidated this status, interacting verbally with the patient (workflow step 5). Toward the end of the procedure, before the patient was reoriented, the operator gave posthypnotic suggestions in order to deal with postprocedural pain and/or further ability in self-hypnosis (workflow step 6). At the end of the procedure, with the patient still on the operating bed, the same hypnosis operator guided the patient out of the hypnotic state, returning him to the present moment (reorientation).
A 2-incision implant technique intervention for S-ICD was performed as previously described.8, 9, 10
The analgesic protocol was carried out by the implanting physician and consisted of the following:
-
(1)
Hypnotic induction (as described above)
-
(2)
Local anesthesia at the site of cutaneous surgical incision on the midaxillary line (lidocaine 200 mg) during the pocket preparation
-
(3)
Intravenous fentanyl 0.05 mg after preparation of the intermuscular pocket, and before the lead tunneling
No other anesthetic support (such as serratus or truncated plane block) was given.
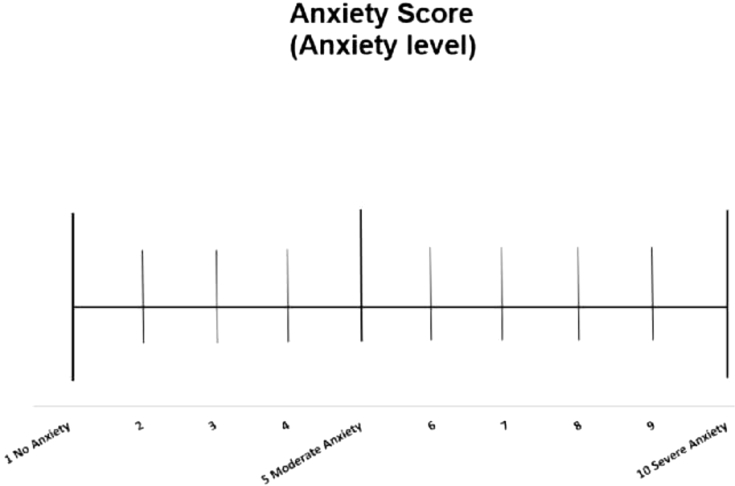
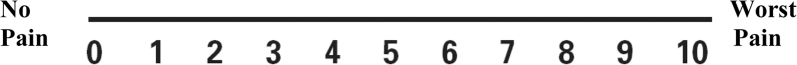
Parameters relating to hypnotic state measured anxiety score, perceived pain, and procedural time perception.
Pain and anxiety perception were quantified using 2 different scores: respectively, Numeric Pain Scale and Anxiety Score Scale, ranging from 0 to 10 (Figures 1 and 2).11
Figure 1.
Anxiety Score Scale.
Figure 2.
Numeric Pain Scale.
The procedure was performed with excellent patient tolerance (Numeric Pain Scale = 0 and Anxiety Score Scale = 0), without any complications.
At the end of the procedure defibrillation testing was carried out in deep sedation with anesthesiologic assistance, using intravenous propofol 40 mg.
The time taken for hypnotic induction was about 4 minutes; the duration of the whole procedure was 50 minutes, while the perceived duration of the procedure by the patient was about 30 minutes.
According to the patient’s wishes, he was discharged 2 days later, asymptomatic. Predischarge device interrogation resulted normal. The patient maintained the ongoing therapy with hydroquinidine 150 mg twice a day.
After 3 months the patient remained asymptomatic.
No S-ICD shocks occurred during the follow-up period.
Discussion
To the best of our knowledge, in this study we examined the first use of hypnotic communication as periprocedural analgesia in S-ICD implantation in a single case study.
Our results suggest that clinical hypnosis performed prior to S-ICD implantation has important beneficial effects:
-
(1)
It allows an invasive and painful procedure such as S-ICD implantation to be performed painlessly.
-
(2)
It reduces anxiety and has a positive impact on pain and procedure time perception, thus reducing the negative psychological impact related to S-ICD implantation.
-
(3)
It has an analgesic synergistic effect, leading to a reduction of painkiller drug use.12,13 Neither serratus plane block nor deep sedation/narcosis was necessary.
This is a single case report on applying hypnosis in S-ICD implantation as analgosedation. However, it is based on the experience of the use of hypnosis for transcatheter ablation in our EP laboratory.3 To the best of our knowledge, no large randomized controlled trials to demonstrate the efficacy and safety of hypnosis in S-ICD implantation have been conducted. However, a wide range of trials have been carried out regarding the use of hypnosis both in percutaneous coronary intervention and in patients undergoing coronary artery bypass graft surgery14,15 and other surgical procedures. They provide overwhelming evidence of the beneficial effects of hypnotic use both preoperatively and postoperatively by reducing stress, anxiety levels, and the analgesic drug intake.
In conclusion, while acknowledging that further trials are needed, our study of the first case of the use of clinical hypnosis as an adjunctive analgosedation technique during S-ICD implantation reinforces the important beneficial effects of this technique, allowing the procedure to be performed painlessly with a reduction of intraprocedural anxiety, time perception, and use of analgesic drugs. Moreover, it is noteworthy that not only is the implanting physician able to perform hypnosis, but also all the other healthcare professionals in the EP laboratory are trained in hypnotic communication, making this technique a routine practice.
