Summary
China has made rapid progress in four key domains of global health. China's health aid deploys medical teams, constructs facilities, donates drugs and equipment, trains personnel, and supports malaria control mainly in Africa and Asia. Prompted by the severe acute respiratory syndrome (SARS) outbreak in 2003, China has prioritised the control of cross-border transmission of infectious diseases and other health-related risks. In governance, China has joined UN and related international bodies and has begun to contribute to pooled multilateral funds. China is both a knowledge producer and sharer, offering lessons based on its health accomplishments, traditional Chinese medicine, and research and development investment in drug discovery. Global health capacity is being developed in medical universities in China, which also train foreign medical students. China's approach to global health is distinctive; different from other countries; and based on its unique history, comparative strength, and policies driven by several governmental ministries. The scope and depth of China's global engagement are likely to grow and reshape the contours of global health.
Introduction
In only three decades, China's global engagement has accelerated from closed autarky to open engagement; from relative isolation to integration into the world system; from a low-income to a middle-income country; and from an aid recipient to an aid donor. As a global demographic and economic giant, China's prominence in global health should not be surprising. With 18% of the world's population, China weighs heavily in all global health metrics, such as life expectancy, disease burden, and health systems. As the world's largest trading nation, its movement of goods and services is associated with transfer of health technologies, diseases, and risk factors. In health knowledge and strategies, China has a rich history of traditional medicine and has pioneered many health-care innovations.
China's ascendency has generated many questions and some concerns. A common assumption is that China uses foreign aid to secure energy and natural resources and to expand export markets.1, 2 China's claim of aid with “no strings attached”, is considered by some to encourage corruption, weaken accountability, or ignore human rights.3 The international press has reported delayed and muddled notification of infectious outbreaks, and much news of exported contaminated Chinese manufactured products. China is sometimes perceived as working alone and insufficiently cooperating with other countries.
In this Review, we attempt to address the following questions: What is China's role in global health? Is China's engagement distinctive or similar to other countries? What does the evidence illuminate of China's global health engagement?
Data sources
China, similar to most countries, has no single official source of data for global health because of the multiplicity of governmental stakeholders, the absence of a national strategy on global health, and the unclear borderline between aid and trade investments.4 A study5 by NYU's Wagner School has estimated China's foreign aid to Africa, Latin America, and southeast Asia from 2002 to 2007. Strange and coauthors6 estimated all previous estimates of Chinese development finance to Africa. The State Council of the Chinese Government, the highest body of state administration, published white papers summarising China's overall foreign aid in 2011 and 2014. None of the above estimations disaggregated or separately reported health aid.7, 8
We thus have resorted to an extensive search of data from multiple Chinese sources—the State Council, the ministries of health, commerce, education, foreign affairs, and science and technology. Reports from provincial governments, Chinese embassies abroad, and the press were searched. Altogether, we obtained data from 529 sources—425 from various websites, 70 from statistical yearbooks, 23 from regular reports, and 15 from newspapers. Data sourced came from 15 groups of organisations, including 227 sources from the ministry of commerce, 35 from the health ministry (National Health and Family Planning Commission), and 15 from ministry of education. The overwhelming proportion of these data sources are in Chinese (95%), with less than 5% in English. All data sources are shown in the appendix. Interviews were done with dozens of former officials, medical team members, and key provincial authorities to collect first-hand information.
Not surprisingly, the data quality is mixed, often incomplete, and the fragments need to be matched and fitted together. The Chinese Government is essentially the only source of information, without other sources of independent verification. Reports of classification and nomenclature often do not follow international standards. A common limitation is the mixing of stock data versus flow data.
Our compiled data, nevertheless, generate what we believe to be the most robust estimation possible. Matching and piecing together the fragments allows inconsistencies to be double checked for consistency. Most inconsistencies relate to exact numbers, but estimation of the general order of magnitude is believed to be reasonably robust. All data sources for this Review are shown in the appendix in both original Chinese and translated English.
Analyses and results
After introducing a framework, we present sections on China's work in health aid, health security, health governance, and knowledge exchange.
China's participation in global health has deep historical roots, not only just in recent years. In the first millennium, knowledge of medical cures were transmitted by the Silk Road that facilitated exchange between China, India, the Middle East, and Europe.9 In the 20th century, some Chinese health crises such as the Manchurian plague epidemic captured the attention of neighbouring countries of the international community.10 China has historically been the origin of many infectious epidemics and a source of key health innovations of breakthroughs such as the barefoot doctor (a term that emerged in the 1960s and 1970s, which refers to farmers who received minimal basic medical and paramedical training and worked in rural China to promote basic hygiene, preventive health care, family planning, and treat common illnesses. The name comes from southern farmers, who would often work barefoot in the rice paddies), and artemisinin, an effective antimalaria drug developed from plant-based Chinese traditional medicine.11, 12
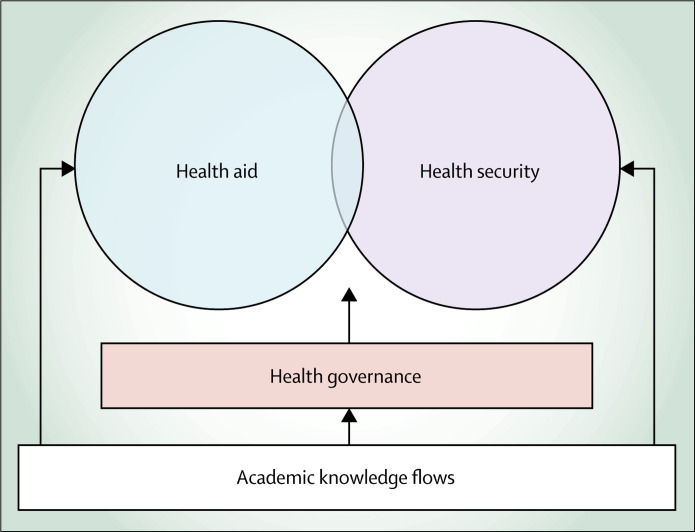
Because there is no universal consensus for the definition of global health, some approaches focus on transnational health risks, which lie beyond the reach of national governments, whereas other approaches stress the global commitment and responsibility to address health inequities and to support health.13 We have adopted a framework of global health as characterised by health and related transnational flows of diseases, people, money, knowledge, technologies, and ethical values.14, 15, 16 Four domains capture these globalisation processes (figure 1 ). First, health aid aims to advance global health equity. It is the traditional area of official development assistance (ODA) coordinated by organisation for economic cooperation and development (OECD) countries. Second, global health security should be ensured by management of interdependence in global health and mutual protection against shared and transferred risks, such as epidemic diseases. Third, health governance is needed for global stewardship to set ground rules as mediated by health diplomacy. Fourth, knowledge exchange is needed, which includes the sharing of lessons and knowledge production, ownership, and application worldwide. Knowledge centrally affects all four pillars of global health, and global health governance is recognised to be central to all four domains (figure 1).
Figure 1.
