Figure 25-16.
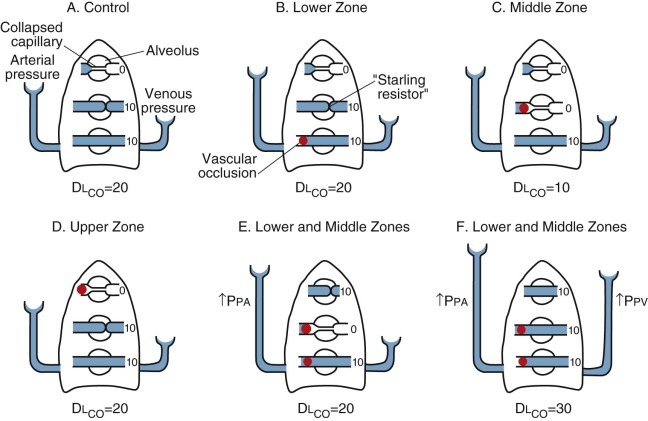
Theoretical model showing the effect of pulmonary arterial pressure (Ppa) and pulmonary venous pressure (Ppv) on pulmonary capillaries at different levels of the lungs.
The magnitude of Ppa or Ppv is indicated by the height of the fluid columns. For simplicity, the pressure in alveoli (Palv) is assumed to be equal to atmospheric pressure. Single-breath carbon monoxide diffusing capacity (DlCO) is given in arbitrary units indicating the relative contribution of various zones of the lung. A, In the control state, at the bottom of the lung, both Ppa and Ppv are greater than Palv, and both keep the capillaries open. In the middle zone, Ppa is greater than Palv and Ppv, so Ppa holds capillaries open. (The exact anatomy of capillaries in the zone in which Palv is greater than Ppv is unknown; in the diagram, the compressed segment at the end of the capillary is meant to suggest a “Starling resistor” effect.) In the upper zone, Palv is greater than Ppa and Ppv, and capillaries are “collapsed.” B, When arterial inflow is occluded to the lower zone (indicated by red solid sphere), Ppv is greater than Palv, so the capillaries in this zone remain distended and DlCO is unchanged. C, When arterial inflow to the middle zone is occluded, Palv is greater than Ppv and capillaries in this area are collapsed, so there is a decrease in DlCO. D, When arterial inflow to the upper zone is occluded, the capillaries are already collapsed, so there is no change in DlCO. E, When arterial inflows to the lower and middle zones are occluded simultaneously, capillaries in the middle zone may collapse. However, if Ppa increases, capillaries in the upper zone may become distended, and the net result may be no change in DlCO. Under these circumstances, if Ppv also increases (F), DlCO may actually increase.
(Modified from Nadel JA, Gold WM, Burgess JH: Early diagnosis of chronic pulmonary vascular obstruction: value of pulmonary function tests. Am J Med 44:16–25, 1968.)