Key Teaching Points.
-
•
Hypnotic communication may be an adjunctive technique for subcutaneous implantable cardioverter-defibrillator (S-ICD) implantation that usually requires deep sedation/narcosis.
-
•
Hypnotic communication also reduces anxiety and perceived procedural time, thus reducing the negative psychological impact related to S-ICD implantation.
-
•
Hypnosis influences the “gate control” phenomenon, allowing the synergistic effect with opioid drugs to be exploited.
Acknowledgment
Mattia Peyracchia and Marco Scaglione contributed equally.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.hrcr.2019.12.008.
Appendix A. Supplementary data
Video recording of the whole procedure including the hypnosis phase and the procedural workflow.
References
- 1.Droghetti A., Basso Ricci E., Scimia P., Harizai F., Marini M. Ultrasound-guided serratus anterior plane block combined with the two-incision technique for subcutaneous ICD implantation. Pacing Clin Electrophysiol. 2018;41:517–523. doi: 10.1111/pace.13318. [DOI] [PubMed] [Google Scholar]
- 2.Miller M.A., Bhatt H.V., Weiner N. Implantation of the subcutaneous implantable cardioverter–defibrillator with truncal plane blocks. Heart Rhythm. 2018;15:1108–1111. doi: 10.1016/j.hrthm.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Scaglione M., Battaglia A., Di Donna P. Hypnotic communication for periprocedural analgesia during transcatheter ablation of atrial fibrillation. Int J Cardiol Heart Vasc. 2019;24:100405. doi: 10.1016/j.ijcha.2019.100405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adachi T., Fujino H., Nakae A., Mashimo T., Sasaki J. A meta-analysis of hypnosis for chronic pain problems: a comparison between hypnosis, standard care, and other psychological interventions. Int J Clin Exp Hypn. 2014;62:1–28. doi: 10.1080/00207144.2013.841471. [DOI] [PubMed] [Google Scholar]
- 5.Barbero U., Ferraris F., Muro M., Budano C., Anselmino M., Gaita F. Hypnosis as an effective and inexpensive option to control pain in transcatheter ablation of cardiac arrhythmias. J Cardiovasc Med. 2018;19:18–21. doi: 10.2459/JCM.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 6.Facco E. Hypnosis and anesthesia: back to the future. Minerva Anestesiol. 2016;82:1343–1356. [PubMed] [Google Scholar]
- 7.Kusumoto F.M., Schoenfeld M.H., Wolkoff B.L. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–e551. doi: 10.1016/j.hrthm.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Knops R.E., Olde Nordkamp L.R., de Groot J.R., Wilde A.A. Two-incision technique for implantation of the subcutaneous implantable cardioverter defibrillator. Heart Rhythm. 2013;10:1240–1243. doi: 10.1016/j.hrthm.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Droghetti A., Locatelli A., Casiraghi M., Arupi M., Ragusa M. Totally submuscular implantation of subcutaneous implantable cardioverter defibrillator: a safe and effective solution for obese or oversized patients. Clin Case Rep. 2016;4:1009–1011. doi: 10.1002/ccr3.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boston Scientific; Belgium: 2017. EMBLEMTM S-ICD Electrode Delivery System Manual; pp. 13–36. [Google Scholar]
- 11.Ware L.J., Epps C.D., Herr K., Packard A. Evaluation of the Revised Faces Pain Scale, Verbal Descriptor Scale, Numeric Rating Scale, and Iowa Pain Thermometer in older minority adults. Pain Manag Nurs. 2006;7:117–125. doi: 10.1016/j.pmn.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Elkins G.R., Barabasz A.F., Council J.R., Spiegel D. Advancing research and practice: the revised APA Division 30 definition of hypnosis. Int J Clin Exp Hypn. 2015;63:1–9. doi: 10.1080/00207144.2014.961870. [DOI] [PubMed] [Google Scholar]
- 13.Wobst A.H.K. Hypnosis and surgery: past, present, and future. Anesth Analg. 2007;104:1199–1208. doi: 10.1213/01.ane.0000260616.49050.6d. [DOI] [PubMed] [Google Scholar]
- 14.Baglini R., Sesana M., Capuano C., Gnecchi-Ruscone T., Ugo L., Danzi G.B. Effect of hypnotic sedation during percutaneous transluminal coronary angioplasty on myocardial ischemia and cardiac sympathetic drive. Am J Cardiol. 2004;93:1035–1038. doi: 10.1016/j.amjcard.2003.12.058. [DOI] [PubMed] [Google Scholar]
- 15.Akgul A., Guner B., Çırak M., Çelik D., Hergünsel O., Bedirhan S. The beneficial effect of hypnosis in elective cardiac surgery: a preliminary study. Thorac Cardiovasc Surg. 2016;64:581–588. doi: 10.1055/s-0036-1580623. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video recording of the whole procedure including the hypnosis phase and the procedural workflow.