Framework of global health
On the basis of this framework, China's modern timeline might be demarcated by five landmarks. First, in 1963, China sent its first overseas medical team to Algeria, followed 6 years later by the donation of its first hospital in Tanzania.17 The explicitly articulated purpose of China's health aid was to further political solidarity as part of China's foreign policy. Second was China's economic openings after 1978, which launched the dramatic transformation of China from a low-income to a middle-income country, leading to China qualifying as an aid recipient followed by increasingly becoming an aid donor.17 Third, starting from 2000, China has hosted a series of Forums on China-Africa Cooperation, with each forum announcing yet another major aid pledge—eg, hospital construction, malaria control, and high education scholarships (2007–09); training of health workers and artemisinin drug donation (2010–12); and brightness action (eye care) campaign (2013–15).18, 19 Fourth, global engagement greatly accelerated after 2001 when China entered the World Trade Organization (WTO), an event that marked China's joining almost all international bodies. Finally, and perhaps most dramatically, the 2003 severe acute repiratory syndrome (SARS) epidemic underscored both China's neglect of its health sector and the reality that China's global trade cannot be done without mutual health protection.20
Health aid
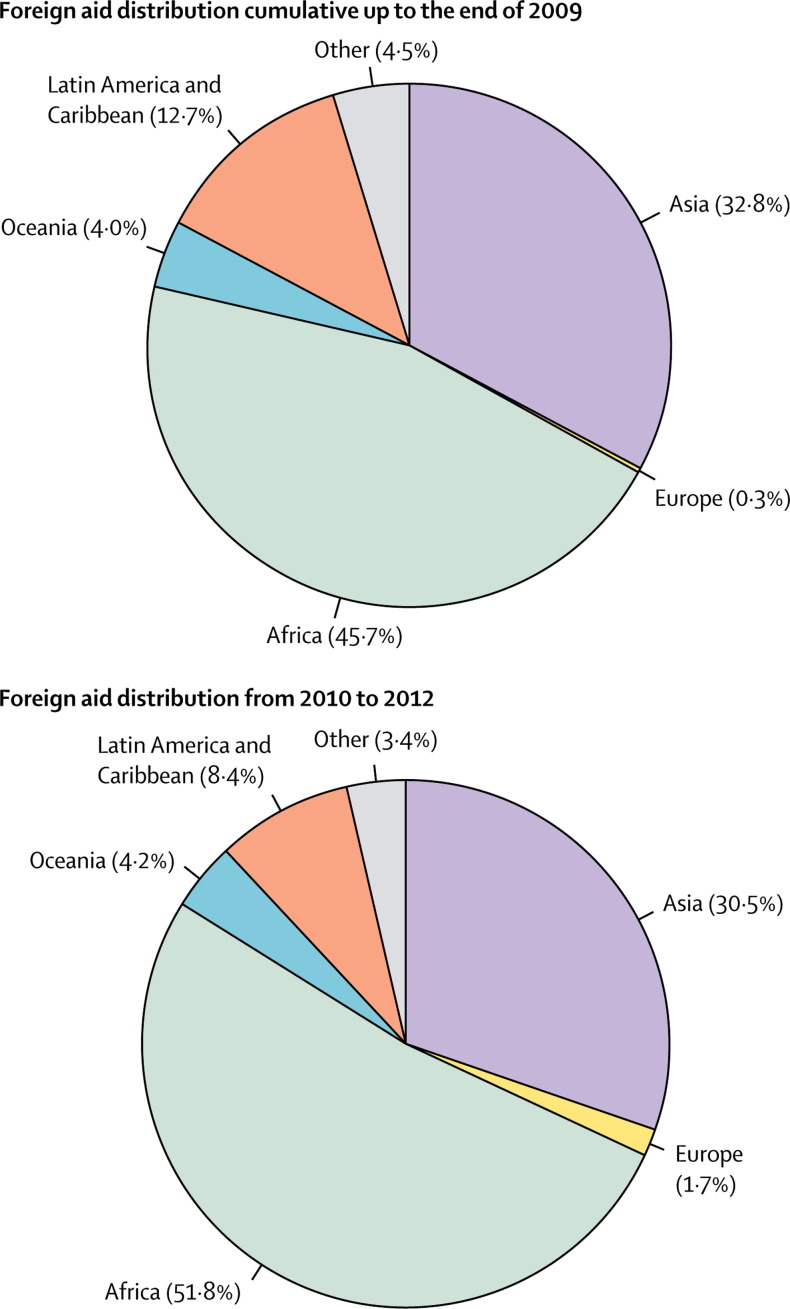
In recent years, the State Council has published two white papers in April, 2011, and July, 2014, summarising China's foreign aid by volume and type. The 2011 white paper reports foreign aid of US$37·6 billion accumulated up to and including 2009 in three categories: grants of $15·6 billion; concessional loans of $10·8 billion; and interest-free loans of $11·2 billion. This amount is fairly close to another estimate of China's foreign aid at $40·5 billion cumulative from 1950 to 2010, reaching $3·9 billion annually by 2010.21, 22 The aid increased significantly during the period of 2010–12, reaching an average of $4·8 billion per year, of which the grants accounted for 36·2%.8 Figure 2 shows that African countries received 46% of all aid, with Asia receiving about a third (33%) and Latin America receiving around 13%, before the end of 2009. The share for African countries increased to 51·8% during the past 3 years, whereas Latin America received relatively less.8 Another estimate computed China aid to Africa in 2008, at $1·2 billion in comparison with Japan at $1·6 billion and USA at $7·2 billion.22
Figure 2.
China's foreign aid by region
Chinese aid in health is provided in five categories: medical teams, construction of hospitals, donation of drugs and equipment, training of health personnel, and malaria control. The largest share of health aid is spent on medical teams and donated facilities. The financial value of Chinese in-kind health aid is difficult to estimate. Crudely, from 2007 to 2011, we estimated the value of Chinese medical teams in Africa to be about $60 million annually, with donated facilities at a similar amount. Total health aid to Africa annually has been estimated at about $150 million. Understanding of the type of health support offered rather than the precise volume of funding might be more important. Different from most OECD donors, China does not offer general sectoral support, albeit small cash grants given to several countries in recent years. Its health aid uses a project approach.7 The in-kind provision in the five categories is based on Chinese competencies. Health seems to constitute only a small proportion of the total Chinese aid. Health aid is mainly in donation form, whereas most of China's overall foreign aid is offered as either concessional or interest-free loans.
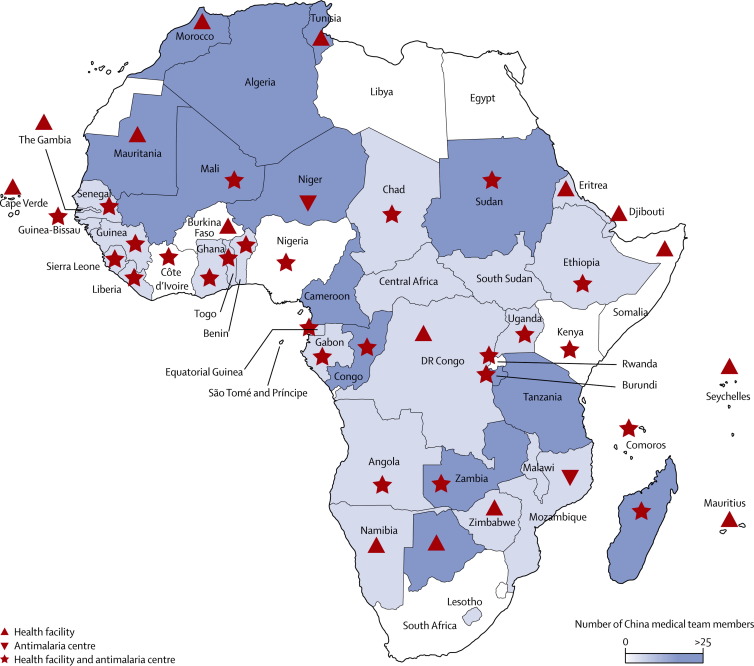
Since 1963, under the protocol on the dispatch of medical teams signed between the government of China and the recipient countries, about 23 000 Chinese medical workers have been sent to about 66 countries to provide services to an estimated 270 million people. At the end of 2013, 1171 Chinese medical workers were working in 113 medical centres in 49 countries. 42 of the countries are in Africa, and the remaining seven are mainly small countries—four in Asia, one in Europe, one in South America, and one in Oceania.23 The table shows African countries in 2013 according to medical teams, aided facilities, and malaria control programmes, along with the Chinese provinces twinned to each country. Figure 3 shows China health aid to Africa with countries shaded according to density of medical team coverage and demarcated by aided facilities and malaria control. The distribution shows wide coverage of nearly all African countries with a higher density of medical teams in western and eastern Africa regions. The largest and most powerful African countries such as South Africa, Nigeria, and Kenya do not have Chinese medical teams. Chinese selection of hosting countries is based on country request and the joint decision by China's ministries of health, foreign affairs, and finance. The medical teams are overseen by the Chinese embassy economic and commercial counsellor's offices.
