Table 3.
Quotes to illustrate patterns and barriers in conveying equipoise
| Quote no. | Patterns in conveying equipoise |
|---|---|
| Q1 | “We have two treatment options, active monitoring versus radiotherapy. We don't know which is best and we're doing a trial, a study, to work out with patients which is the best treatment.” (Cons_Decline14_Neurosurgeon1) |
| Q2 | “If you go into the trial, whichever arm you are in… you would be followed closely with scans, we'd keep a close eye on you, we'd do some extra tests for your sort of brain function and things like that.” (Cons_Consent2_Neurosurgeon1) |
| Q3 | “It causes, in the short term, some additional fatigue, maybe feeling a bit headachy, and you lose your hair in the areas that we treat.” (Cons_Decline28_Radiation‐oncologist2) |
| Q4 | “And more what we're concerned about is the longer‐term side‐effects of radiotherapy, so it can affect your cognitive function.” (Cons_Decline27_Radiation‐oncologist3) |
| Q5 | “[Radiotherapy] is an everyday treatment for around six weeks … got to admit it's efforts on your behalf to… I think the travelling is as much a bother than anything else.” (Cons_Consent31_Radiation‐oncologist4) |
| Q6 | “The general UK practice and also internationally a lot, is that if the tumour's been macroscopically removed…if it's all visible bits have been taken out, often people will elect for a period of surveillance and then wait for the tumour…to come back and then have radiotherapy. So this trial is really trying to answer that question. Is it, in fact, better to have up‐front radiotherapy or to have a period of surveillance.” (Cons_Decline27_Radiation‐oncologist3) |
| Q7 | “What is active monitoring? What does that entail? … when my surgeon told me … I thought the one option was just radiotherapy, if not, being left to it.” (Int_Decline12) |
| Q8 | “If you are going to have the radiotherapy… it can have some side effects, especially in people like you, that you're young, radiotherapy can affect certain parts of the brain.” (Cons_Decline_Neurosurgeon7) |
| Q9 | “And the other thing you need to factor in is your age… because you are older, you have less, you know, you haven't got as many years to live as if you were 40.” (Cons_Decline4_Neurosurgeon1) |
| Q10 | “The other thing you'd have to think about… is the fact that you live in [2 hours away] [laughter].” (Cons_Neurosurgeon1) “Yes, it's a long way to come… I would just probably rent something.” (Cons_Consent5) |
| Practitioners’ barriers to conveying equipoise | |
| Q11 | “I think the very young are difficult and also the very old who would struggle with radiotherapy. So it's always the extremes of age that are a bit more tricky, but otherwise there's a big, big trench in the middle we should be able to hopefully hone in on… Once you're up above your mid 70s then… radiotherapy isn't an easy option unless you're very fit.” (Int_Radiation‐oncologist5) |
| Q12 | “I think it will affect like higher cognitive functions. If somebody obviously works in a highly skilled professional, you know. It depends also on the pre‐morbid status and it depends on what expectations are from him professionally or socially, because in some people it may not be very obvious but in others it will be more obvious… that is a stumbling block I think for the study.” (Int_Neurosurgeon7) |
| Q13 | “Certainly if there's no brain invasion, then surveillance [monitoring] is appropriate… if it's a standard tumour then I would say that surveillance is appropriate… This trial is using quite a high dose of radiotherapy. Sometimes with grade two we know historically it's the lower dose but for this study, 'cause there is evidence for it in other studies that it's acceptable, they've used the higher dose of radiotherapy.” (Int_Radiation‐oncologist8) |
| Q14 | “It's back to the fact that if you're offering a treatment up front you need to discuss all the side effects of the treatment and because you're offering, you're basically offering a treatment against what could be perceived as a no treatment option… what you're then talking about from the negative point of view are the things that will actually, could potentially be an issue for patients if they are randomised to the radiotherapy arm.” (Int_Radiation‐oncologist6). |
| Q15 | “When [practitioners’ are] talking about treatments they have to point out the potential side effects… these days everybody's so keen about covering their backs.” (Int_ResearchNurse9) |
| Q16 | “Personally I think [radiotherapy side effects are discussed in detail] because [practitioners] want, they don't want anyone to complain back, saying, ‘this happened to me and is it because of radiotherapy?’” (Int_ResearchNurse10) |
| Q17 | “Radiotherapy does have side effects and we've got to be honest about that… And, you know, I see a lot of people after radiotherapy, some are fine but a lot have ongoing side effects and, you know. So I would still want, I wouldn't want my role to be taken away. I would still want to be, because I feel I'm the, the patient advocate as it were… I'm not there to sell a trial to somebody that I don't think wants it.” (Int_Neurosurgeon11) |
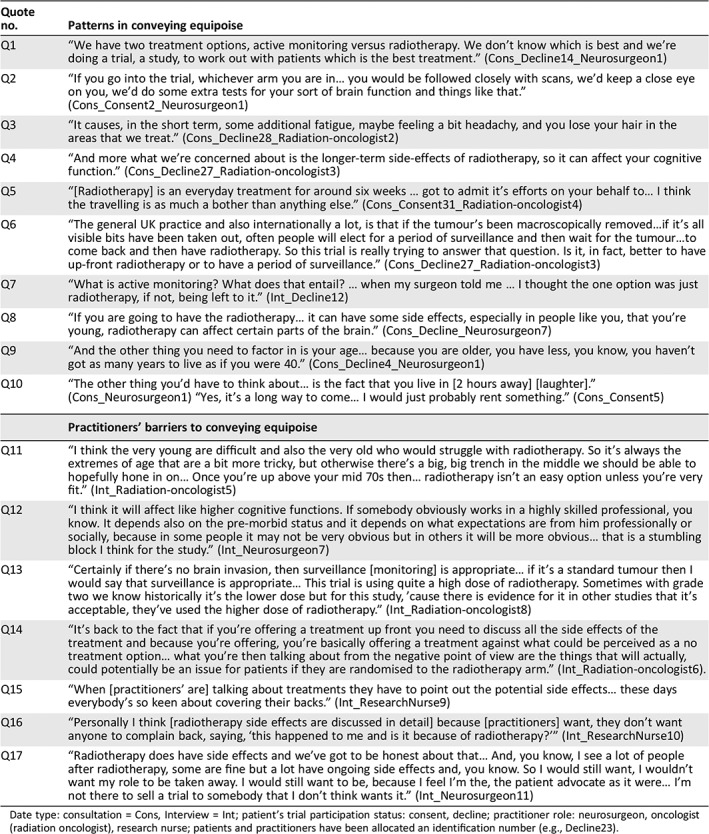
Date type: consultation = Cons, Interview = Int; patient's trial participation status: consent, decline; practitioner role: neurosurgeon, oncologist (radiation oncologist), research nurse; patients and practitioners have been allocated an identification number (e.g., Decline23).
