Figure 13-12.
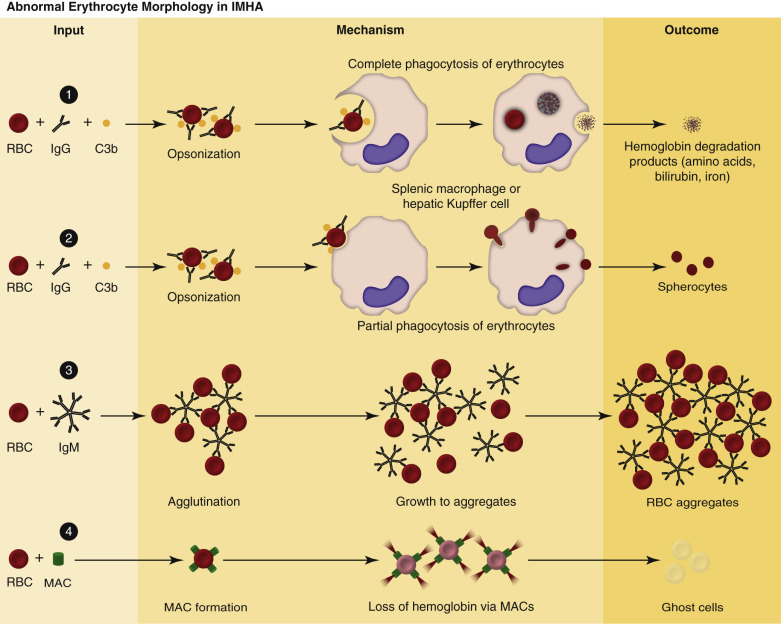
Pathogenesis of Abnormal Erythrocyte Morphologic Changes in Immune-Mediated Hemolytic Anemia.
1, Red blood cell (RBC) degradation. Antierythrocyte antibodies bind RBC surface antigens, resulting in RBC opsonization by immunoglobulins (mainly immunoglobulin G [IgG]) and complement (primarily C3b). Immunoglobulin- or C3b-bound RBCs are phagocytized and digested by sinusoidal macrophages. 2, Spherocytes. Spherocytes form when the membrane of immunoglobulin- or C3b-bound RBCs are phagocytized by macrophages, without removing the entire RBC from circulation. Compared to normal erythrocytes, spherocytes appear smaller, more eosinophilic, and lack central pallor. 3, RBC aggregation (agglutination). RBC aggregation occurs when antierythrocyte immunoglobulins (immunoglobulin M [IgM] or high concentrations of IgG) bind multiple erythrocytes simultaneously. 4, Ghost cells. Antierythrocyte antibodies bind RBC surface antigens, resulting in complement activation and formation of the membrane attack complex (MAC). MACs form membrane pores, resulting in rupture of RBCs, and the release of hemoglobin into the circulation. Ghost cells are RBC membrane remnants that lack cytoplasm (hemoglobin).
(Courtesy Dr. K.M. Boes, College of Veterinary Medicine, Virginia Polytechnic Institute and State University; and Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