Table.
China medical teams, facilities, and malaria control by countries
| Twinned Chinese province |
China medical teams |
Number of aided facilities | Antimalaria centre | |||
|---|---|---|---|---|---|---|
| Year started | Number of up to 2013 | Number of members (2013) | ||||
| Algeria | Hubei | 1963 | 23 | 86 | 0 | No |
| Angola | Sichuan | 2009 | 3 | 11 | 2 | Yes |
| Benin | Ningxia | 1978 | 19 | 26 | 3 | Yes |
| Botswana | Fujian | 1981 | 13 | 46 | 1 | No |
| Burkina Faso | Beijing | 1976 | 10 | 0 | 1 | No |
| Burundi | Qinghai | 1987 | 15 | 29 | 1 | Yes |
| Cameroon | Shanxi | 1974 | 16 | 45 | 6 | Yes |
| Cape Verde | Heilongjiang + Sichuan | 1984 | 15 | 8 | 2 | No |
| Central Africa | Zhejiang | 1978 | 15 | 16 | 2 | Yes |
| Chad | Jiangxi | 1978 | 10 | 12 | 1 | Yes |
| Comoros | Guangxi | 1994 | 9 | 11 | 1 | Yes |
| Congo | Tianjin | 1967 | 22 | 33 | 4 | Yes |
| Côte d'lvoire | .. | .. | .. | .. | 1 | Yes |
| Democratic Republic of the Congo | Hebei | 1973 | 15 | 18 | 1 | No |
| Djibouti | Shanxi | 1981 | 17 | 14 | 2 | No |
| Egypt | 0 | .. | .. | .. | 0 | No |
| Equatorial Guinea | Guangdong | 1971 | 26 | 27 | 1 | Yes |
| Eritrea | Henan | 1999 | 8 | 18 | 1 | No |
| Ethiopia | Henan | 1974 | 17 | 15 | 1 | Yes |
| Gabon | Tianjin | 1977 | 17 | 17 | 2 | Yes |
| The Gambia | Guangdong | 1977 | 9 | 0 | 5 | No |
| Ghana | Guangdong | 2009 | 3 | 11 | 3 | Yes |
| Guinea | Beijing | 1968 | 23 | 19 | 2 | Yes |
| Guinea-Bissau | Guizhou + Sichuan | 1976 | 14 | 17 | 4 | Yes |
| Kenya | 0 | .. | .. | .. | 4 | Yes |
| Lesotho | Hubei | 1997 | 9 | 8 | 0 | No |
| Liberia | Heilongjiang | 1984 | 7 | 9 | 2 | Yes |
| Libya | Beijing | 1983 | 5 | 0 | 0 | No |
| Madagascar | Gansu | 1975 | 19 | 30 | 1 | Yes |
| Malawi | Shaanxi | 2008 | 3 | 16 | 0 | No |
| Mali | Zhejiang | 1968 | 23 | 31 | 1 | Yes |
| Mauritania | Heilongjiang | 1968 | 30 | 27 | 5 | No |
| Mauritius | 0 | .. | .. | .. | 2 | No |
| Morocco | Shanghai | 1975 | NA* | 79 | 6 | No |
| Mozambique | Sichuan | 1976 | 19 | 17 | 0 | Yes |
| Namibia | Zhejiang | 1996 | 9 | 4 | 1 | No |
| Niger | Guangxi | 1976 | 17 | 37 | 1 | Yes |
| Nigeria | 0 | .. | .. | .. | 1 | Yes |
| Rwanda | Inner Mongolia | 1982 | 16 | 20 | 3 | Yes |
| São Tomé and Principe | Heilongjiang + Sichuan | 1976 | 11 | 0 | 0 | No |
| Senegal | Fujian | 1975 | 15 | 13 | 1 | Yes |
| Seychelles | Shandong | 1985 | 14 | 6 | 1 | No |
| Sierra Leone | Hunan | 1973 | 16 | 10 | 1 | Yes |
| Somalia | Shanghai + Jilin | 1965 | 13 | 0 | 2 | No |
| South Africa | 0 | .. | .. | .. | 0 | No |
| South Sudan | Anhui | 2012 | 1 | 12 | 1 | No |
| Sudan | Shaanxi | 1971 | 31 | 42 | 2 | Yes |
| Swaziland | 0 | .. | .. | .. | 0 | No |
| Tanzania | Shandong + Jiangsu | 1964 + 1968 | 48 | 46 | 3 | Yes |
| Togo | Shanghai + Shanxi | 1974 | 20 | 20 | 2 | Yes |
| Tunisia | Jiangxi | 1973 | 20 | 45 | 1 | No |
| Uganda | Yunnan | 1983 | 16 | 8 | 1 | Yes |
| Zambia | Henan | 1978 | 16 | 28 | 1 | Yes |
| Zimbabwe | Hunan | 1985 | 13 | 10 | 3 | No |
| Non-African countries | NA | NA | 66 | 163 | 25 | No |
NA=not applicable.
The number of teams in Morocco is not calculated like other teams so is not presented here. Data sources are shown in the appendix.
Figure 3.
China health aid to Africa medical teams, facilities, malaria control, in 2012
Data sources in the appendix.
Medical teams are financed by the health aid budget in the health ministry (except the basic salaries), which is responsible for dispatching medical teams. Selected countries are twinned to specific Chinese provinces with public hospitals and local medical schools responsible for staffing, supervising, and partially funding the medical teams.24 Some practical criteria such as willingness and workload are used to match Chinese provinces and recipient countries in the twinning arrangement.
The number of members in medical teams ranges from a half dozen people to nearly 100, usually working out of Chinese donated hospitals and clinics. Most workers are clinicians, and most teams include a leader and a translator. Public health skills are usually not included. Medical teams mainly provide clinical services, especially for specialties in short supply—eg, surgery, gynaecology, and obstetrics. The average duration of an overseas assignment is 2 years, with team members receiving housing and food plus enhanced salaries. Over the period of 2010–12, these medical teams working in 54 countries had provided about 7 million medical consultations and treatments.8 Panel 1 describes some of these medical teams in southern Sudan and the Democratic Republic of the Congo.
