Table 4.
Quotes to illustrate patterns and barriers to exploring patients’ treatment preferences
| Quote no. | Patterns in exploring patients’ treatment preferences |
|---|---|
| Q18 | “Do you have a thought either way? I know when you first came you were like can I have radiotherapy?” (Cons_Consent22_Neurosurgeon1) |
| Q19 | “Do you have any questions about either way to go?” (Cons_Decline30_Radiation‐oncologist6) |
| Q20 | “The more I'm swinging more towards surveillance rather than radiotherapy… but I understand the need for research and anything that will reduce recurrence, you know.” (Cons_ Consent22); “…There are obviously advantages and disadvantages of the therapy. The, if you're in a study and randomised to radiotherapy, the potential advantage is that it reduces the risk of regrowth but there is a potential, you know, a potential risk of side effects, as we discussed.” (Cons_Neurosurgeon1) |
| Q21 | “To be honest with you, I've made my decision [not to take part]…. because of the timeline of my holiday and coming back to work.” (Cons_Consent25) … “When is your holiday? … Okay, right. So we have until… until [date] to start you, ‘cause we have 12 weeks… As far as going back to work is concerned, I would certainly have thought that there would be no reason, if we put the sort of timescale that you're looking at anyway.” (Cons_Radiation‐oncologist6) |
| Q22 | “To just be monitored and see if [the tumour] does comes back, then six months down the line to have to… that's not what I really want.” (Cons_Consent6) “… the reality is that the risk of it coming back is only about three or four out of ten, so it's still more likely that it won't… And even with radiotherapy, there's no guarantee that you wouldn't be any better… I think our default, given that we don't know, is we don't tend to offer radiotherapy up front if they're not in the trial because we don't think there's a proven benefit.” (Cons_Radiation‐oncologist2) |
| Q23 | “I do want to go ahead with it [the trial] … I want to do whatever is going to get rid of it …” (Cons_Decline12); “Well I think the first thing to say that it has been got rid of in the sense that what was there [the surgeon] has done a fantastic resection… what we would offer you today, because one is to consider entry into the trial… and then if you, if you decided you didn't want to go into the trial I think, being the age that you are, probably our best option would be to survey you in the first instance.” (Cons_Radiation‐oncologist5) |
| Q24 | “I'm [older age] this year… and I just think to myself, you know, it's took a long while for it to grow hasn't it? … And this is in the back of my mind, you know, whether to proceed with the other ongoing thing what you've just told me about.” (Cons_ Decline17); “Yeah. I mean I think it's fair to say that the chances of, you know, you running into further problems from this I think are hopefully quite small.” (Cons_Radiation‐oncologist2) |
| Q25 | “I'm quite… well the thing is I'm quite happy like, you know, [other surgeon] said… they've tried and… most of the tumour is taken out now…” (Cons_Decline26) “Absolutely, that is the most important thing… and you're so well so I think… because you are so young and the main question is people like you, we don't know what the future holds and what is the best thing and want to give the best to our patients, so have a little think about it…” (Cons_Neurosurgeon7) |
| Practitioners’ barriers to exploring patients' treatment preferences | |
| Q26 | “If a patient says, oh no, no, I don't want radiotherapy my aunt had that. I would always ask them, you know, what did your aunt have treated, when was it, how long ago, what side effects did they have, that your treatment is going to be very different because we're treating the brain and we've got modern radiotherapy… Whatever they say you've got to get more detail, you can't just accept it at face value that they're saying there's a problem with the treatment.” (Int_Radiation‐oncologist12) |
| Q27 | “We have to be very, very careful we're not coercing people to do something that they're not keen to do… So if a patient says I'm not interested in it, then I can't say, ‘I know you say that but I think you should think about’, I think that would be seen as coercion.” (Int_Radiation‐oncologist12) |
| Q28 | “The GP advised them not to participate in the study… but then I was like, you know, you don't really want to push patients, so yeah, I was like, okay that's fine, I respect that…” (Int_Neurosurgeon13) |
| Q29 | “I don't like specifically ask the question, which treatment you would prefer… because generally people are coming to see me for me to, as me as the expert to kind of outline the options… They're sort of coming to me because they want answers to their diagnosis.” (Int_Radiation‐oncologist3) |
| Q30 | “I would think that, if clinicians aren't doing that [exploring treatment preferences], then it suggests that they're trying to get through the consultation quickly.” (Int_Radiation‐oncologist12) |
| Q31 | “Maybe time pressure [is a reason why practitioners might not explore treatment preferences]… I think that's always a factor, isn't it, in the NHS.” (Int_Radiation‐oncologist14) |
| Q32 | “We're all under pressure, we can't be spending two hours with somebody who we know that is never going to… you know, even consider participation. So perhaps that's the reason why [practitioners don't spend time exploring patient treatment preferences with all patients]… it just makes sense really, rather than to keep pushing.” (Int_Radiation‐oncologist3) |
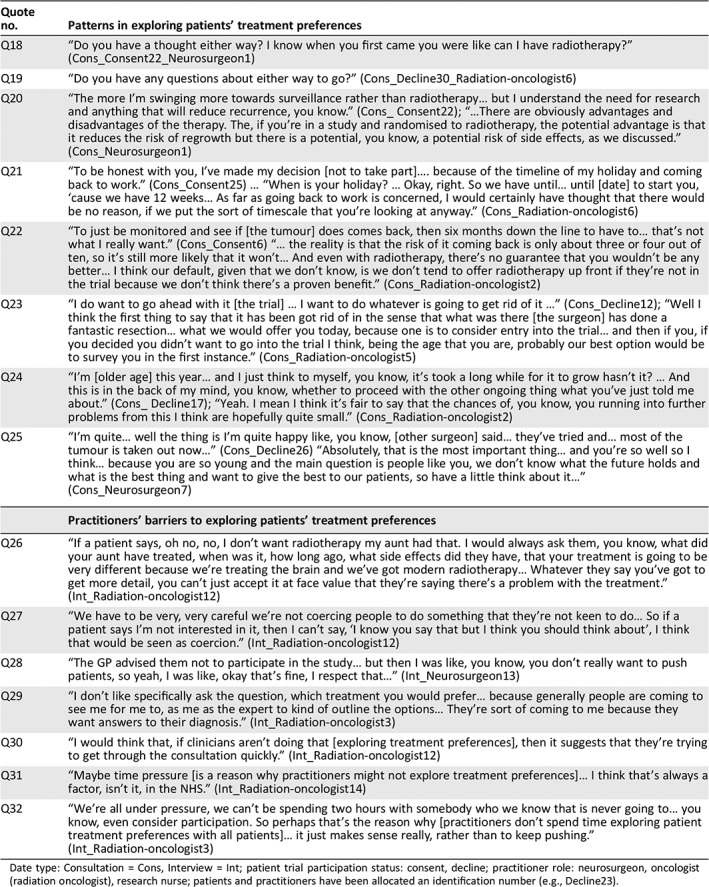
Date type: Consultation = Cons, Interview = Int; patient trial participation status: consent, decline; practitioner role: neurosurgeon, oncologist (radiation oncologist), research nurse; patients and practitioners have been allocated an identification number (e.g., Decline23).