Panel 1. Chinese medical teams work and perspectives.
29 physicians, two nurses, two chefs, two translators, and one medical engineer from Shaanxi Province constituted China's 30th medical team to Sudan in 2007–09. The 15th Chinese team from Hebei Province to the Democratic Republic of the Congo arrived in 2012, consisting of a team leader, 13 physicians (including one in Chinese traditional medicine), two nurses, one French translator, and one chef. For both teams, their primary role was to provide clinical care to patients. An ancillary function was to mentor, train, and improve the skill of local health workers. Medical teams were self-sufficient, bringing all their own supplies, equipment, and medicines. In response to questionnaires, team members commented positively on their experiences. Higher salaries, financial subsidies, and allowances from both central government and employers (about a six-fold increase) operated as important incentives. Reported constraints included language barriers, unaccustomed disease profiles, poor facilities and equipment, unstable water and electricity supply, and homesickness. If the opportunity were offered, nearly all would be willing to serve again.25, 26
Since 1970, China has constructed more than a hundred health facilities overseas with its health aid. China accelerated its assistance in the construction of hospitals and clinics—from 2010 to 2012, China has supported about 80 construction projects of health facilities.8 Most of these facilities are donated, and only a few are built as part of large infrastructure projects funded by Chinese loans. African countries were the recipients of more than three-quarters of the donated facilities. Although most countries have received at least one facility, some have received up to 6. These facilities are mostly so-called turnkey operations, for which Chinese construction firms build the facility for transfer to local authorities.
Malaria control has recently been prioritised. Control programmes are undertaken through 30 anti-malaria centres, featuring artemisinin based on Chinese traditional medicine. Panel 2 describes an ambitious Chinese programme of malaria eradication with mass drug administration with artemisinin on the Comoros Islands.
Panel 2. Traditional Chinese medicine to eradicate malaria?
Malaria eradication in some countries had been successful with dichlorodiphenyltrichloroethane, and hopes have focused on new vaccines. But a professor of Chinese traditional medicine from Guangzhou University of Chinese Medicine is leading an unprecedented effort to eradicate malaria on the Comoros Islands with traditional Chinese medicine. Starting in 2007 on Moheli Island where 23% of the 36 000 residents were carriers of Plasmodium falciparum, disease prevalence has dropped to 0·3% in 4 months with mass administration of artemisinin and piperaquine, donated by China's ministry of commerce. 5 years later, the Chinese team extended this programme to Anjouan, an island of 350 000, reducing the prevalence of P falciparum carriers from 19% to 0·5%. Last year, the efforts were expanded to the 420 000 residents of Grande Comore, the country's largest island. The project goal is malaria eradication in the 900 000 people of the Comoros by 2016.27
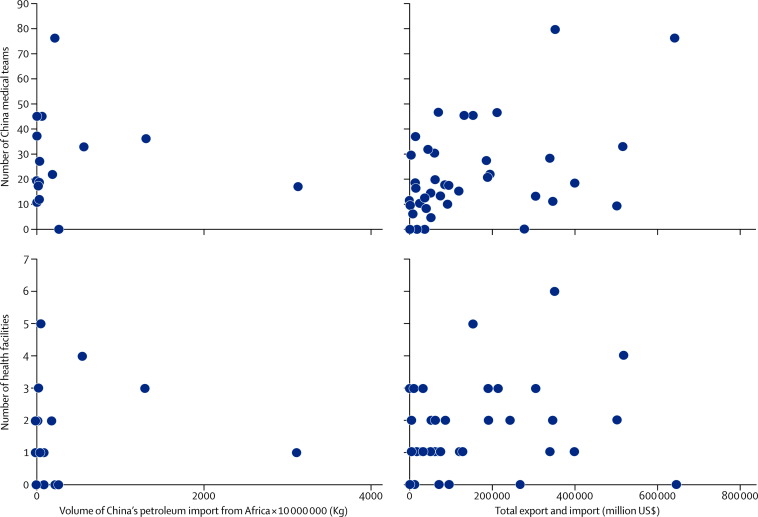
The question of whether health aid is mainly driven by China's commercial interest is not easy to investigate. Much depends upon interpretation of underlying motivation. For example, Chinese aid to Africa might be viewed as either helping the world's poorest countries or building friendship with the origin of much of the world's energy and natural resources and potential export markets. A comprehensive analysis of this question would need access to data not currently available. As a preliminary first step, we attempted to examine correlations between health aid and commercial economic indicators. Regression analysis of African countries with variables of health aid (medical teams, donated facilities, malaria control) and economic interests (petroleum imports, China's foreign investment, and China's imports and exports) yielded no significant pattern. Figure 4 shows four scatter-plots of China health aid and African trade. In the four diagrams, individual African countries are plotted according to health and commercial indicators. The scatter-plots did not show any association between medical aid and economic interests. Spearman's Rank Correlation and t test analysis for the period of 2002–11 showed no significant findings of correlations. These preliminary analyses should not be interpreted as conclusive.
Figure 4.
China health aid and African trade, 2011
Health security
A core component of global health is mutual health protection against international transfer of health risks, which shows health interdependence. Transborder movement of infectious diseases, contaminated goods and products, air pollution, and globally pooled CO2 are prime examples.
For China, the 2003 SARS epidemic was a crisis with serious economic and political consequences. Both disease control and international cooperation were delayed. Chinese errors made in the early stage of SARS have been acknowledged and have generated strong corrective measures, both domestically and internationally.28 Domestic measures include major re-investment in the public health system via the Chinese Center for Disease Control and Prevention (CDC), including development of the world's largest real-time electronic surveillance system.29 International efforts include active participation and leadership in many international forums that foster cooperation in compliance of disease reporting and control, as shown by the initiation of the UN resolution on enhancement of capacity-building in global public health in 2003, and the joint International Pledging Conference on Avian and Human Pandemic Influenza with China, the European Commission, and the World Bank held in Beijing in 2006.30, 31, 32
Subsequent management of infectious outbreaks such as avian influenza A H7N9 virus shows that China recognises the importance of strict adherence to the International Health Regulations. In the 2003 SARS outbreak, China needed 87 days between first case detection and report to WHO and another 46 days for joint teams to investigate the outbreak. For H7N9 one decade later, less than half the days lapsed between first case and report to WHO and the initiation of joint investigations.33, 34, 35
Infections can move in several directions. China has been the destination of cross-border infectious transmissions. In 2011, a polio epidemic was imported from Pakistan into China's Xinjiang province.36 It took more than a year for China to return to polio-free status after making arduous efforts and expending large resources.37 Similarly, China has been threatened by the import of dengue fever, malaria, and several other transmissible diseases.38, 39
Cross-border risks can also accompany the import and export of commodities. As the world's largest exporter of manufactured products, China, of course, transfers health risk overseas. News reports have been plentiful of contamination in Chinese exports of toothpaste, lead paint, milk products, and heparin.40, 41, 42, 43 These safety concerns are not limited to exporters. China has also been a destination in the dumping of contaminated chemicals from richer to poorer countries;44 these safety hazards are of equal concern to the Chinese public. These concerns might be why China has upgraded its State Food and Drug Administration (SFDA) to the status of a ministry with larger budget, increased staff, and stronger regulatory powers.45
Environmental pollution also moves across national boundaries. Air pollutants in China have been cited as causing acid rain damage to forests in Korea and Japan.46, 47 China is today the world's largest emitter of carbon dioxide, contributing substantially to global climate change.48 To tackle air pollution, China's State Council released an action plan setting a 5-year road map for air pollution control.49 Its implementation deserves tracking for monitoring and evaluation of control effect.
Health governance
Health governance sets ground rules for global stewardship of diverse activities. Across the board, China has become an active member of the world system, opening with China's economic reform and accelerating after its entry into the WTO in every aspect—eg, political (UN), financial (World Bank, International monetary fund), economic (WTO), and military (arm control and disarmament). China has joined almost all specialised UN bodies—WHO, UNICEF, UNFPA, UNAIDS—and also the multilateral health funds. Backed by strong political support, a Chinese national has been elected twice as the Director-General of WHO.
China is an active member of the governing body of WHO, UNAID, and the Global Fund, and an increasing number of Chinese experts participate in WHO's global normative work. China is the only developing country that hosts two codex committees—CCFA (Codex Committee on Food Additives) and CCPR (Codex Committee on Pesticide Residues), including leading the drafting of some international codex standards.
Data underscore the participation of China in global governance. China's receipt of net official development assistance and official aid peaked at about $1800 million in 2005, had steadily decreased to a third of that amount by 2010, and is already disappearing as China increasingly becomes an aid donor rather than an aid recipient.50 From 1998 to 1999, China's receipt and contribution to WHO were equal at about $5 million. By 2012–13, China's assessed contribution to WHO had increased to $30 million, while WHO funding to China had remained at baseline.51 In parallel with this increase in funding, the number of Chinese staff members in WHO has expanded. Whereas in 1999, there were only 12 Chinese officials working in WHO, that number had tripled to 34 by 2012, although Chinese staff in WHO are still under-represented.52 Additionally, based on the newly released white paper, China allocated $280 million to support the Global Fund and other international organisations in 2010–12.8
Global health participation by China has been mainly governmental. In non-governmental stakeholders, growth in the international participation of some academic universities, business, and industry has occurred. China has very few non-governmental organisations (NGOs) and thus the Chinese are mostly absent from global civil society forums. A few international NGOs work in China, but few have achieved official registration from the Chinese Government. It will take substantial time, if ever, before China's civil society becomes active in global health.
Knowledge exchange
Knowledge is both local and global, and its production, ownership, exchange, and application have global dimensions. China has much to share with and much to learn from the rest of the world.
In medicine, strategy, and implementation, China has had some spectacular accomplishments, worthy contributions to the world's knowledge pool. Chinese traditional medicine offers many health-enhancing technologies—ranging from ephedrine to acupuncture.53, 54, 55 In the 1930s, village health workers were field tested, and later re-engineered as the barefoot doctor.11 China's three-tier rural health system was established soon after the founding of the People's Republic.56 The Alma Ata movement for primary health care took great encouragement from China in showing what barefoot doctors could do at the community level. The three decades after the founding of the People's Republic in 1949 witnessed some of the steepest advances of mortality control in human history.57 China's management of common infectious diseases, maternal-child health, tropical disease control, malaria and schistosomiasis containment, mass social hygiene campaigns, and recent achievement of near-universal health coverage are worthy of documentation as valuable lessons.
Panel 3 describes an innovative grant by UK Government's Department for International Development (DFID) to foster research by, and capacity building for Chinese universities and other institutions to disseminate and share Chinese lessons with other countries.
Panel 3. Dissemination of China's lessons abroad.
When announcing aid cessation to China in 2012, the UK's Department for International Development (DFID) provided an unusual tie-off grant (£12 million) for the China–UK Global Health Support Program (GHSP).58 The programme aims to strengthen China's global health cooperation through capacity building by (1) distilling of and dissemination of positive Chinese experiences; (2) understanding of best practice in health development cooperation; (3) contributing to global health policy and governance; and (4) application of China lessons and best practices abroad. The programme is establishing a China network on global health in universities and research institutes that started in 2014 with eight awards to Peking University, Fudan University, China Center for Disease Control and Prevention, various units of the health ministry, and other Chinese units.59 This unusual grant has the overarching goal of encouraging Chinese institutions to partner with institutions from low-income and middle-income countries to work for better world health.
For the future, China aspires to be a worldwide knowledge leader and it has fast growing research and development investments in biomedicine. Chakma60 reported China's biomedical research and development at $8·4 billion in 2012, in comparison with USA ($119 billion), Europe ($82 billion), and Japan ($37 billion). The absolute size of these figures might undervalue Chinese investments because the lower salaries, cost of infrastructure, and cost of operations in China might not be captured fully by purchasing power parity-adjusted values. Strikingly, China's investments since 2007 have increased annually at 33% in comparison, for example, to −2% for the USA.60 China, moreover, houses laboratories for most of the major pharmaceutical companies. It has advanced genetic research capacity as shown by its genetic sequencing of the H7N9 virus within 7 days of isolation and identification.34 China is also a growing producer and exporter of generic products. China aspires to be a powerhouse in the discovery and production of new drugs and vaccines in global health.
China's medical universities are increasingly undertaking research and education in global health. In the past year, several new multidisciplinary centres of global health were built in such universities as Peking, Fudan, Sun Yatsen, Central South (Xiangya), Wuhan, Kunming, and Peking Union Medical College.61 These universities are developing a Chinese curriculum in global health and pursuing research in Chinese health policy and systems. In these endeavours, Chinese collaboration with international universities has been growing. Joint programmes in global health have been launched with Duke University, Graduate Institute of Geneva, Georgetown University, Harvard, London School of Hygiene and Tropical Health, and University of Washington. The new Duke-Kunshan University, a partnership between Duke, Wuhan University, and the City of Kunshan near Shanghai, is featuring global health as one of its masters degree programmes aimed at both Chinese and overseas students.62 Panel 4 describes the formation of a China Consortium of Universities in Global Health, inspired by its counterpart in North America.
Panel 4. China Consortium of Universities for Global Health (CCUGH).
Sparked by the North American model, a CCUGH was established in November, 2013, by ten founding universities: Central South University, Chinese University of Hong Kong, Duke-Kunshan University, Fudan University, Kunming University, Peking University, Peking Union Medical College, Sun Yat-sen University, Wuhan University, and Zhejiang University. CCUGH aims to promote global health development in Chinese universities through sharing of knowledge and resources, fostering of cooperation, advancement of educational curriculum, promotion of research, provision of advisory services, and facilitation of Chinese participation in global health activities abroad. CCUGH also encourages long-term partnerships with overseas universities for global health education, training, research and consultative services.61, 63
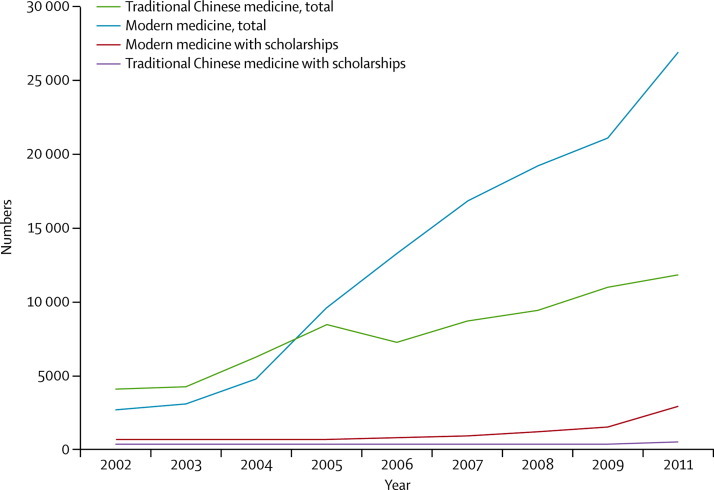
China supports government officials, technical professionals, and young people from developing countries to participate in training and education programmes in China. In 2010–12, the government provided 76 845 scholarships for such programmes, of which many were health related.8 China's medical universities also train foreign medical students. According to the data from the China Education Yearbook, in 1999–2011, China trained 240 123 foreign medical students, who constitute 13% of all foreign students in 2011. For that year, the ministry of education reported almost 27 000 foreign medical students studying modern medicine and 12 000 studying traditional Chinese medicine.64, 65 By 2013, China had extended authorisation to 52 medical schools to admit foreign students who will study medicine in English.66 Figure 5 shows the rapid increase of foreign medical students and scholarships in China in 2002–11. Although foreign interest in traditional medicine is high, most foreign students register for modern medicine. About 10% of the foreign medical students receive Chinese Government scholarships that might be regarded as part of China's foreign health aid. Chinese medical schools charge foreign students higher than Chinese tuition fees,67 and the schools acknowledge foreign students as a source of school revenue. In 2011, many of the students came from neighbouring Asian countries, such as India, Japan, Pakistan, South Korea, and southeast Asia.
Figure 5.
Foreign medical students and scholarships in China, 2002–11
Data sources in the appendix.
Discussion
Our most salient finding is China's distinctive mode of engagement in global health. China's health aid volume is small, but the mode is distinctive, driven by China's health capabilities and national experiences. Unlike many other traditional donors, China's in-kind aid focuses more on some important aspects of the health system. China's overall global engagement follows a very different path from developed countries partly because it has no colonial experience nor did it participate in shaping the American-led post-World War 2 world order. China was inward-looking until it expanded into the global economy in 1978. Over the ensuing three decades, China has had large shifts from a low-income to a middle-income country, and from aid recipient increasingly to aid donor. The spread of its foreign aid throughout the breadth of Africa presumably reflects both efforts to solidify friendship politically, promote mutually beneficial economic gains, and compete with Taiwan for political friendship.68 China's health aid is embedded in the dynamic shifting of foreign and economic policies. The opening in 1978 marked a shift from economic development serving foreign policy to foreign policy serving economic development because China's association, for example, with Africa, has developed from a political one in the 1970s to a broader economic-based and trade-based engagement.69, 70 These are all defining characteristics of China's engagement in global health.
China's global health work, unfortunately, does not seem to rank highly in government agencies. Health has been assigned a lower position than political and commercial affairs. Taking advantage of both domestic and international resources and accessing both domestic and international markets is China's explicit national development strategy.71 These powerful economic motives drive much of China's global engagement, including its engagement in Africa, to the point where the dividing line between trade and aid become blurred and hard to demarcate.70 Health aid is only a very small adjunct to these much larger and more powerful forces.
China's overseas forces include several government agencies. As a result, improved interministerial coordination is a necessary development for the evolution of a coherent overall engagement in global health. Formulation of a China global health strategy could help bring coherent policy and harmonised action, because it would compel the articulation of specific health and humanitarian objectives in Chinese governmental policies. An explicit China global health strategy would provide a stronger context for NGOs and private sector overseas participation.
China's bilateral approach differs substantially from its multilateral approach. Although China's bilateralism takes an independent approach, China's multilateral strategy is full participation, joining as a regular member and complying with its responsibilities and privileges in UN bodies such as WHO. The records show that China respects and complies with rules governing multilateral institutions in all affairs—health, trade, migration, environment, and other aspects of global governance. China has increased its contribution to multilateral funding pools, such as the Global Fund from $2 million per year in 2003, to $5 million per year in 2012. How important China will become as a major donor to these pooled funds is uncertain. Some see the early actions as symbolic gestures of cofunding, whereas others hope that the size of the Chinese economy will propel it to become a financial leader of multilateral funds. The New Development Bank being established by BRICS countries aims to compete with the World Bank and International Monetary Fund, which is one example of how China has debatably played a leadership role.72
Most important is the avoidance of over-simplification. No country's international engagement is free from political or economic motives—eg, Europe colonialism, US millennium development accounts, or Sweden–Vietnam partnership during the American war.73 And no single modality of foreign aid has proven to be more effective or more sustainable.74, 75 Although China's health aid is generally appreciated by recipient official statements, there are indeed complaints about the scale of China's intrusion, access to natural resources, and the trade market in Africa. But energy resource-based trade structure with Africa does not occur only in China; it occurs with all major African trading partners. The most fundamental improvement is to increase the capacity for independent development, to which all partners in Africa should contribute.
China's global health engagement is difficult to attribute to one motivation factor. Chinese driving forces are undoubtedly several and complex—political, economic, social, and humanitarian. China's approach has been characterised as pragmatic that “combines the utilitarian logic of reaping material benefit, the realist objective of expanding its global power and influence, the neo-liberalist interest in pursuing absolute gains from international cooperation, and the constructivist attempt to become a responsible stakeholder in the system”.76
China's global health engagement will probably grow substantially with expanding budgets, more projects, and more staff sent abroad. China will pursue its own distinctive approach, not copying the developed world model; Chinese Government policy and indigenous professional capacity will be key. The first generation of Chinese professionals with experience and foreign language fluency is emerging along with stronger global health institutions. Given this trajectory, one should assume global health will likely be re-shaped by China's participation, with its structures and processes increasingly accommodating Chinese characteristics.
This online publication has been corrected. The corrected version first appeared at thelancet.com on September 26, 2014
Acknowledgments
Acknowledgments
We thank Haomin Yang, Yang Li, and Jing Bai for their work on data collection, data analysis, and research assistance.
Contributors
PL led and coordinated the authors’ group. All authors participated in study design, data collection, analysis, interpretation, and paper writing and editing. LC and ZL produced the first draft.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Emory Global Health Institute . Case study: can global sanitation 2020 contribute to China's prosperity? E-mory Global Health Institute; Atlanta: 2013. [Google Scholar]
- 2.Zweig D, Jianhai B. China's global hunt for energy. 2005. http://www.foreignaffairs.com/articles/61017/david-zweig-and-bi-jianhai/chinas-global-hunt-for-energy (accessed Jan 16, 2014).
- 3.Hanson S. China, Africa, and oil. Council on Foreign Relations 6. 2008. http://www.washingtonpost.com/wp-dyn/content/article/2008/06/09/AR2008060900714.html (accessed Jan 16, 2014).
- 4.Haan A. Will China change international development as we know it? J Int Dev. 2011;23:881–908. [Google Scholar]
- 5.Lum T, Fischer H, Fomez-Granger J, Leland A. China's foreign aid activities in Africa, Latin America, and Southeast Asia. 2009. http://fas.org/sgp/crs/row/R40361.pdf (accessed Nov 8, 2013).
- 6.Strange A, Parks B, Tierney M. China's development finance to Africa: a media-based approach to data collection. 2013. http://international.cgdev.org/sites/default/files/chinese-development-finance-africa_0.pdf (accessed Jan 18, 2014).
- 7.Information Office of the State Council White Paper on China's Foreign Aid. 2011. http://english.gov.cn/official/2011-04/21/content_1849913.htm (accessed Jan 18, 2014).
- 8.Information Office of the State Council White Paper on China's Foreign Aid, The People's Republic of China, Beijing. 2014. http://news.xinhuanet.com/english/china/2014-07/10/c_133474011.htm (accessed Jan 18, 2014).
- 9.Sen A. Passage to China. New York Rev Books. 2004;51:61–63. [Google Scholar]
- 10.Summers W. The great Manchurian plague of 1910–1911: the geopolitics of an epidemic disease. Yale University Press; New Haven: 2012. [Google Scholar]
- 11.Sidel V. The barefoot doctors of the People's Republic of China. N Engl J Med. 1972;286:1292–1300. doi: 10.1056/NEJM197206152862404. [DOI] [PubMed] [Google Scholar]
- 12.Butler A, Wu Y. Artemisinin (Qinghaosu): a new type of antimalarial drug. Chem Soc Rev. 1992;21:85–90. [Google Scholar]
- 13.Kickbusch I, Buse K. Moving global health governance forward. Making sense of global health governance: a policy perspective. 2009. http://graduateinstitute.ch/files/live/sites/iheid/files/shared/summer/GHD%202009%20Summer%20Course/Kickbusch_Chapter%2015_Moving%20Global%20Health%20Governance%20Forward.pdf (accessed Feb 11, 2014).
- 14.Koplan J, Bond T, Merson M. Towards a common definition of global health. Lancet. 2009;373:1993–1995. doi: 10.1016/S0140-6736(09)60332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frenk J. Health Professionals for a new century. 2011. http://www.who.int/workforcealliance/media/speeches/JulioFrenk_Presentation.pdf (accessed Feb 11, 2014).
- 16.Ng N, Ruger J. Global health governance at a crossroads. 2011. http://www.ghgj.org/Ng&Ruger.pdf (accessed Feb 11, 2014). [PMC free article] [PubMed]
- 17.Li A. Chinese medical cooperation in Africa. 2011. http://nai.diva-portal.org/smash/get/diva2:399727/FULLTEXT02 (accessed Feb 11, 2014).
- 18.King K. Aid within the wider China-Africa partnership: a view from the Beijing Summit. 2006. http://www.cctr.ust.hk/materials/conference/china-africa/papers/King,Kenneth.pdf (accessed Feb 13, 2014).
- 19.Forum on China-Africa Cooperation The fifth ministerial conference of the forum on China-Africa cooperation Beijing Action Plan. July 23th, 2012. http://www.focac.org/eng/zxxx/t954620.htm (accessed Feb 25, 2014).
- 20.Chan L, Chen L, Xu J. China's engagement with global health diplomacy: was SARS a watershed? PLoS Med. 2010;7:e1000266. doi: 10.1371/journal.pmed.1000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Global Health Strategies initiatives Shifting paradigm: how the BRICS are reshaping global health and development. 2012. http://www.g20civil.com/documents/199/472/ (accessed Jan 22, 2014).
- 22.Bräutigam D. Chinese development aid in Africa: what, where, why, and how much? 2011. http://www.american.edu/sis/faculty/upload/brautigam-chinese-aid-in-africa.pdf (accessed Feb 20, 2014).
- 23.Zhu N. China to strengthen cooperation with Africa on health. 2013. http://news.xinhuanet.com/english/china/2013-08/16/c_132637291.htm (accessed Jan 19, 2014).
- 24.Bliss K. Key players in global health: how Brazil, Russia, India, China, and South Africa are influencing the game. 2010. http://csis.org/files/publication/101110_Bliss_KeyPlayers_WEB.pdf (accessed Jan 23, 2014).
- 25.Jiang X, Characteristics of China-Africa health collaboration The case of Democratic Republic of Congo. Chin J Health Policy. 2014;7:64–68. [Google Scholar]
- 26.Wang K, Gimbel S, Malik E, Hassen S, Hagopian A. The experience of Chinese physicians in the national health diplomacy programme deployed to Sudan. Glob Public Health. 2012;7:196–211. doi: 10.1080/17441692.2011.594450. [DOI] [PubMed] [Google Scholar]
- 27.Xu J. Fighting malaria. 2013. http://usa.chinadaily.com.cn/china/2013-09/03/content_16938925.htm (accessed Jan 19, 2014).
- 28.Chan L, Lee P, Chan G. China engages global health governance: processes and dilemmas. Glob Public Health. 2009;4:1–30. doi: 10.1080/17441690701524471. [DOI] [PubMed] [Google Scholar]
- 29.Wang L, Wang Y, Yang G, Ma J, Wang L, Qi X. China Information System for Disease Control and Prevention (CISDCP) 2013. http://pacifichealthsummit.org/downloads/HITCaseStudies/Functional/CISDCP.pdf (accessed Feb 23, 2014).
- 30.Permanent Mission of the People's Republic of China to the UN Statement by Chinese permanent representative Wang Guangya at the 58th Session of the UN introducing a draft resolution entitled “enhancing capacity building in global public health”. 2003. http://www.china-un.org/eng/chinaandun/socialhr/health/t40032.htm (accessed Feb 25, 2014).
- 31.WHO International Pledging Conference on Avian and Human Pandemic Influenza. 2006. http://www.who.int/dg/lee/speeches/2006/flumeeting_beijing/en/ (accessed Feb 25, 2014).
- 32.Chen Z. China's Health Diplomacy: sharing experience and expertise. 2012. http://wsb.moh.gov.cn/mohgjhzs/s7952/201205/54917.shtml (accessed Feb 25, 2014) (in Chinese).
- 33.Wikipedia Influenza a virus subtype H7N9. 2013. http://en.wikipedia.org/wiki/Influenza_A_virus_subtype_H7N9#Reported_cases_in_2013 (accessed Dec 12, 2013).
- 34.WHO China—WHO Joint mission on human infection with avian influenza A (H7N9) virus. 2013. http://www.who.int/influenza/human_animal_interface/influenza_h7n9/ChinaH7N9JointMissionReport2013.pdf (accessed Feb 25, 2014).
- 35.BBC news Timeline: SARS virus. 2004. http://news.bbc.co.uk/2/hi/asia-pacific/2973415.stm (accessed Feb 25, 2014).
- 36.WHO Controlling the polio outbreak in China. 2012. http://www.wpro.who.int/immunization/documents/CHN_PolioOutbreakControl_ENG.pdf (accessed Feb 23, 2014).
- 37.China Daily Xinjiang remains polio-free. 2012. http://usa.chinadaily.com.cn/china/2012-12/20/content_16033801.htm (accessed Feb 23, 2014).
- 38.China Daily China tightens quarantine for malaria, dengue. 2012. http://www.chinadaily.com.cn/china/2012-03/26/content_14917561.htm (accessed Feb 23, 2014).
- 39.Xinhua News Agency China Regions on Alert for malaria, dengue Fever. 2006. http://www.china.org.cn/english/health/187700.htm (accessed Feb 23, 2014).
- 40.Halle M, Long G. Elements of a sustainable trade strategy for China. 2010. http://www.iisd.org/pdf/2010/elements_sustainable_trade_china.pdf (accessed Jan 20, 2014).
- 41.Haller C. Made in China. J Med Toxicol. 2008;4:141–142. doi: 10.1007/BF03160969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xiu C, Klein K. Melamine in milk products in China: examining the factors that led to deliberate use of the contaminant. Food Policy. 2010;35:463–470. [Google Scholar]
- 43.Mitka M. Contaminated heparin seized by FDA. JAMA. 2008;300:2597. doi: 10.1001/jama.2008.786. [DOI] [PubMed] [Google Scholar]
- 44.Clapp J. Toxic exports: the transfer of hazardous wastes from rich to poor countries. Cornell University Press; Ithaca: 2001. [Google Scholar]
- 45.Tremblay J. China upgrades drug safety agency–people's congress: move aims to raise quality of food and drug supply. 2013. http://cen.acs.org/articles/91/i11/China-Upgrades-Drug-Safety-Agency.html (accessed Feb 2, 2014).
- 46.Terada H, Ueda H, Wang Z. Trend of acid rain and neutralization by yellow sand in east Asia—a numerical study. Atmos Environ. 2002;36:503–509. [Google Scholar]
- 47.Okudera A, Hayashi N, Yoshioka K. Air pollution from China reaches Japan, other parts of Asia. 2013. https://ajw.asahi.com/article/economy/environment/AJ201302010087 (accessed Feb 16, 2014).
- 48.Rogers S, Evans L. World carbon dioxide emissions data by country: China speeds ahead of the rest. 2011. http://www.theguardian.com/news/datablog/2011/jan/31/world-carbon-dioxide-emissions-country-data-co2 (accessed Jan 20, 2014).
- 49.Ministry of environmental protection. the People's Republic of China The state council issues action plan on prevention and control of air pollution introducing ten measures to improve air quality. 2013. http://english.mep.gov.cn/News_service/infocus/201309/t20130924_260707.htm (accessed Feb 16, 2014).
- 50.World Bank Data: net official development assistance and official aid received (current US$) http://data.worldbank.org/indicator/DT.ODA.ALLD.CD (accessed Feb 23, 2014).
- 51.WHO Financial and auditing reports from World Health Assembly, from WHA51 to WHA66. http://apps.who.int/gb/e/e_wha66.html (accessed Jan 22, 2014).
- 52.WHO Human resources: annual report, 2000–2013. World Health Assembly 53-66. http://www.who.int/mediacentre/events/governance/wha/en/ (accessed Jan 22, 2014).
- 53.Zhu Y-P. Chinese materia medica: chemistry, pharmacology and applications. CRC Press; Florida: 1998. [Google Scholar]
- 54.Deng L. Chinese acupuncture and moxibustion. 2001.
- 55.Normile D. Asian medicine. The new face of traditional Chinese medicine. Science. 2003;299:188–190. doi: 10.1126/science.299.5604.188. [DOI] [PubMed] [Google Scholar]
- 56.Eggleston K, Li L, Meng Q, Lindelow M, Wagstaff A. Health service delivery in China: a literature review. Health Econ. 2008;17:149–165. doi: 10.1002/hec.1306. [DOI] [PubMed] [Google Scholar]
- 57.Banister J, Hill K. Mortality in China 1964–2000. Popul Stud. 2004;58:55–75. doi: 10.1080/0032472032000183753. [DOI] [PubMed] [Google Scholar]
- 58.UK Department for International Development Global health support programme supports shared international development objectives. 2013. https://www.gov.uk/government/news/global-health-support-programme-supports-shared-international-development-objectives (accessed Feb 23, 2014).
- 59.DFID China UK Global Health Support Programme (GHSP) 2013. http://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=4&ved=0CEMQFjAD&url=http%3A%2F%2Fiati.dfid.gov.uk%2Fiati_documents%2F3717707.doc&ei=Yc4KU4amOKm0sQTYqYDwDw&usg=AFQjCNFXEzzcpDT0wfxPfRkroDexqMxpxA&sig2=_xOFOuHkBLludKiUGvY8tg&bvm=bv.61725948,d.cWc (accessed Jan 27, 2014).
- 60.Chakma J, Sun GH, Steinberg JD, Sammut SM, Jagsi R. Asia's ascent–global trends in biomedical R&D expenditures. N Engl J Med. 2014;370:3–6. doi: 10.1056/NEJMp1311068. [DOI] [PubMed] [Google Scholar]
- 61.Duke Kunshan university, and the leading Chinese universities launch new global health consortium. 2013. https://dku.edu.cn/en/leading-chinese-universities-launch-new-global-health-consortium (accessed Feb 23, 2014).
- 62.Duke Kunshan University Liberal education meets Chinese tradition. 2014. https://dku.edu.cn/en/about (accessed Feb 23, 2014).
- 63.Yu J. China consortium of universities for global health established in Beijing. 2013. http://bynew.bjmu.edu.cn/art/2013/11/19/art_11308_90066.html (accessed Feb 17, 2014) (in Chinese).
- 64.Ministry of Education of People's Republic of China . China education yearbook. People's education press; Beijing: 2012. [Google Scholar]
- 65.Ministry of Education of People's Republic of China . Brief statistics of international students in China. Advanced Education Press; Beijing: 2012. [Google Scholar]
- 66.Ministry of Education of People's Republic of China New list of Chinese medical institutions admitting International Students for Academic Year 2013–2014. 2013. http://www.admissions.cn/news/363674.shtml (accessed Jan 27, 2014).
- 67.Ministry of Education of People's Republic of China Interim provisions to control the quality of foreign students’ undergraduate education (English class) in China. 2007. http://www.fmprc.gov.cn/ce/cepk/chn/wenhuafuwu/t352633.htm (accessed Aug 1, 2014).
- 68.McKee M, Atun R. Beyond borders: potential gaps in the international system of public health surveillance. Lancet. 2006;367:1224–1226. doi: 10.1016/S0140-6736(06)68520-6. [DOI] [PubMed] [Google Scholar]
- 69.Ho S. China: foreign policy serves domestic development. 2012. http://www.voanews.com/content/china-foreign-policy-serves-domestic-development-countrys-sovereignty-141555643/180776.html (accessed Jan 19, 2014).
- 70.Zhong J. China's priorities in Africa: enhancing engagements. 2014. http://www.chathamhouse.org/sites/files/chathamhouse/field/field_document/20140613ChinasPrioritiesAfrica.pdf?dm_i=1TYF,2M2U0,BRVILH,9JKI3,1 (accessed July 10, 2014).
- 71.Party Literature Research Center of the CPC Central Committee . Collection of important documents since third plenary session. People's Publishing House; Beijing: 1982. (in Chinese). [Google Scholar]
- 72.Sky J. Emerging economics to launch development. 2014. http://www.dw.de/emerging-economies-to-launch-development-bank/a-17779926 (accessed May 7, 2014).
- 73.Stuckler D, McKee M. Five metaphors about global-health policy. Lancet. 2008;372:95–97. doi: 10.1016/S0140-6736(08)61013-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Moon S, Omole O. Development assistance for health: critiques and proposals for change. 2013. http://www.chathamhouse.org/sites/files/chathamhouse/public/Research/Global%20Health/0413_devtassistancehealth.pdf (accessed Feb 13, 2014). [DOI] [PubMed]
- 75.Deaton A. The great escape: health, wealth, and the origins of inequality. Princeton University Press; Princeton: 2013. [Google Scholar]
- 76.Huang Y. China and Global Health Governance. 2012. http://www.indiana.edu/~rccpb/pdf/Huang%20RCCPB%2026%20Health%20May%202012.pdf (accessed Feb 26, 2014).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.